Introduction
Extradural hematoma is seen in 1-2% cases of head injury patients. The maximum incidence is between the age of 11 to 60 years. Uncommon in young and old age in whom dura is attached to the bone firmly. It is usually a result of direct trauma and is commonly associated with overlying skull fracture though it may develop without skull fracture which is usually seen in children due to increased elasticity of bone in them.1,2 Extradural hematoma is infrequent in paediatric age group (less than 18 years) and is present in about 1-3% of all paediatric head injuries. It occurs rarely in neonates and is associated with delivery by forceps or vacuum extraction2 and fall. In infancy and the intermediate childhood period, low velocity impact (such as falls) comprise the most common mechanism of injury. Even falls from less than few feet may rarely result in EDH in this age group. Although intentional head injury in young children and infants typically causes subdural hematomas, child abuse accounts for 6-18% of EDH in some case series. In late childhood and early adolescent years, road traffic accidents are the primary cause of EDH.3,4 Though the most common source of EDH is middle meningeal artery rupture, it may also be caused by bleeding from veins, diploic vessels and dural sinuses. Posterior fossa extra dural heamatoma is of venous origin in 85% of the cases and develops as a result of injury to the transverse or sigmoid sinuses, secondary to occipital bone fracture. This study is undertaken because age itself, even within the paediatric age range, is a major independent factor affecting the mortality rate in head-injured patients having EDH.
Materials and Methods
This is a prospective analytical study conducted in a tertiary care centre in Kolkata for the period of two years. Total 47 patients were enrolled for this study collected from Neurosurgery emergency and outpatient department. All traumatic extra dural hematoma below 18 years of age of both sexes irrespective of the presence or absence of other intracranial injuries were included in this study. Non-traumatic EDH, spontaneous EDH and post neurosurgical procedure EDH were not included in the study. All patients were assessed both clinically and radiologically All data were analyzed/ interpreted at the end of study to derive all important variables which are related with the case and their effect on the outcome.
Results
Maximum number of patients in our study were in between 1-5 years (55.32%) followed by 5-18 years (38.30%) and less than 1 year (6.38%).
Table 1
| Age | No of cases | Percentage |
| Less than 1 year | 3 | 6.38 |
| 1 to 5 years | 26 | 55.32 |
| >5 years | 18 | 38.30 |
| Total | 47 | 100 |
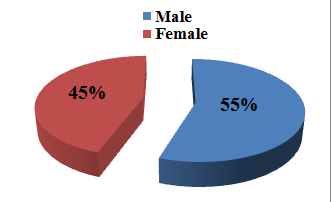
In our study out of 47 patients, 26(55.32%) were male and the rest 21(44.68%) were female. There was slight male preponderance
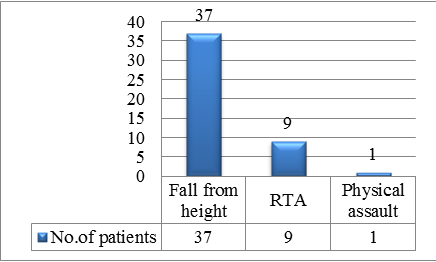
Most of the injuries in our study were found to be following, fall from height (from stairs followed by from roof and bed), following RTA and rarely physical assault.
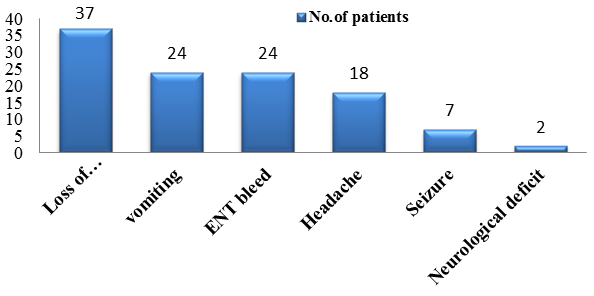
The most common presentation in our study was loss of consciousness, followed by vomiting ENT bleed, headache, seizure and focal neurological deficits.
Glasgow coma scale score assessed at the time of presentation showed, 40 patients had a score of 14-15, whereas 6 had score between 9 to 13 and the rest one had a score below 9
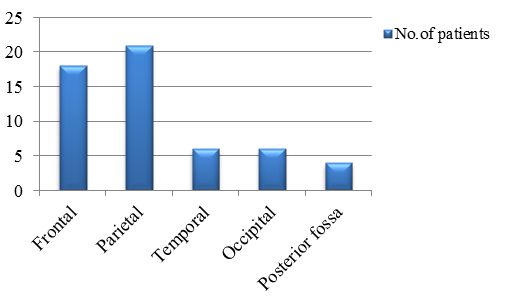
The most common location of EDH in our study was parietal region (44.68%), followed by frontal (38.29%), temporal (12.76%) and posterior fossa (6.38%).
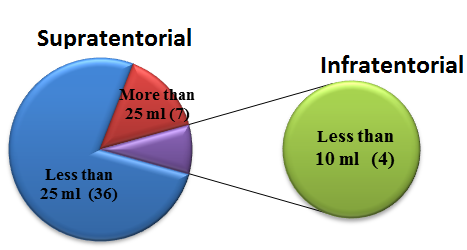
On CT scan it was seen that 7 patients (16.28%) had supratentorial hematoma of volume more than 25ml and 36 patients (83.72%) had hematoma volume less than 25ml. Four patients out of 47 had infratentorial hematoma less than 10ml. None had infratentorial hematoma more than 10ml.
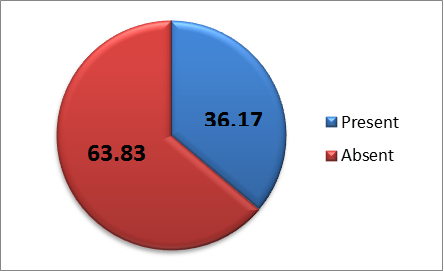
Thickness of clot seen in CT scan less than 15mm was in 40(85.10%) patients and more than 15mm was seen in 7(14.90%) patients. Midline shift was present in 17(36.17%) patients.
Brain edema was the most common associated intracranial injury in our study, followed by parenchymal contusion, pneumocephalus, subdural hematoma and subarachnoid haemorrhage
Table 3
| Nature of injury | No of patients | Percentage |
| Brain edema | 12 | 54.54 |
| Parenchymal contusion | 9 | 40.90 |
| pneumocephalus | 3 | 13.6 |
| Subarachnoid haemorrhage | 2 | 9.0 |
| Subdural hematoma | 2 | 9.0 |
Basal cistern was seen to be effaced in 5(10.64%) cases.
Table 4
| Status of basal cisterns | No of patients | Percentage |
| Effaced | 5 | 10.64 |
| Normal | 42 | 89.36 |
| Total | 47 | 100 |
Majority of the patients in our study were managed medically.
Most of the patients in our study had good recovery after both surgical as well as medical treatment.
Discussion
A cute epidural hematomas in children, and especially in infants, represent a quite rare and potentially life threatening complication resulting from head injuries. Furthermore, epidural hematomas in infants constitute a different clinical entity than the ones in adults due to their nonspecific clinical presentation and the inability of infants to communicate. The lack of any guidelines regarding the conservative treatment, appropriate management of EDH in paediatric age group is more complicated.
Mean age of presentation in our study is 8 years 3 months. Langlois J, Rutland et al5 in their study of 72 paediatric patients with traumatic head injury found maximum number of cases in between 1 year to 8 years and mean age of presentation was 10 years. In our current study slight male preponderance in incidence (55.32% male vs 44.68% female) was found.
Extradural hematoma is prevalent in young adult males with a male to female ration of 4:1 as shown by Ocrtal M et al.6 Fall from height was the most common mode of injury in our study constituting 78.72% followed by road traffic accident (19.15%) and physical assault ( 2.13%). In a study of Seeling JM et al,7 fall was the most common cause (70%) of extradural hematoma in paediatric age group.
Loss of consciousness was the most common presentation found in our study followed by vomiting, ENT bleed, seizure episode and neurological deficits. The observation of classical signs like deterioration in conscious level, hemiparesis and pupillary asymmetry, were found to be extremely important from the diagnostic point of view. However, most cases were not seen to behave in the classical way. Only five patients in our study presented with these three signs together. Jamieson and Yelland8 in their study in patients with traumatic extradural hematoma in paediatric age group also found this picture in 2.4% of their patients. The description of deterioration in consciousness level i.e concussion followed by a lucid interval followed again by unconsciousness is usually thought to be the only classical sign of extradural hematoma in a significant number of patients as shown by Mckissock et al.9 to be as high as 26% and Jamieson and Yelland8 showed it to be 12%. But it was observed in only five (10.64%) patients in our study. So the description of lucid interval as the only sign for extradural hematoma seems to be overemphasized.
The parietal area was the most common anatomical location of EDH in our study. Our findings demonstrated that anatomical location was not associated with outcome. Ersahin et al10 and pasaoglu et al.11 reported that temporo -parietal and temporal regions were the most common locations in their series. Again, no relationship between the anatomical location of EDH and the outcome was established in their study. In the current study most of the patients had good GCS score at presentation. 40(85.11%) patients presented with GCS score of 14-15; 6(12.76%) with 9-13 and 1(2.13%) with 3-8. Pang D, Horton JA, Herron JM,12 in their study found most of their patients (76.8%) presenting with GCS score.13,14,15
In this study volume of hematoma was found ranging from 8ml to 40ml and mean volume was 14.81ml. Out of 47 patients 43(91.48%) had EDH in supratentorial compartment and rest 4(8.51%) had EDH in infratentorial compartment. Of the supratentorial EDH 7(16.28%) patients had hematoma volume more than 25ml and rest 36(83.72%) had hematoma volume less than 25ml. According to one study by Mazza c, pasqualin A, Feriotti G, D apian R (1982)13, volume of hematoma upto 30ml in young age group (less than 5 years) can be compatible with survival and low morbidity. Most of the studies found a significant correlation of hematoma volume and outcome. Our study also shows similar results and all patients who had residual neurological deficits had comparatively larger hematoma volume than those who had no post treatment neurological deficits. Clot thickness was found in between 2mm to 25mm with mean clot thickness more than 15mm. Gutierrez FA et al.11 in their study found no direct correlation of clot thickness with outcome. Bezirciogle et al.14 studied 43 patients of traumatic extradural hematoma in children and concluded that clot thickness alone has no direct correlation with outcome.
The treatment of choice in the majority of acute traumatic EDHs remains to be surgical evacuation via a flap craniotomy or trephine craniotomy whenever the hematoma is causing significant mass effect. Six (12.77%) patients in our study were surgically evacuated, while 41(87.23%) were treated conservatively. Chen et al.15 suggested that a hematoma volume larger than 30ml, with thickness of more than 15mm, and a midline shift more than 5mm constitute strong indications for surgical evacuation in supratentorial compartment whereas in infratentorial compartment volume more than 10ml, clot thickness more than 10mm and midline shift of more than 5mm are surgical indications.
Conclusion
Traumatic extradural hematoma in children is an uncommon trauma sequel. Most commonly EDH in children is due to fall from height and RTA. Associated intracranial injuries are common and affect outcome. EDH volume itself does not affect the outcome if timely intervention is done. GCS score at presentation is the most important factor determining the outcome.