Introduction
Third ventricular colloid cyst constitute about 0.5%-1% of all intracranial tumors. There are several therapeutic approach suggested ranging from surgery, shunt, stereotactic aspiration.1 Due to its location in the roof of third ventricle near the foramen of Monroe, the presentation is usually is biventricular hydrocephalus.2 The advantage of excellent visualization and minimally invasive corridor through the dilated ventricular system makes endoscopic excision as the preferred treatment of choice in current scenario.3
In this paper we present our preliminary experience of five consecutive cases of colloid cysts operated using endoscopic approach.
Materials and Methods
Five cases of colloid cysts were operated in Department of Neurosurgery, J. N. Medical College, Aligarh Muslim University between July 2017 to June 2019. The age of the patient was between 8 years and 60 years.
After taking informed consent all patients underwent endoscopic surgery. We have used Karl Storz lotta hopkins ventriculo scope with wide angled telescope 6 degree, 2.6mm instrument channel and irrigation and suction channel 1.6mm. with high definition camera. Continuous irrigation is done with Ringer’s Lactate .
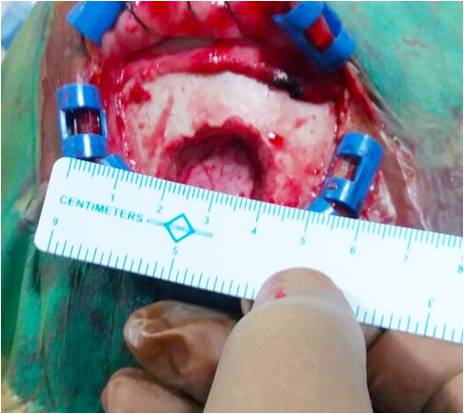
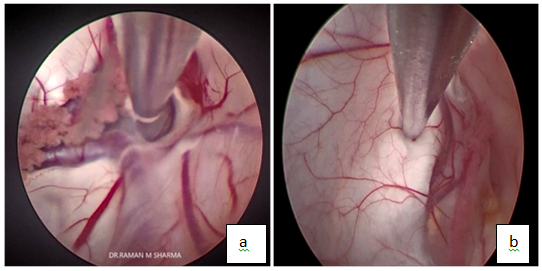
All patient were operated under general anaesthesia. Patients were positioned supine on horse shoe with head end elevated at 30 degrees. Burr hole was made 4cm lateral to midline and 3 cm anterior to the coronal suture Figure 1. All patient had moderate to severe hydrocephalus, henceforth free hand technique was used to insert the trocar in all the cases. After checking the ventricular entry zero degree endoscope was inserted and irrigation was started. Anatomy around the foramen of Monroe was carefully defined. Shape of the foramen along with its relationship with Septal and thalamic vein is also defined.Figure 2
According to the size of the foramen of Monroe and its type two major approach were used (1) Transforaminal Approach (2) Trans- Septal Approach.Figure 3.
In the transforaminal Approach the foramen is wide and cyst can be seen through the foramen. The cyst wall is coagulated with monopolar along with the feeder arterioles. The cyst wall is cut with a knife and contents are aspirated. Gradual removal of pieces is required with a grasper if the contents are very thick or viscous, in one of the case the content was calcified2. Occasionally a fogarthy is inserted and inflated tinside the cavity to widen the opening and press the content out. Once the cyst is decompressed the wall is removed after holding it with biopsy forceps and rotatry movement, piecemeal excision of the cyst wall is preferred. If there is residual cyst wall it is coagulated with bipolar to make it shrink to a very small tissue. Adequate Cerebrospinal fluif (CSF) flow was confirmed at the end of procedure Figure 5
In transseptal approach the cyst wall is approached just the anterior or posterior to the septal vein. The same principal of coagulating the cyst wall and aspiration of the cyst content were applied.
Inadverent bleeding was managed with continuous irrigation. If there is bleed from the choroid plexus a tamponade can be applied by 3 French Fogarthy catheter Figure 5. Hemostasis is ensured by cauterization of both inner and outer surface of the cyst wall Figure 5.
At the end of the procedure third ventriculostomy was done in all the case to prevent postoperative blockage of CSF flow by debris and the blood Figure Figure 5.
Results
Overall five patients of colloid cyst were successfully managed. The youngest patient was 8 year old child and the oldest was 60 years old. Three patients were male two patients were female. Of all five cases three cases presented with intermittent headache associated with blurring of vision and vomiting. One patient had history of drop attacks and headache. One patient has presented with urinary incontinence and walking difficulty. Three patients had colloid cyst measuring more than 2.5cm and two were less than 2.5cm.
The operative time ranges between 180 minutes to 240 minutes. The type of cyst and the foraminal anatomy defined the approach Figure 3. Three patients underwent transseptal or combined approach, two patient underwent transforaminal approach. Gross total excision could be achieved in three patients, two patients had partial excision. Content of the cyst is varied from viscous content, thick and in one of our case the content of collid cyst was calcified Figure 4.
Two cases had mild to moderate intraventricular hemorrage which required postoperative extraventricular drainage of cerebrospinal fluid (CSF), which was removed within 48-72 hours. One case required postoperative ventriculoperitoneal shunt placement. One patient had transient altered sensorium which improved gradually.
We have a mean followup of 7 months 14 days (range 3mont to 550 days). There was no radiological evidence of recurrence in any of our patient Figure 6. All patient return back to their work after an average of 78 days following discharge.
Discussion
The velum interpositum is most likely the site of origin of colloid cyst. They are the slow growing tumors and causes gradual obstruction of the foramen Monroe and hydrocephalus. Because of the enlarged ventricule size and foramen of Monroe these lesion deemed good for neuroendoscopic excision. The cyst either can grow anteriorly which may cause a larger foramen of Monroe and cyst growing in to the lateral ventricle. Such cases are handeled preferably with the direct transforaminal approach.
Figure 2
Foramen Monroe Endoscopic Anatomy with relation to the surrounding structure (a) large foramen monroe with related structure (b) large but difficult area of entry (c) coapted type with very small foramen with cyst bulging in the lateral ventricle (d) crescentric type foramen with choroid plexus covering the colloid cyst (e) displayed type in which foramen is totally closed and cyst is displayed into the lateral ventricle (f) image awaited
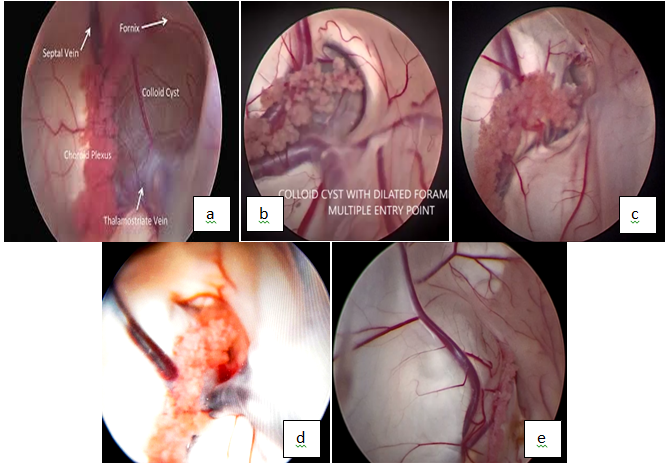
Figure 4
Type of the content (a): Calcified colloid cyst content removed with grasper and excising the cyst wall (b): Viscous content aspirated with suction tip (c): Thick content removed piecemeal with grasper and suction
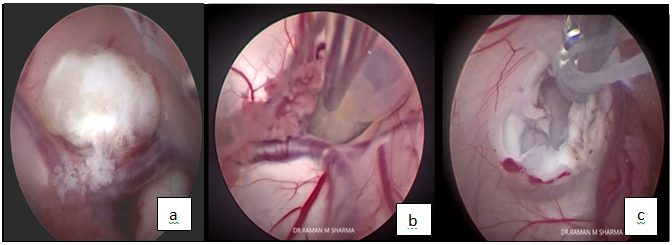
Figure 5
(a): Achieving hemostasis with tamponade by the fogarthy bulb inflation withinin the foramen monroe (b): Establishment of the Cerebrospinal fluid flow after excision of the coloid cyst after transseptal approach (c): Cauterization of both inner and outer surface of the cyst wall; (d): Third ventriculostomy at the end of procedure
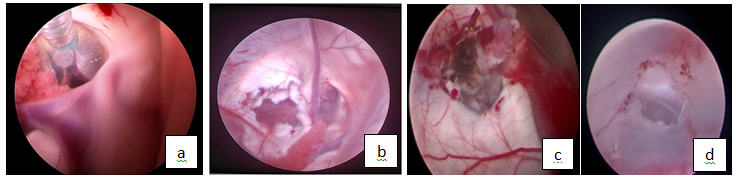
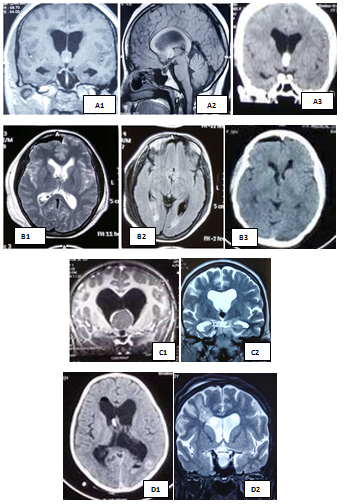
Figure 6
Preoperative and postoperative radiological evaluation (a) A-1 ,2 ,3 Foraminal type of colloid cyst with normal sized third ventricle B-1,2,3 Postoperative scan (b) Coapted and displayed type C1,2; and D1,2; are the postoperative scan of the corresponding patients
A cyst growing more posteriorly tends to go medial to the septum pellucidum leading to narrowing of foramen of Monroe. It also leads to widening of interforniceal space and displaces the fornices. Mac Millan described coappted and displayed type of Foramen in such patients. In these cases transforaminal approach is not possible. Aspiration of the cyst content posteriorly and away from the fornices will lead to opening of the foramen of Monroe and subsequent excision of the cyst by transforaminal route. Thus conversion to the microsurgical approach unnecessary. In three of our cases we had to do transseptal approach.4
There is a constant debate regarding more incidence of colloid cyst wall residue in endoscopic approach as compared to microsurgical excision. Howsoever there are several studies that suggest that that subtotal resection with cyst coagulation may be sufficient and comparable to microsurgical removal. Hoffman et al in 2017 suggested that residual cyst having high recurrence of 33.3% and the aim of the aim of the surgery to be complete excision.5 In our series we had two cases in which we could not completely excise the cyst wall. In one of the cases there was torrential bleeding while sepearating the cyst wall from the choroid plexus. We could not excise the colloid cyst wall completely. In this case we have coagulated the wall to shrunk it a small size. Third ventriculostomy and septostomy was done in this patient and extraventricular drain was kept in the postoperative period. Subsequently patient required ventriculoperitoneal shunt for symptomatic hydrocephalus. Both these cases are in followup without any fresh symptoms though the follow up is less than one year. It is to be acknowledge that there is definitive learning curve associated with endoscopic management of intraventricular tumour. It is our initial experience, with the advent of better endoscopic equipment and various endoscopic manoeuvre the excision rates are getting better. We attempt to perform the gross total excision all the case. However we opine that unnecessary traction and manuovere to achieve this goal can lead to uncontrollable bleeding sometime. Good opening of the cyst wall, adequate removal of content and septostomy is recommended in such cases. Biventricular technique has been suggested as a good technique for radical excision.2