Introduction
Systemic lupus erythematosus (SLE) is an autoimmune, multi system chronic inflammatory disease of the connective tissue.1 Neuropsychiatric SLE (NPSLE) refers to series of complex and heterogeneous neurological and psychiatric symptoms directly related to SLE.2 However golden standard for diagnosis of NPSLE is lacking and different approaches like multidisciplinary assessment are used for clinical diagnosis. 3 The presence of neuropsychiatric symptoms is a serious indicator of severe course and poor prognosis in patients with SLE. 1 Herein we report a case of NPSLE, a relatively less common and severe form of SLE.
Case Report
An 18 year old adolescent female patient was referred from district level hospital for further management. She was admitted with complaint of diarrhea there for 5 days. She developed generalized convulsion, two episodes, for which she was referred to our hospital. On admission she was conscious, vitals were stable and except for brisk deep tendon reflexes rest of neurological examination was normal. Her general examination revealed presence of malar rash over face, alopecia, oral ulcers and mild hepatomegaly. She had complaint of headache and joint pain intermittently since 5 to 6 month. There was no history suggestive of Raynaud's phenomenon. There was no past history of any drug ingestion.
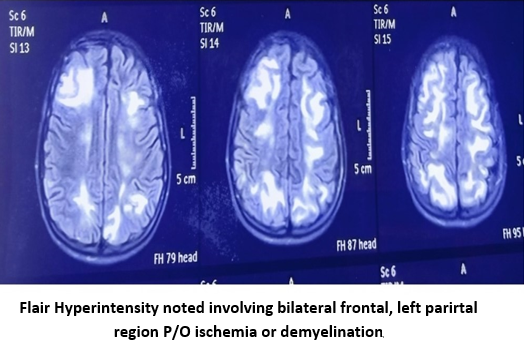
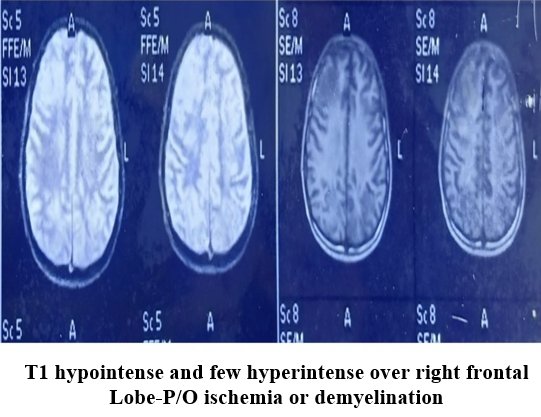
Her CBC report showed Hemoglobin 12 Gm/dl, TLC 13000/cmm, Platelet count 1,20,000/cmm. LFT showed mildly elevated hepatic enzymes (SGPT 60 U/L, SGOT 51 U/L). RBS, S calcium, S electrolytes, RFT, CSF examination and X- Ray chest was normal. Urine Protein/ Creatinine ratio was 3.82. There was no hematuria, RBC cast on urine routine examination. ESR was 6 mm/hour.ANA profile was +3 with homogenous pattern. Anti -DS DNA antibodies were positive. ANA immunoblot test showed specific bands for RNP -SM & Ribosomal Protein strongly positive; SM & Histone band positive and Nuclosome band borderline positive. Anti phospholipid (APL) IgG & IgM was negative. Direct Coomb's test (DCT) was +3. Her lipid profile showed Cholesterol 126 mg/dl, Triglyceride 222 mg/dl, HDL 32 and LDL 100 mg/dl. MRI Brain showed diffuse bilateral symmetrical patchy hyper intensities in cortical and sub cortical areas of cerebral cortex and cerebellum on T2 and Flair images suggestive of ischemia/ demyelination. EEG was not done due to unavailability of bedside EEG facility.
On basis of clinical features and lab reports diagnosis of SLE was made. Since the patient had neurological symptom neuropsychiatric SLE (NPSLE) was considered. Patient was started with Methylprednisolone (pulse therapy) 30 mg/kg daily for 5 days followed by oral prednisolone (2mg/kg/day) and oral Hydroxychloroquine (HCQ) 5 mg/kg/day. She received injection phenytoin, injection Phenobarbitone, injection levetirecetam and injection sodium valproate as per standard dose for control of her seizures. Nephrologists' opinion was taken as her urine Protein/Creatinine ratio was high and she was started with intravenous Cyclophosphamide according to Euro- Lupus regimen on 3rd day of admission i.e. injection cyclophosphamide intravenously 500 mg every 2 week for 6 doses.
She had multiple episode of generalized seizure in spite of giving four anticonvulsants. She was found to have behavioral symptoms in form of vacant look, irrelevant talk and confusion from 5th day of admission onwards. A psychiatric consultation was done for her behavioral symptoms, however she was not prescribed any medication for that.
On 15th day of admission she developed fever and respiratory distress. Repeat blood count showed neutropenia (WBC 3000/cmm) and thrombocytopenia (platelet count 35000/cmm). X- Ray chest showed consolidation. In view of fever with severe neutropenia she was put on broad spectrum antibiotics. Her condition was worsening gradually in spite of giving higher antibiotic, antifungal and ventilator support and she died on 30th day of hospitalization.
Discussion
SLE is a multisystem autoimmune disease having broad spectrum of clinical manifestations and several immune abnormalities leading to multi organ dysfunction. The 2019 European League against Rheumatism/American College of Rheumatology classification criteria for SLE include at least one positive antinuclear antibody (ANA) test as a mandatory entry criterion, followed by additive weighted standards grouped in seven clinical (Constitutional, hematological, neuropsychiatric, serosal, musculoskeletal, renal, and mucocutaneous) and three immunological (antiphospholipid antibodies, complement proteins, and SLE‐specific antibodies) domains weighted from 2 to 10, with patients accumulating ≥10 points being diagnosed with SLE.4, 5 The reported prevalence of NPSLE range from 39% - 50% in different studies.2 It is more frequently reported in Africans and Asians as compared to white individuals and in women mainly in childbearing age.1 NPSLE can be focal or diffuse and clinical manifestation ranges from subtle cognitive dysfunction to acute confusion state, seizure disorder and psychosis.2 Headache, anxiety, mood and cognitive disorder are the most frequent neuropsychiatric manifestation.2, 6, 7 The diagnosis of NPSLE lacks specific criteria and it is done by excluding other common causes like metabolic, infective, drug or toxin related encephalitis.2 American college of Rheumatology (ACR) nomenclature and case definition for NPSLE suggested criteria, which are divided into two groups:
First group- Seizure psychosis, cerebro-vascular event, cranial nerve lesion, quantitative alteration of consciousness. Second group - Cognitive dysfunction, lupus headache, peripheral neuropathy, MRI changes, EEG changes, ENMG changes, positive aRPA, positive aPL.
The presence of at least one criterion from the first group and at least two criteria from second group is sufficient to make final diagnosis of NPSLE. 1, 8
Our patient had mucocutaneous involvement in form of malar rash, oral ulcers; renal involvement in form of proteinuria, strongly positive ANA, thus fulfilling the 2019 European League Against Rheumatism (EULAR) / ACR classification criteria for diagnosis of SLE. Further our patient had seizures, headache, confusion and MRI changes, thus fulfilling the criteria for diagnosis of NPSLE.
The management of NPSLE is challenging and some of the therapies are empirical due to lack of controlled clinical trials. Treatment is mainly focused on symptomatic treatment such as antiepileptic for seizure, anxiolytics/ antipsychotics for psychiatric symptoms, antihypertensives if blood pressure is high and correction of metabolic abnormality along with drugs to halt inflammation driven syndrome. 2 Intravenous cyclophosphamide and oral prednisolone are the only agents tested in NPSLE with positive results.2, 9 Our patient was started with immunosuppresant corticosteroid along with cyclophosphamide and symptomatic treatment.
NPSLE is associated with worse prognosis. Previous research indicated up to nine fold increased mortality in NPSLE as compared to general population. 2, 10, 11 The main contributors to mortality are infections, cardiovascular disease and renal involvement. 5 Our patient developed pneumonia and severe sepsis which was the cause of death. Monahan et al also found increased risk of death due to infections compared to general population. 3
Conclusion
A multidisciplinary effort is needed in both diagnosis and treatment of NPSLE in absence of specific diagnostic biomarker and limited management guidelines. Infections are the major cause of death. The potential increased risk of infection secondary to immunosuppressive treatment poses a challenge to manage such patients.