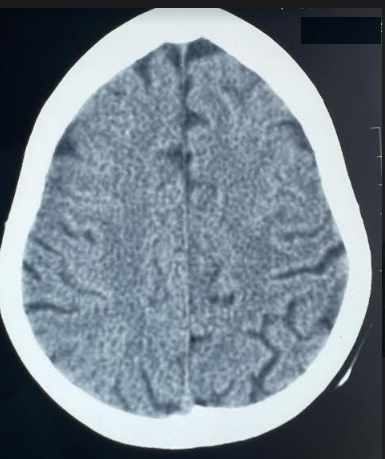
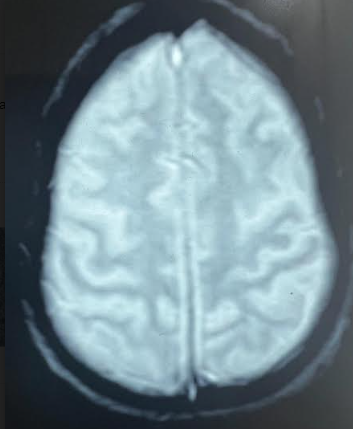
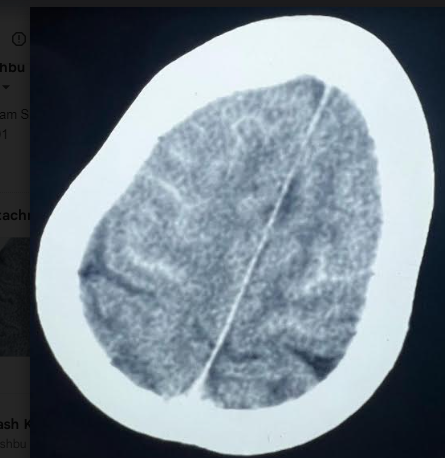
A 71-year-old lady with diabetes mellitus and hypertension was admitted under cardiology care for coronary angiography. Her hemoglobin level was 10.6 gm/dL and Serum creatinine was 1.2 mg/dL. She underwent uneventful coronary stenting (Iohexol 125 ml was used). 2 hours after the procedure she had an episode of seizure followed by altered sensorium. There was no history of fever, headache or vomiting. Her blood pressure was 140/80 mm of Hg and pulse was 80 per minute. On neurological examination she had a GCS of 10(E3M5V2]. There were no focal neurological deficits. There was no neck stiffness. Plain Computerised Tomography (CT) Head showed bilateral frontal sulcal hyperdensity and was reported as subarachnoid hemorrhage [Figure 1]. Basal cisterns did not show any hyperdensity. Bilateral frontal cortex and left basal ganglia showed subtle hyperdensity. Bilateral middle cerebral artery and basilar artery were hyperdense. She underwent immediate CT cerebral angiography and was normal. Lumbar puncture was done on the same day and it did not show any red blood cells. Repeat CT done with in 48 hours was normal [Figure 2]. MRI done at 72 hours after the ictus did not show any evidence of blood in susceptibility weighted Images [Figure 3]. Patient became normal in 48 hours and was discharged after 72 hours.
Increased attenuation of the basal cisterns and subarachnoid spaces on CT scans is a characteristic finding of acute subarachnoid hemorrhage (SAH). CT mimics of SAH are called pseudo SAH.
The term “pseudo-SAH” was first coined by Spiegel et al1 in 1986 in 10 patients with profound cerebral edema, and later Avrahami et al 2 described this phenotype in 100 comatose patients with cerebral edema due to various causes. It is also reported in purulent meningitis, cerebral infarction, subdural hematoma, status epilepticus, intracranial hypotension, polycythemia, intrathecal contrast administration and leakage of intravenous contrast in to subarachnoid space. 3
The most common neurologic complications associated with cardiac catheterization procedures include acute ischemic stroke secondary to atheroembolism, air embolism, vasospasm, and intimal dissection. Contrast-induced encephalopathy (CIE) is a rare complication of intravenous contrast administration.
Figure 1
Axial CT head showing bilateral frontal sulcal hyper density mimicking subarachnoid hemorrhage.
The clinical presentation of CIE varies widely, including altered mental status, focal motor and sensory deficit, visual disturbance, ophthalmoplegia, global aphasia, cortical blindness and seizures. Transient cortical blindness is the most commonly reported neurological symptom which has been attributed to the relatively higher permeability of the BBB in the occipital cortex. Symptoms usually occur in minutes to hours after contrast administration and typically resolve entirely within 24-48 hours. Radiologically, CIE can mimic subarachnoid hemorrhage (SAH) on CT head with hyperdensity in the subarachnoid space due to iodinated contrast extravasation. The current hypothesis for the underlying mechanism of CIE is disruption of the blood–brain barrier (BBB) allowing the contrast agent to permeate into the CNS causing direct neuronal toxicity and cerebral edema. Contrast agents also have epileptogenic potential and can result in seizures. 4 Risk factors for CIE are renal dysfunction, previous stroke, male gender, hypertension, diabetes mellitus and large volumes of contrast.
The density of lesion on Hounsfield scale may distinguish between blood and contrast, as contrast has higher attenuation values. CIE related subarachnoid hyperdensity usually resolves in 12-24 hours. MRI brains shows normal susceptibility weighted images (SWI) in CIE.CT scan of the vial of CSF also may be useful in diagnosing CIE. Dual energy computed tomography has shown to be able to distinguish between intracranial hemorrhage and contrast extravasation. 5
Diagnosis of subarachnoid hemorrhage in the setting of coronary angiography and stenting has grave therapeutic consequences. When CT head shows findings suggestive of subarachnoid hemorrhage following contrast administration, Pseudo subarachnoid hemorrhage should always be ruled out.