- Visibility 266 Views
- Downloads 69 Downloads
- Permissions
- DOI 10.18231/j.ijn.2024.036
-
CrossMark
- Citation
Intravenous thrombolysis in acute Hemi-chorea hemi-ballismus syndrome
- Author Details:
-
Gaurav Shah *
Abstract
Hyperkinetic movement disorders of acute onset are rare manifestation of acute ischemic stroke.
They are believed to be due to lesion in basal ganglia specifically to sub thalamic nuclei. Intravenous thrombolysis in this cases can prevent major disability. Here is a case of a 32 years old lady who had sudden onset of involuntary movements of left upper and lower limb with weakness of left side of the body. She was brought to the hospital within one hour of onset of her symptoms. Her vitals, blood sugars and CT brain plain was normal. Intravenous thrombolysis was done. She had complete resolution of symptoms in next 48 hours. MRI brain with angiography infarct in right caudate, putamen and anterior limb of internal capsule, M1 segment stenosis of right middle cerebral artery for which she was referred for carotid revascularization. Thus early identification and prompt treatment helps in prevention of disability.
Introduction
Acute ischemic stroke can present with variety of negative symptoms like facial drooping, vision loss, limb weakness or numbness of limbs. Positive symptoms like hyperkinetic movement disorders are rare, in particular hemi-chorea hemi-ballismus syndrome which occur in less than 1% of cases.Hemichorea manifests as spontaneous, dance-like movements affecting the limbs and head, with a higher frequency observed in distal body parts compared to proximal ones.[1] Typically, contralateral involvement of the subthalamic nucleus/basal ganglia is observed in this particular movement disorder. [2]
Case Report
A 32-year-old lady with no previous comorbidities, had sudden onset left upper and lower limb involuntary movements of 1-hour duration, these movements were repetitive, non-stereotypical in nature with no suppressibility involving proximal and distal part of the limbs. She also had difficulty in speech and difficulty in walking. On examination, she was conscious, cooperative, her vitals were stable blood sugar levels were normal. Pupils were normal and reactive to light, left upper motor type of facial palsy was seen, left upper and lower limb showed flinging movements and choreiform movements in both left upper and lower limb. The power of left upper and lower limb was 4/5 MRC grade with left plantar extensor in nature. Sensory system was intact. CT brain plain showed no abnormality.(Alberta stroke programme early CT score-10).([Figure 1])

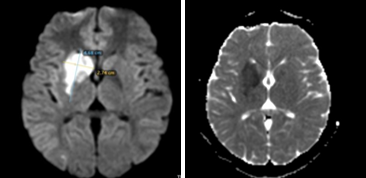
The procedure was uneventful, MRI brain with angiography done after 24 hours of thrombolysis showed infarct in right basal ganglia and internal capsule, M1 segment of right middle cerebral artery was stenosed. She was started on dual antiplatelets and statin. Other investigations including Hba1c, lipid profile, serum ceruloplasmin, serum ANA, ANCA, APLA profile, homocysteine and viral markers were negative. In next 48 hours she had resolution of symptoms.([Figure 2], [Figure 3])

Discussion
Acute ischemic stroke presenting with hyperkinetic movement disorder is rare. [3] Less than 1% develop acute or delayed movement disorder complication. In a review various movement disorder were found in stroke including Ballismus, chorea, dystonia, tics, asterixsis, myoclonus, parkinsonism among others.[4] Hemiballismus-hemichorea syndrome is particularly common movement disorder among stroke around 40% of cases. [3] Chorea consists random, dancelike movements of parts of body which are imperisistent.[5] Hemiballism is large amplitude movements involuntary movements of the limbs on one side of the body. Vidakovic et al described 19 patients with hemiballism of 25 total cases of ballismus. Majority of them were secondary to infarct in brain and age of onset was 66 years. [6]
Contralateral subthalamic nucleus (STn) lesion is most common cause for this phenomenology. [3] Chung et al showed basal ganglis (STn, caudate, putamen) and cortical lesions contralateral to the affected side on MRI. [7] Hemiballism is closely associated with these lesions. [4] Transient ischemic attack can also cause Hemichorea symptoms. [8] It has also been described in MRI brain negative lesion presenting in large vessel disease on angiography which subsided the symptom on treating the stenosis. [9] Structures outside basal ganglia have also been described to cause chorea particularly parietal lobe involvement. [10] The mechanism for chorea outside basal ganglia lesion is probably due to involvement of striatal fibers from parietal lobe. [11]
The other causes of chorea in acute setting include any underlying Autoimmune disorders like Systemic Lupus Erythematosus, anti-phospholipid antibody syndrome, para proteinemic vasculitis, Sydenham chorea. [12] The another important cause of acute onset chorea is hyperglycemic chorea. [13]
Two case report for use of thrombolysis in acute HCHB syndrome. [14], [15] where there was almost resolution of symptoms was seen and a case of acute onset Choreoathetosis and weakness was successfully treated with thrombolysis followed by thrombectomy. [16]
Outcome of HC-HB is generally good and it depends on site of lesion. Hemichorea-hemiballismus due to parietal lobe lesion resolves completely whereas basal ganglia involvement causes complete resolution in 50% of cases. Typical neuroleptics like haloperidol are used in treatment. Atypical neuroleptics can also help with less side effects than typical neuroleptic drugs. Drugs with other mechanisms with efficacy include tetrabenazine, reserpine, benzodiazepines, sodium valproate, gabapentin, and Topirmate. [17], [18]
Conclusion
Hemi-ballismus hemi chorea syndrome is a rare manifestation of acute ischemic stroke. It’s earliest detection and intervention can reduce major disability.
Abbreviations
CT-Computed Tomography, MRI- Magnetic Resonance Imaging, STn- subthalamic nuclei, MRC-medical research council, HCHB- Hemichorea hemiballismus Syndrome.
Source of Funding
None.
Conflict of Interest
None.
Acknowledgement
Dr Ram Pansuriya, MD (Radiology), Pooja diagnostic and Imaging center for MRI brain and carotid angiography images.
References
- Cardoso F, Seppi K, Mair K, Wenning G, Poewe W. Seminar on choreas. Lancet Neurol. 2006;5(7):589-602. [Google Scholar]
- Pinsker J, Shalileh K, Rooks V, Pinsker R. Hemichorea-hemiballism secondary to non-ketotic hyperglycemia. J Clin Med Res. 2015;7(9):729-30. [Google Scholar]
- Ghika-Schmid F, Ghika J, Regli F. Hyperkinetic movement disorders during and after acute stroke: the Lausanne Stroke Registry. J Neurol Sci. 1997;146(2):109-16. [Google Scholar]
- Bansil S, Prakash N, Kaye J, Wrigley S, Manata C, Stevens-Haas C. Movement Disorders after Stroke in Adults: A Review. Tremor Other Hyperkinet Mov (N Y). 2012;2. [Google Scholar] [Crossref]
- Ristic A, Marinkovic J, Dragasevic N, Stanisavljevic D, Kostic V. Long-term prognosis of vascular hemiballismus. Stroke. 2002;33(8):2109-11. [Google Scholar]
- Vidakovic A, Dragasevic N, Kostic VS. Hemiballism: Report of 25 cases. J Neurol Neurosurg Psychiatry. 1994;57(8):945-9. [Google Scholar]
- Chung S, Im J, Lee M, Kim J. Hemichorea after stroke: Clinical-radiological correlation. J Neurol. 2004;251(6):725-9. [Google Scholar]
- Nedelmann M, Kolbe M, Angermueller D, Franzen W, Gizewski E. Cerebral hemodynamic failure presenting as limb-shaking transient ischemic attacks. Case Rep Neurol. 2011;3(1):97-102. [Google Scholar]
- Su H, Cao Q, Sun G, Xu Y, Ying T. Hemichorea without MRI findings accompanied by significant internal carotid artery stenosis: A case report. Neurol Asia. 2022;27(2):489-91. [Google Scholar]
- Strauss S, Rafie D, Nimma A, Romero R, Hanna P. Pure Cortical Stroke Causing Hemichorea-Hemiballismus. J Stroke Cerebrovasc Dis. 2019;28(10). [Google Scholar] [Crossref]
- Patel A, Patel A, Desai S. Acute Hemiballismus as the Presenting Feature of Parietal Lobe Infarction. Cureus. 2019;11(5). [Google Scholar] [Crossref]
- Orzechowski N, Wolanskyj A, Ahlskog J. Antiphospholipid antibody-associated chorea. J Rheumatol. 2008;35(11):2165-70. [Google Scholar]
- Wintermark M, Fischbein N, Mukherjee P, Yuh E, Dillon W. Unilateral putaminal CT, MR, and diffusion abnormalities secondary to nonketotic hyperglycemia in the setting of acute neurologic symptoms mimicking stroke. AJNR Am J Neuroradiol. 2004;25(6):975-6. [Google Scholar]
- Mccollum D, Silvers S, Dawson S, Barrett K. Resolution of acute onset hemichorea-hemiballismus after treatment with intravenous tissue plasminogen activator. Neurohospitalist. 2013;3(3):131-4. [Google Scholar]
- Zidverc-Trajković J, Jovanović D, Marjanović I, Radojičić A, Beslać-Bumbaširević L. Successful intravenous thrombolysis in a stroke patient with hemiballism. Neurologist. 2011;17(4):205-7. [Google Scholar]
- Muhammad A, Bielskute E, Guyler P, Grunwald I. Acute ischaemic stroke-related choreoathetosis treated with arterial thrombectomy. BMJ Case Rep. 2019;12(1). [Google Scholar] [Crossref]
- Handley A, Medcalf P, Hellier K, Dutta D. Movement disorders after stroke. Age Ageing. 2009;38(3):260-6. [Google Scholar]
- Dewey R, Jankovic J. Hemiballism-hemichorea: clinical and pharmacologic findings in 21 patients. Arch Neurol. 1989;46(8):862-7. [Google Scholar]
How to Cite This Article
Vancouver
Shah G. Intravenous thrombolysis in acute Hemi-chorea hemi-ballismus syndrome [Internet]. IP Indian J Neurosci. 2024 [cited 2025 Oct 28];10(3):168-170. Available from: https://doi.org/10.18231/j.ijn.2024.036
APA
Shah, G. (2024). Intravenous thrombolysis in acute Hemi-chorea hemi-ballismus syndrome. IP Indian J Neurosci, 10(3), 168-170. https://doi.org/10.18231/j.ijn.2024.036
MLA
Shah, Gaurav. "Intravenous thrombolysis in acute Hemi-chorea hemi-ballismus syndrome." IP Indian J Neurosci, vol. 10, no. 3, 2024, pp. 168-170. https://doi.org/10.18231/j.ijn.2024.036
Chicago
Shah, G.. "Intravenous thrombolysis in acute Hemi-chorea hemi-ballismus syndrome." IP Indian J Neurosci 10, no. 3 (2024): 168-170. https://doi.org/10.18231/j.ijn.2024.036
