- Visibility 51 Views
- Downloads 16 Downloads
- DOI 10.18231/j.ijn.2024.017
-
CrossMark
- Citation
Economic assessment of convulsive status epilepticus: Investigating socioeconomic correlations in hospitalization costs and outcomes in Northern India
Introduction
Convulsive Status Epilepticus (CSE) presents a significant health burden globally, particularly in regions with limited access to healthcare resources and socioeconomic disparities. It is defined as continuous or repetitive seizures without regaining consciousness between seizures, CSE requires prompt medical intervention to prevent complications and reduce mortality rates.[1] However, beyond its clinical implications, CSE also imposes substantial economic strain on patients and their families, especially in resource-limited settings where healthcare costs can exacerbate financial vulnerabilities.[2]
The economic impact of epilepsy, including CSE, has been studied in various contexts worldwide, highlighting the multifaceted challenges faced by affected individuals and healthcare systems.[3] In low- and middle-income countries (LMICs), where epilepsy prevalence is often higher and access to healthcare resources is limited, the economic burden of the condition can be particularly severe.[4] Factors such as out-of-pocket healthcare expenses, loss of productivity due to disability, and social stigma further compound the financial challenges faced by individuals living with epilepsy in these settings.[5]
Northern India, with its dense population and diverse socioeconomic landscape, represents a pertinent context for examining the economic impact of CSE. Despite the region's significant burden of epilepsy, studies focusing specifically on the economic consequences of CSE and its implications for affected individuals' financial well-being are scarce. Understanding the economic dynamics of CSE in this region is crucial for informing policy interventions and healthcare strategies aimed at reducing the burden of epilepsy and improving access to quality care.
This study is one of a kind in the North Indian Subcontinent as it evaluates the relationship between socio-economic status and the cost of hospital stay, as well as clinical outcomes, in patients with Convulsive Status Epilepticus. Prior research has assessed factors that can predict the expense of status epilepticus and the patterns of expenditure of individuals with epilepsy.[6], [7]
This study aims to address this gap by assessing the economic impact of CSE in Northern India, focusing on hospital costs and the financial strain experienced by patients and their family members. By analyzing data from patients presenting with CSE, including hospitalization expenses, income status, and the Kuppuswamy socioeconomic scale, the present study seeks to elucidate the associations between socioeconomic factors and clinical outcomes. Through this study, the aim of this study is to provide insights that can inform targeted interventions to alleviate economic strain and enhance access to healthcare services for individuals affected by CSE in Northern India.
Materials and Methods
This observational study was conducted at Jawaharlal Nehru Medical College, Aligarh Muslim University (AMU), Aligarh, India, from September 2020 to October 2022.
Patient selection
Inclusion criteria
All patients who presented with convulsive status epilepticus (CSE), that is, patients presenting with continuous or repetitive seizures without regaining consciousness for more than 5 minutes were included in the study.
Exclusion criteria
Patients with a history of traumatic head injury, eclampsia, brain tumour, or those who declined to provide consent were excluded from the study.
Ethical considerations
The protocol of this study was approved by the Institutional Ethics Committee of Jawaharlal Nehru Medical College, AMU, Aligarh. The study was done in accordance with the principles of Good Clinical Practice and the Helsinki Declaration.
Data collection
Patients diagnosed with convulsive status epilepticus were identified upon admission to the hospital. After taking informed consent demographic information, including age, gender, and residence, that is, rural or urban, was recorded for each patient in Microsoft Excel 2019 spreadsheet. Furthermore, the following variables were recorded through a questionnaire and subsequently entered into Microsoft Excel
Length of Hospital Stay: The duration of hospitalization for each patient was noted from the date of admission to the date of discharge or transfer.
Total monthly income of the family: The income level of the patient's family was assessed using self-reported data or available financial records and graded according to Kuppuswamy classification 2021 from a score of 1 to 12 ([Table 1]).[8]
Education of the Head of the family: The educational attainment of family members, particularly the head of the family, was recorded using a questionnaire and scored from a score of 1 to 7 ([Table 1]).
Occupation of the Head of the family: The occupation of the head of the family was categorized according to the Kuppuswamy Scale and scored from a score of 1 to 10 ([Table 1]).
Kuppuswamy Socioeconomic Scale: Using the Modified Kuppuswamy socioeconomic scale updated for the year 2021, the socioeconomic status of the patients' family was analysed and recorded using a questionnaire ([Table 1]).[8], [9]
Estimated Total Cost During Hospital Stay: The total cost incurred during the hospital stay, including expenses related to medical treatment, investigations, and ancillary services, was calculated for each patient and noted in Indian Rupees.
Other parameters, that is, presence of acute symptomatic leading to hospital admission, Estimated Cost of medication in previous year in patients who were already on antiepileptic drug therapy and poor Financial Condition leading to Drug Default were documented and entered in a Microsoft Excel 2019 spreadsheet.
Patient Management: The management of all patients followed the established guidelines of the International League against Epilepsy for the management of status epilepticus.[10]
Outcome assessment
The primary outcome measure was the association between socioeconomic factors and clinical outcomes in patients with convulsive status epilepticus. Poor outcome was defined as death of the patient or discharged from the hospital but with remaining neurological deficit. Good outcome was defined as being discharged from hospital without any neurological deficit.
Statistical analysis
The presentation of the Categorical variables was done in the form of number and percentage (%). On the other hand, the quantitative data with normal distribution were presented as the means ± SD and the data with non-normal distribution as median with 25th and 75th percentiles (interquartile range). The data normality was checked by using Shapiro-Wilk test. The cases in which the data was not normal, we used non parametric tests. The following statistical tests were applied for the results: 1. The association of the variables which were quantitative and not normally distributed in nature were analysed using Mann-Whitney Test and variables which were quantitative and normally distributed in nature were analysed using Independent t test. 2. The association of the variables which were qualitative in nature were analysed using Chi-Square test. If any cell had an expected value of less than 5 then Fisher’s exact test was used. 3. Receiver operating curve was used to find out cut off point, sensitivity and specificity of individual components scores of Modified Kuppuswamy Socio-economic Scale, that is, total monthly income of the family score, education of the head of the family score, occupation of the head of the family score and Kuppuswamy Socioeconomic Class. 4. Univariate logistic regression was used to find out odds ratio with 95% CI for predicting risk of poor outcome. The data entry was done in the Microsoft EXCEL spreadsheet and the final analysis was done with the use of Statistical Package for Social Sciences (SPSS) software, IBM manufacturer, Chicago, USA, ver 25.0. For statistical significance, p value of less than 0.05 was considered statistically significant.
Results
The study enrolled a total of 110 patients diagnosed with Convulsive Status Epilepticus (CSE) at Jawaharlal Nehru Medical College, AMU, Aligarh, from September 2020 to October 2021. The demographic and clinical characteristics of the patients, as well as their association with outcomes, are summarized in [Table 2].
Demographic parameters and clinical outcome
The mean age of patients under study was 35.8 ± 18.0 years. 59.1% (n= 65) of the patients were males and 40.9 % (n=45) were females. There was no significant association observed between age and gender with poor outcome (p=0.466, p=0.447 respectively). 50.9% (n=56) of patients were from rural areas and 49.1% (n=54) were from urban areas and no significant association was observed between resident status of patients and Outcome (OR 0.667 95% CI 0.291 - 1.526, p=0.450) ([Table 2]).
Socio-economic parameters and clinical outcome
Socio-economic Parameters were assessed using Modified Kuppuswamy Socio-economic status 2021 and its components, that is, occupation of the head of the family, total income of the family updated as per 2021, education of the head of the family and Kuppuswamy Socio-economic status scale.
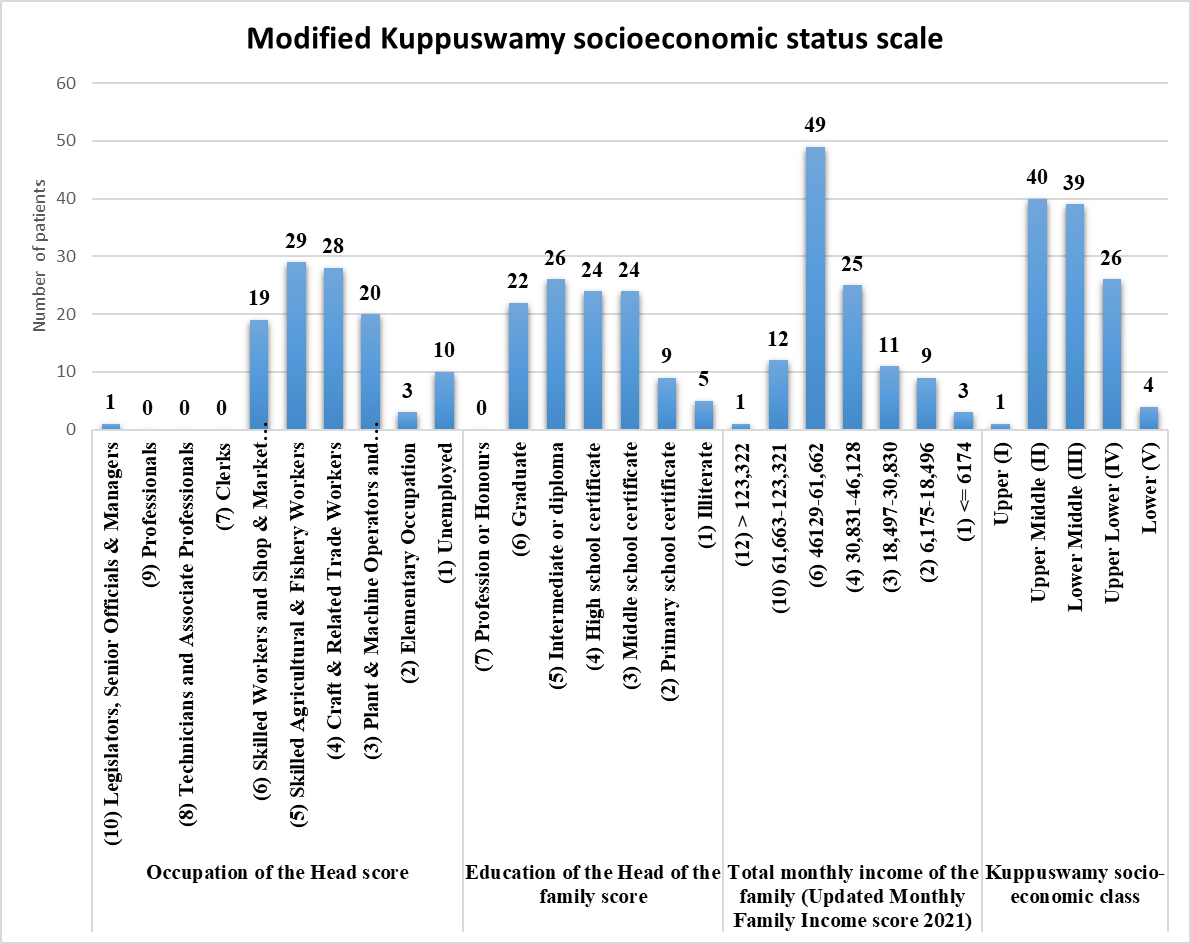
Occupation of the head of the family
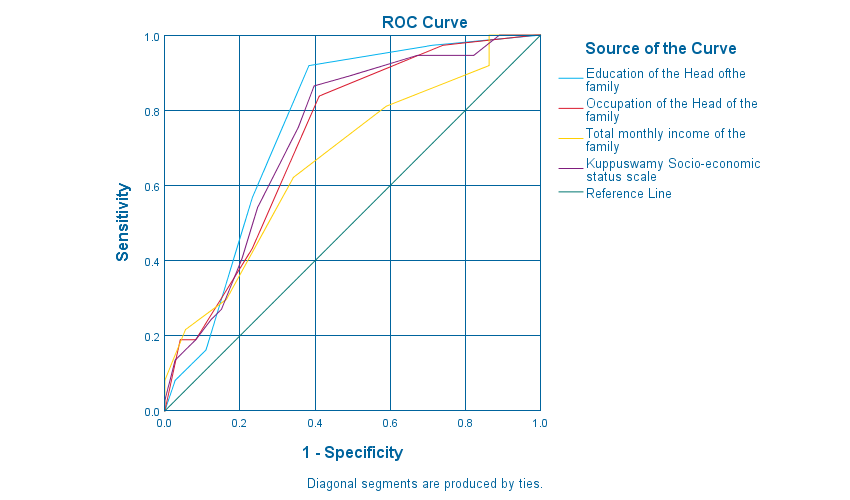
Frequency distribution of the parameters is shown in Figure 1, with the maximum of patients having a score of 5 (26.36%, n=29) followed by a score of 4(25.45%, n=28). Receiver Operator Curve (ROC) of Occupation score was analysed and showed area under the cure (AUC) of 0.726 (sensitivity 83.84%, specificity 58.91% p<0.001) ([Figure 2], [Table 3]). Upon analysing Occupation score and outcome, no significant association was observed (OR 2.553 95% CI 0.791 - 8.24, p=0.117).
Education of the head of the family
Majority of the patients had an education score of 5 (23.63%, n=26), followed by a score of 4 and 3 as shown in Figure 1. The ROC analysis was performed and showed AUC of 0.763 (sensitivity 91.93%, specificity 61.62%, p<0.001) ([Table 3], [Figure 2]). Using the cutoff value of less than 4, analysis was performed for Education score and poor outcome and a significant association was observed (OR 4.196 95% CI 1.803 - 9.769, p=0.001).
|
S.No. |
Occupation of the Head of the family |
Score |
|
1 |
Legislators, Senior Officials & Managers |
10 |
|
2 |
Professionals |
9 |
|
3 |
Technicians and Associate Professionals |
8 |
|
4 |
Clerks |
7 |
|
5 |
Skilled Workers and Shop & Market Sales Workers |
6 |
|
6 |
Skilled Agricultural & Fishery Workers |
5 |
|
7 |
Craft & Related Trade Workers |
4 |
|
8 |
Plant & Machine Operators and Assemblers |
3 |
|
9 |
Elementary Occupation |
2 |
|
10 |
Unemployed |
1 |
|
S.No. |
Education of the Head of the family |
Score |
|
1 |
Profession or Honours |
7 |
|
2 |
Graduate |
6 |
|
3 |
Intermediate or diploma |
5 |
|
4 |
High school certificate |
4 |
|
5 |
Middle school certificate |
3 |
|
6 |
Primary school certificate |
2 |
|
7 |
Illiterate |
1 |
|
S.No. |
Total monthly income of the family (Updated Monthly Family Income score 2021) |
Score |
|
1 |
> 123,322 |
12 |
|
2 |
61,663-123,321 |
10 |
|
3 |
46129-61,662 |
6 |
|
4 |
30,831-46,128 |
4 |
|
5 |
18,497-30,830 |
3 |
|
6 |
6,175-18,496 |
2 |
|
7 |
<= 6174 |
1 |
|
S. No. |
Kuppuswamy socio-economic status scale 2021 |
Socioeconomic Class |
|
1 |
26 to 29 |
Upper (I) |
|
2 |
16 to 25 |
Upper Middle (II) |
|
3 |
11 to 15 |
Lower Middle (III) |
|
4 |
5 to 10 |
Upper Lower (IV) |
|
5 |
<5 |
Lower (V) |
|
Parameters |
Good Outcome |
Poor Outcome |
OR(95% CI) |
P value |
|
|
Age (years) |
Mean ± SD |
34.41 ± 18.46 |
38.46 ± 16.65 |
- |
0.466 ‡ |
|
Gender |
Male |
45 (69.23%) |
20 (30.77%) |
1.363(0.613 to 3.03) |
0.447 † |
|
Female |
28 (62.22%) |
17 (37.78%) |
- |
||
|
Residence |
Rural |
42 (75.0%) |
14 (25%) |
0.667 (0.291 - 1.526 |
0.450 † |
|
Urban |
36 (66.67%) |
18 (33.33%) |
- |
||
|
Education of the Head of the family score |
>=4 |
56 (77.78%) |
16 (22.22%) |
4.196(1.803 to 9.769) |
0.001 † |
|
<4 |
17 (44.74%) |
21 (55.26%) |
- |
||
|
Occupation of the Head of the family score |
>=3 |
67 (69.07%) |
30 (30.93%) |
2.553(0.791 to 8.24) |
0.117 † |
|
<3 |
6 (46.15%) |
7 (53.85%) |
- |
||
|
Total monthly income of the family |
>=4 |
61 (70.11%) |
26 (29.89%) |
2.133(0.835 to 5.448) |
0.113 † |
|
<4 |
12 (52.17%) |
11 (47.83%) |
- |
||
|
Kuppuswamy socio-economic class |
26-29 Upper (I) |
1 (100%) |
0 (0%) |
- |
- |
|
16-25 Upper Middle (II) |
36 (90%) |
4 (10%) |
0.591(0.003 to 116.244) |
0.845 |
|
|
11--15 Lower Middle (III) |
21 (53.85%) |
18 (46.15%) |
4.128(0.022 to 767.722) |
0.595 |
|
|
5--10 Upper Lower (IV) |
14 (53.85%) |
12 (46.15%) |
4.136(0.022 to 783.934) |
0.596 |
|
|
<5 Lower (V) |
1 (25%) |
3 (75%) |
12.098(2.044 to 3352.747) |
0.038 |
|
|
Length of Hospital stay (Days) |
Median(25th-75th percentile) |
7(5-10) |
9(6-16) |
1.095(1.022 to 1.173) |
0.012 § |
|
Acute Symptomatic Etiology |
- |
41 (60.29%) |
27 (39.71%) |
2.049(0.871 to 4.82) |
0.112 § |
|
Estimated Cost of medication in previous year (Rupees) |
Mean ± SD |
5290.41 ± 15540.021489 |
2394.594 ± 9754.748 |
- |
0.053 ‡ |
|
Poor Financial Condition leading to Drug Default |
- |
10 (90.91%) |
1 (9.09%) |
0.252(0.041 to 1.562) |
0.139 † |
|
Estimated cost during Hospital Stay (Rupees) |
Median (25th-75th percentile) |
18000(10000-38000) |
43120(14000-96000) |
- |
0.006 § |
|
‡ Independent t test, § Mann Whitney test, * Fisher's exact test, † Chi square test |
|
Variables |
Area under the ROC curve (AUC) |
P value |
Cut off |
Sensitivity |
Specificity |
|
Education of the Head of the family score |
0.763 |
<0.001 |
<4 |
91.93% |
61.62% |
|
Occupation of the Head of the family score |
0.726 |
<0.001 |
<5 |
83.84% |
58.91% |
|
Total monthly income of the family score |
0.669 |
0.004 |
<4 |
62.27% |
65.82% |
|
Kuppuswamy socio-economic class |
0.736 |
<0.001 |
<14 |
86.56% |
60.31% |
|
Variables |
P value |
Odds ratio |
|
Duration of hospital stay (days) |
0.275 |
1.126 (0.91 – 1.392) |
|
Education of the head of the family |
|
|
|
>=4 |
- |
1 [Reference] |
|
<4 |
0.036 |
65.405 (1.322 - 3235.454) |
|
Kuppuswamy socio-economic class 2021 |
||
|
Upper{26 to 29} |
- |
1 [Reference] |
|
Upper middle{16 to 25} |
0.057 |
0.065 (0.018 – 1.345) |
|
Lower middle{11 to 15} |
0.259 |
0.164 (0.096 – 1.134) |
|
Upper lower{5 to 10} |
0.045 |
1.198 (1.013 – 1.305) |
|
Lower{<5} |
0.022 |
2.156 (1.235 – 9.307) |
Total monthly income of the family
Total monthly income score of 6 had the majority of the patients (44.54%, n=49) followed by a score of 4 (22.72% ,n=25) (Figure 1). ROC analysis showed an AUC monthly income score of 0.669 (sensitivity 62.27%, specificity 65.82%, p=0.004) ([Table 3], [Figure 2]). However, the association between low monthly income score and poor outcome was not significant (OR 2.133 95% CI 0.835 - 5.448, p=0.113).
Modified kuppuswamy socio-economic status scale
Majority of the patients were in Socio-economic Class II (36.36%, n=40) followed by Class III(35.45%, n=39) and on performing ROC analysis, the AUC was 0.736 (sensitivity 86.56%, specificity 60.31%, p<0.001). On analysing Socio-economic class and poor outcome only patients belonging to class V were significantly associated with poor outcome (OR 12.098 95% CI 2.044 - 3352.747, p=0.038) ([Table 2]).
Upon analysis independent risk factors of poor outcome using univariate logistic regression, Kuppuswamy Education score of the Head of family of less than 4 (p=0.036, OR 65.405 95% CI 1.322 - 3235.454) and Kuppuswamy Socio-economic Class IV and V were significantly associated with poor outcome (p=0.045, OR 1.198 95% CI 1.013 - 1.305 and p=0.022, OR 2.156 95% CI 1.235 - 9.307 respectively) ([Table 4]).
Financial burden of status epilepticus and outcome
In the present study 19.09% (n= 21) of the patients had a history of epilepsy and the patients were on antiepileptic medication (phenytoin 47.61%, n=10; Sodium Valproate 19.04%, n=5, Levetiracetam 23.80%, n=5 and clobazam 9.52%, n=2). The mean cost of medication in the last year of those patients who were on antiepileptic medication was 4368.8 ± 18943.9 Rupees.
The median of the length of hospital stay of the patients under study was 8(4 – 18) days. A significant association was observed with the length of hospital stay and poor outcome, with median length of hospital stay in patients with poor outcome of days 9(6-16) as compared to 7(5-10) days in patients with good outcome (OR 1.095 95% CI 1.022 - 1.173, p=0.012).
During the present hospital stay of the patients under study, the median of the cost incurred during the hospital stay, including expenses related to medical treatment, investigations, and ancillary services was 18000(4560 – 46903) Rupees and there were more with patients that had poor outcome as compared to patients with good outcome and a significant association was observed (p=0.006) ([Table 2]).
Discussion
Convulsive Status Epilepticus (CSE) is a neurological emergency that not only poses significant clinical challenges but also exerts a considerable economic burden on patients, families, and healthcare systems. In this discussion, we delve into the findings of our study and contextualize them within existing literature, highlighting the socioeconomic factors influencing the economic impact of CSE in Northern India.
Demographic parameters and clinical outcome
The mean age of the patients under study was 35.8 ± 18.0 years, and male patients were more as compared to females. More patients were from rural areas as compared to urban areas. The present study showed similar observations as compared to previous studies.[11], [12], [13]
Socioeconomic factors and clinical outcomes
Our study revealed several socioeconomic factors were significantly associated with clinical outcomes in patients with CSE. Notably, patients from families with a score of less than 4 of Education of the head of the Family (p=0.036, OR 65.405 95% CI 1.322 - 3235.454) and Modified Kuppuswamy Socio-economic Status Class IV and V (p=0.045, OR 1.198 95% CI 1.013 - 1.305 and p=0.022, OR 2.156 95% CI 1.235 - 9.307 respectively) were more likely to experience poor outcomes. This finding underscores the role of education in healthcare decision-making, treatment adherence, and access to resources.[4] Similarly, patients from families with lower occupational status tended to have poorer outcomes, suggesting a complex interplay between socioeconomic status and health outcomes.[14]
Additionally, our study found a trend towards poorer outcomes among patients from lower-income households and those with lower Kuppuswamy socioeconomic status scale scores. While these associations did not reach statistical significance, they highlight the socioeconomic disparities influencing the management and prognosis of CSE.[5] Previous research has demonstrated that low socioeconomic status is associated with inadequate access to healthcare services, delays in seeking medical care, and poorer treatment outcomes in epilepsy. [15]
Duration of hospital stay and cost of care
A longer duration of hospital stay was significantly associated with poor outcomes in our study (OR 1.095 95% CI 1.022 - 1.173, p=0.012), emphasizing the need for efficient management strategies to reduce hospitalization rates and improve patient outcomes. Prolonged hospitalization not only places a strain on healthcare resources but also contributes to indirect costs such as loss of productivity and income for patients and caregivers.[16] Moreover, the present study revealed a substantial correlation between higher expenses during hospitalisation and poor outcomes (p=0.006), underscoring the economic hardship endured by patients and their families which contributes to subpar medication adherence contributing to increased hospitalisation rates.
The high cost of medical care for CSE can exacerbate socioeconomic inequalities and lead to financial hardship, particularly for vulnerable populations in resource-limited settings. [2] Access to affordable healthcare services is crucial for ensuring equitable outcomes and reducing the economic impact of CSE on affected individuals and communities.
Implications for policy and practice
The results of our study have significant implications for healthcare policy and practice in Northern India and comparable contexts. Reducing socioeconomic disparities and enhancing access to healthcare resources are crucial for mitigating the economic impact of CSE and enhancing patient outcomes. Specific interventions that focus on improving individuals' understanding of health information, encouraging proactive healthcare practices, and offering financial support to families with low income can help reduce the influence of socioeconomic factors on the management of CSE.[17]
Moreover, initiatives aimed at enhancing the efficiency of healthcare delivery, maximising the allocation of resources, and minimising avoidable hospital admissions can mitigate the economic burden on patients and healthcare systems. To effectively address the economic impact of CSE and improve the well-being of affected individuals, it is necessary to employ multidisciplinary approaches that involve healthcare providers, policymakers, and community stakeholders. These approaches will help in developing comprehensive strategies.
Limitations and Future Directions
Although our study has contributed invaluable contributions, it is important to acknowledge and address its limitations. The present study may have limited generalizability due to the retrospective design and relatively small sample size. Moreover, the dependence on self-reported data for socioeconomic variables may introduce bias into our analysis.
Further research should prioritize prospective study designs with larger sample sizes and ongoing follow-up in order to validate our findings and investigate the fundamental processes that contribute to the correlation between socioeconomic factors and clinical outcomes in CSE.
Conclusion
In conclusion, our study highlights the significant economic burden of CSE in Northern India and underscores the influence of socioeconomic factors on clinical outcomes and healthcare expenditures. Addressing socioeconomic disparities and improving access to healthcare resources are critical for reducing the economic impact of CSE and improving patient outcomes.
Moreover, the research reveals a compelling correlation between prolonged hospital stays and heightened financial strain on CSE patients and their families. This underscores the importance of efficient healthcare management to minimize economic burdens associated with extended hospitalizations. Additionally, the study underscores the impact of low education scores on the economic consequences of CSE, emphasizing the need for educational interventions to enhance health literacy among affected individuals.
Source of Funding
None.
Conflict of Interest
None.
References
- E Trinka, H Cock, D Hesdorffer, AO Rossetti, IE Scheffer, S Shinnar. A definition and classification of status epilepticus--Report of the ILAE Task Force on Classification of Status Epilepticus. Epilepsia 2015. [Google Scholar]
- SV Thomas, PS Sarma, M Alexander, L Pandit, L Shekhar, C Trivedi. Economic Burden of Epilepsy in India. Epilepsia 2001. [Google Scholar]
- E Beghi, G Giussani, E Nichols, F Abd-Allah, J Abdela, A Abdelalim. Global, regional, and national burden of epilepsy, 1990-2016: a systematic analysis for the Global Burden of Disease Study. Lancet Neurol 2016. [Google Scholar]
- AG Diop, DC Hesdorffer, G Logroscino, WA Hauser. Epilepsy and mortality in Africa: a review of the literature. Epilepsia 2005. [Google Scholar]
- AK Ngugi, C Bottomley, I Kleinschmidt, JW Sander, CR Newton. Estimation of the burden of active and life-time epilepsy: A meta-analytic approach: Estimation of the Burden of Epilepsy. Epilepsia 2010. [Google Scholar]
- UK Misra, J Kalita, SK Bhoi, D Dubey. Cost of status epilepticus in a tertiary care hospital in India. Seizure 2015. [Google Scholar] [Crossref]
- A Sinha, DK Bhaumik. Treatment expenditure pattern of epileptic patients: a study from a tertiary care hospital, kolkata, India. Neurol Res Int 2014. [Google Scholar] [Crossref]
- S Ain, Z Khan, M Gilani. Revised kuppuswamy scale for 2021 based on new consumer price index and use of conversion factors. Indian J Public Health 2021. [Google Scholar]
- SM Saleem, SS Jan. Modified Kuppuswamy socioeconomic scale updated for the year 2021. Indian J Forensic Community Med 2021. [Google Scholar]
- JP Betjemann, DH Lowenstein. Status epilepticus in adults. Lancet Neurol 2015. [Google Scholar]
- R Dani, A Sodani, K Telang, R Nigam. Determinants of outcome in convulsive status epilepticus in adults: An ambispective study from central India. Ann Indian Acad Neurol 2019. [Google Scholar]
- A Bhalla, B Das, R Som, S Prabhakar, P Kharbanda. Status epilepticus: Our experience in a tertiary care centre in Northwestern India. J Emerg Trauma Shock 2014. [Google Scholar]
- A O Rossetti. Prognosis of status epilepticus: role of aetiology, age, and consciousness impairment at presentation. J Neurol Neurosurg Psychiatry 2006. [Google Scholar]
- N Muthiah, S Rothenberger, TJ Abel. Socioeconomic status and healthcare utilization disparities among children with epilepsy in the United States: Results from a nationally representative sample. Sci Rep 2023. [Google Scholar] [Crossref]
- A Gaitatzis, K Carroll, A Majeed, J Sander. The epidemiology of the comorbidity of epilepsy in the general population. Epilepsia 2004. [Google Scholar]
- J Jung, HY Seo, YA Kim, IH Oh, YH Lee, SJ Yoon. The economic burden of epilepsy in Korea. J Prev Med Public Health 2010. [Google Scholar]
- GA Baker, A Jacoby, D Buck, C Stalgis, D Monnet. Quality of life of people with epilepsy: a European study. Epilepsia 1997. [Google Scholar]
- Introduction
- Materials and Methods
- Results
- Demographic parameters and clinical outcome
- Socio-economic parameters and clinical outcome
- Occupation of the head of the family
- Education of the head of the family
- Total monthly income of the family
- Modified kuppuswamy socio-economic status scale
- Financial burden of status epilepticus and outcome
- Discussion
- Demographic parameters and clinical outcome
- Socioeconomic factors and clinical outcomes
- Duration of hospital stay and cost of care
- Implications for policy and practice
- Limitations and Future Directions
- Conclusion
- Source of Funding
- Conflict of Interest
