- Visibility 41 Views
- Downloads 10 Downloads
- DOI 10.18231/j.ijn.2019.027
-
CrossMark
- Citation
A rare case of multilocular cyst in 4th ventricle – Racemose type neurocysticercosis
- Author Details:
-
Shifa Zareena *
-
V Thanga Tirupathi Rajan
-
S Nandish.H
-
Sathish Anand.V.S
Introduction
The most important helminthic infestation of the central nervous system is the pork tapeworm causing neurocysticercosis (NCC). Neurocysticercosis has been listed as a neglected disease by the WHO.[1] About 50 million people world wide have neurocysticercosis and it causes about 50,000 deaths each year.[1] Seizure, raised intracranial pressure, neurological deficits are the most common clinical manifestations of neurocysticercosis. In developing countries, NCC is responsible for more than 50% of the cases of late onset epilepsy.[1] The National Institute of Mental Health and Neuro Sciences (NIMHANS), Bangalore reported a diagnosis of NCC in 2% of unselected series of epilepsy patients.[2] In a study from New Delhi, NCC accounted for 2.5% of all intracranial space occupying lesions.[3] The solitary form of the disease (solitary cysticercus granuloma, SCG) is the commonest presentation, reported in nearly two-thirds of all patients with NCC.[4] Between 26 and 50% of all Indian patients presenting with partial seizures are diagnosed with a SCG on the Computerised tomography scan.[2] Intraventricular cysts usually appear as solitary lesions, with the fourth ventricle being the most common site of infection (50%)[5],[6]. Racemose type of NCC is an uncommon type and it is caused by cysticercus racemosus.[7] This type is of cyst is seen in the ventricles and cisterns.[7]
Case Report
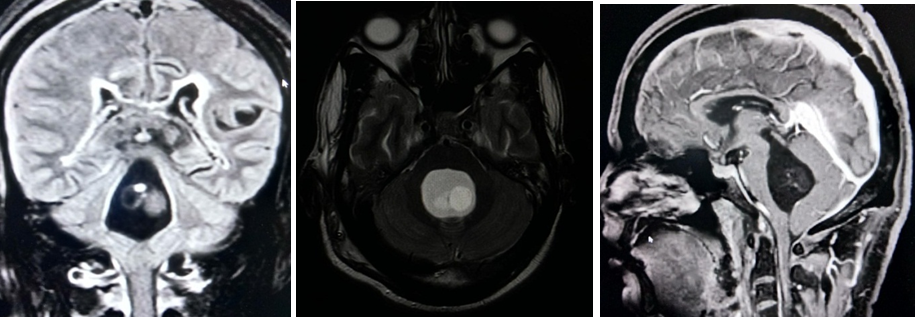
A 36 year old male, farmer by occupation, presented with persistent headache since 4 months associated with vomiting, blurring of vision and gait disturbances. He had no history of fever, seizures. No other comorbid condition. On clinical examination, he was conscious and oriented, with bilateral cerebellar signs and gait ataxia. Fundus examination revealed bilateral papilledema. Computerized tomography of brain showed dilated ventricles with cystic lesions in the fourth ventricle [Figure 1]. Complete blood examination were normal except that he was hepatitis B positive.

To relieve the obstructive hydrocephalus patient was taken up for emergency right ventriculo peritoneal shunt the same day. Cerebrospinal fluid was sent for biochemical, pathological and microbiological analysis and was found to be normal. Post operative period was uneventful. Mmagnetic Resonance Imaging brain with contrast [Figure 2] was taken which showed a well defined multicystic lesion epicentered in fourth ventricle with few non enhancing internal nodules and a small cystic lesion in the left parietal region.
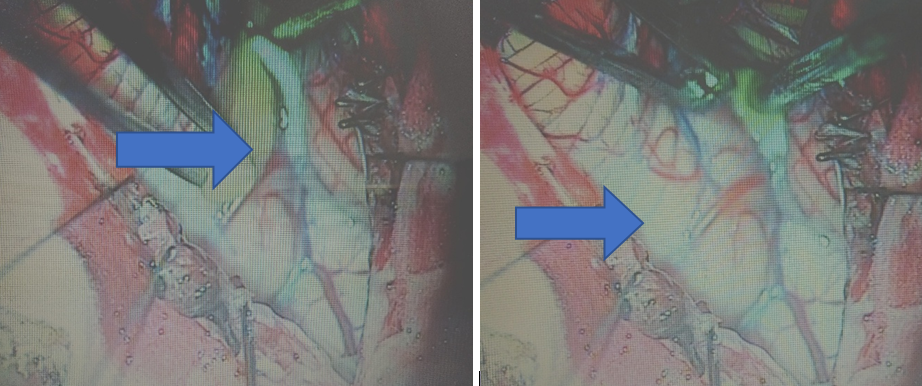
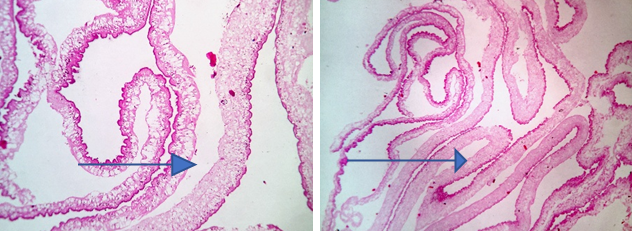
After obtaining fitness for surgery, patient underwent midline sub occipital craniectomy telovelar approach with excision of multiple fourth ventricle cyst[Figure 3],[Figure 4] Post operative period was uneventful. A post operative Computerized tomography brain showed complete excision of ventricular cysts with the shunt in situ. Post operatively patient was relieved of cerebellar signs. The cyst was sent for histopathological examination [Figure 5] which confirmed neurocysticercosis. Two weeks later p atient was started on oral antihelminthic agents.

| S.No. | Study | 4 th ventricular NCC | Racemose type 4 th ventricular NCC |
| 1 | Kar A, Biswal P, Gouda K, Mohanty P, Mohanty L, et al. 2013 | 1 | 1 |
| 2 | Divye Prakash tiwari, et.al. 2013 | 13 | |
| 3 | Poonam Mohan Shenoy et.al. 2014 | 1 | 1 |
| 4 | Saifullah Khalid,et.al. 2016 | 1 | |
| 5 | Carola Mullin et.al. 2017 | 1 | |
| 6 | Theodore E. Nash et.al. 2018 | 16 |
Discussion
Neurocysticercosis typically results from ingestion of cysticercal eggs in food contaminated by human or porcine feces. Thus, vegetarians and other people who do not eat pork can acquire cysticercosis.[8]
Dissemination in the central nervous system occurs through small capillaries into the parenchyma or through the choroid plexus into the ventricles, eventually leading to the subarachnoid space[9] and elicit inflammatory changes in the surrounding tissues.
Cysticerci may remain for a long time in this stage, protected by the blood-brain barrier and active immune-evasion mechanisms by the cysticerci.[8] Cysticerci cause symptoms because of mass effect or by blocking the circulation of cerebrospinal fluid, but most symptoms in neurocysticercosis are the direct result of the inflammatory process that accompanies cyst degeneration[8],[10] arachnoiditis and basal meningitis, or obstruction of the subarachnoid pathways of the ventricular system.[9]
Clinical presentation of neurocysticercosis can range from subclinical or subtle to epilepsy, headaches, or life-threatening manifestations.[5],[11] Seizures occur in 80% of all symptomatic neurocysticercosis cases, and other manifestations include focal neurological deficits (16%), increased intracranial pressure (12%), and cognitive decline (5%).[12] Among the reported cases of racemose type of NCC, most were confined to temporal horn and few to occipital horn of lateral ventricle.[13]
In endemic regions, recent onset of seizures in otherwise healthy teenage, young adult, or middle-aged individuals strongly suggests neurocysticercosis[12].
Intraparenchymal neurocysticercosis is more frequently associated with focal neurological signs, headaches, and seizures and accounts for 60% to 90% of all cases.[12],[14] Intraventricular cysts usually appear as solitary lesions, with the fourth ventricle being the most common site of infection and accounts for about 50%.[5],[6]
Intraventricular cysts have a more aggressive behaviour than their parenchymal counterparts. Symptoms associated with the parenchymal lesions largely result from the host’s inflammatory response to the dead or dying larva; irritation, oedema of the brain and epileptic seizures may develop.[15] If the larva settles in the subarachnoid space or ventricles, the cysticercus becomes multilocular and spreads over a wide area.[10]. These racemose cyst often causes hydrocep halus and cranial nerve palsies[10] Intraventricular cysts may become symptomatic secondary to obstruction of CSF flow, with consequent hydrocephalus and the symptoms and signs of increased ICP. Involution of the cyst will begin on antihelminthic drug administration, and the dying or dead cyst will provoke an inflammatory reaction leading to ependymitis, scarring, obstruction, and ventriculitis. Antihelminthic treatment is usually started after surgery. Hence antihelminthic agents are contraindicated in intraventricular NCC and ocular NCC prior to surgical removal of the cyst.
According to PubMed and Google scholar data search in past 10 years, solitary cysts of fourth ventricle have been reported frequently whereas racemose variety of NCC is rarely reported [Table 1] . Diagnosis of neurocysticercosis is always based upon clinical presentation, neuroimaging abnormalities and histopathological examination.[10] Complete excision of all the cysts should be done for good surgical outcome. Cerebrospinal fluid diversion may be required if a patient with fourth ventricular cyst presents in an emergency condition with obstructive hydrodephalus. Surgical excision of the cyst, relieving the cerebrospinal fluid obstruction, followed by a short course of corticosteroid administration postoperatively is the treatment for intraventricular NCC. In our case imaging study showed multilocular cysts in the fourth ventricle which post surgically was confirmed with histopathological examination. Early surgical intervention is necessary in the setting of raised intracranial pressure caused by hydrocephalus or giant cysts.
Conclusion
We conclude that in developing countries, the diagnosis of neurocysticercosis should be considered in patients presenting with neurological deficits and space occupying lesions in central nervous system even in the fourth ventricle. For cysts located on the fourth ventricle, A suboccipital craniotomy and telovelar approach remains a valid option.[16] Although solitary cysts are common, there is paucity of literatures on racemose type of NCC affecting the fourth ventricle, hence this case is reported.
Source of Funding
None.
Conflict of Interest
None.
References
- Bouteille B. Epidemiology of cysticercosis and neurocysticercosis. Med Sante Trop 2014. [Google Scholar]
- Makhale C N Wadia R.S, A V Kelkar, K B Grant. Focal epilepsy in India with special reference to lesions showing ring or disc-like enhancement on contrast computed tomography. J Neurol Neurosurg Psychiatry 1987. [Google Scholar]
- Ramesh C K Mani, G K Ahuja. Cysticercosis presenting as epilepsy. Neurol. India 1974. [Google Scholar]
- M A Wani, A Banerjee, P N Tandon. Neurocysticercosis some uncommon presentations. Neurol.India 1981. [Google Scholar]
- Kimura Hayama ET, Higuera JA, Corona Cedillo R, Chávez Macías L, Perochena A, Quiroz Rojas LY. Neurocysticercosis: radiologic-pathologic correlation. Radiographics 2010. [Google Scholar]
- J L Zhao, A Lerner, Z Shu, X J Gao, C S Zee. Imaging spectrum of neurocysticercosis. Radiol Inf Dis 2015. [Google Scholar]
- Pankaj Gupta, Manish Agrawal, V.D. Sinha, Ashok Gupta. Intraventricular racemose type neurocysticercosis with anterior interhemispheric fissure cyst: A rare case report. J Neurosci Rural Pract 2015. [Google Scholar]
- Héctor H García, Armando E Gonzalez, Carlton A W Evans, Robert H Gilman. Taenia solium cysticercosis. Lancet 2003. [Google Scholar]
- G A Alsina, J Patrick Johnson, Duncan Q Mcbride, R L Patrick, C Mark Rhoten. Spinal neurocysticercosis. Neurosurg Focus 2002. [Google Scholar]
- A Kar, P Biswal, K Gouda, P Mohanty, L Mohanty. Neurocysticercosis of 4th Ventricle-A Rare Site Encountered with Rare Presentation. J Clin Case Rep 2013. [Google Scholar]
- H H Garcia, T E Nash, Del Brutto, O H .. Clinical symptoms, diagnosis, and treatment of neurocysticercosis. Lancet Neurol 2014. [Google Scholar]
- Del Brutto OH. Neurocysticercosis: a review. Sci World J 2012. [Google Scholar]
- Jonathan A Mullins, Hugo Muniz, Osvaldo Sandoval, Luis Ramos Padilla, Carola Mullins. Neurocysticercosis of the fourth ventricle associated with hydrocephalus. Proc (Bayl Univ Med Cent) 2017. [Google Scholar]
- C Delbridge, C P Da Costa, A S Winkler. An unusual presentation of neurocysticercosis: a space-occupying lesion in the fourth ventricle associated with progressive cognitive decline. Am J Trop Med Hyg 2016. [Google Scholar]
- C Cuetter, R J Andrews. Intraventricular neurocysticercosis: 18 consecutive patients and review of the literature. Neurosurg Focus 2002. [Google Scholar]
- D Simo, J C Teixeira, A R Campos, D Coiteiro, M M Santos. Fourth ventricle neurocysticercosis: A case report. Surg Neurol Int 2018. [Google Scholar] [Crossref]
