- Visibility 46 Views
- Downloads 7 Downloads
- DOI 10.18231/j.ijn.2024.009
-
CrossMark
- Citation
Post-encephalitic movement disorders - The natural course
Introduction
Encephalitis lethargica (1916-24) has been a mystery in the history of post-encephalitic movement disorders (PEMD).[1] Persistent central nervous system (CNS) virus has been attributed to various movement disorders; however, the finding is inconsistent.[2], [3] Japanese encephalitis (JE) may have a similar presentation with dystonia and parkinsonism. The exact pathophysiology and its course still need insight. Our study included three patients with varying movement disorders during the post-encephalitic phase and their course.
Case Description
Case 1
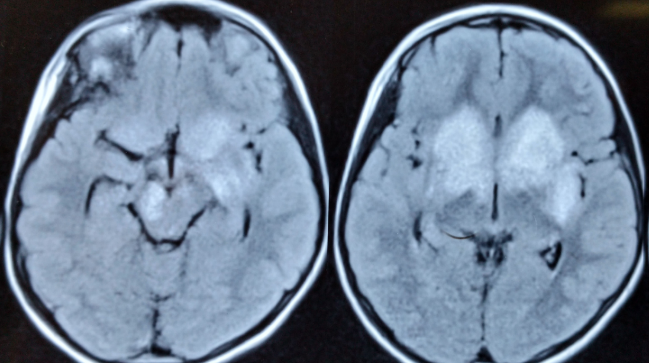
A-10-year girl presented with fever, abnormal behavior, and abnormal posturing of limbs of 20-days duration. Examination revealed generalized dystonia and speech difficulty. Magnetic resonance imaging (MRI) of brain showed T2/ Fluid attenuated inversion recovery (FLAIR) hyper-intensities in bilateral thalami, basal ganglia, brain-stem and basi-fronto-temporal lobe. ([Figure 1]) Cerebrospinal fluid (CSF) showed 25 cells (all mononuclear), 85 mg% protein and normal sugar. CSF for Herpes Simplex, Varicella Zoster, JE, and dengue were negative. Six months later, dystonia improved, but the patient developed hyperactivity, aggression, hyperorality, and hypersexuality. Antipsychotic treatment significantly reduced the symptoms. At 18 months of her illness, she developed stereotypy and vocal-tics, which persisted for six months. At the six-year follow-up, she is off medications, independent, and going to school with some writing difficulties.
Case 2
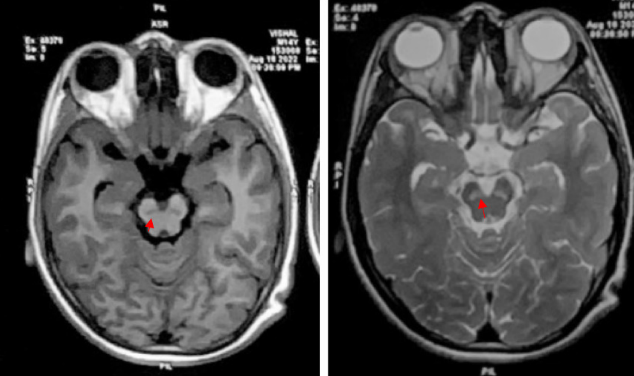
A-14-year male had a history of seven days of fever followed by altered sensorium. During convalescence, he developed parkinsonism. Levodopa led to improvement but he developed early motor-fluctuations with severe “on dyskinesias” at 18 months. Brain MRI showed bilateral symmetrical degeneration of substantia nigra(SN). ([Figure 2]) Dopaminergic therapy was optimized using dopamine-agonist and amantadine. He responded to treatment with 3-4 hours of “on” period and minimal dyskinesias.
Case 3
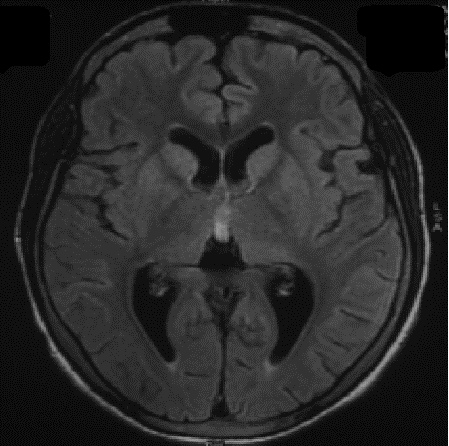
A-12-year boy presented with fever, generalized tonic-clonic seizures and altered sensorium for five days. His GCS was E2V1M1. He was started on acyclovir and antiepileptics. MRI-brain showed subtle T2-FLAIR hyperintensities in bilateral thalami and basal ganglia.([Figure 3]) CSF examination showed 80 cells (94% lymphocytes), 58 mg% protein and normal sugar. CSF was positive for IgM JE ELISA. At two months, he developed parkinsonism, left-hand dystonia, and echolalia for which he was given levodopa-carbidopa (125mg thrice daily) therapy, trihexyphenydyl (2mg thrics daily) and speech therapy. He showed good response over 1 month of therapy and we started gradual tapering of medications after 6 months. After one year, he is off medications and independent.
Discussion
In this case series, we present the diverse movement disorders encountered in patients suffering from acute viral encephalitis with a prolonged follow-up profile. Post-encephalitic movement disorders have varying spectrums. Dystonia, parkinsonism, tics, sterotypy, motor fluctuations along with behavioural abnormalities were evident in the post-febrile phase of illness in our case series. The involvement of thalamus, substantia nigra and basal ganglia could be related to genesis of such pattern of involvement in our patients. Due to the time-to development of symptom-onset (abnormal movements) in these case series, the element of post-encephalitis autoimmune involvement of deep gray matter of brain is suspected.[4] A phenomena of ‘persistence’ of movements have been described in a report by Murgod et al.[5] In a study by Jhunjhunwala et al, dystonia was found to be the commonest movement disorder in post-encephalitis sequelae, with thalamus attributing to the most common anatomical site. [6] In another study by Misra et al, it was observed that movement disorders are more common and severe in JE and are attributed to the involvement of the thalamus, basal ganglia and substantia nigra.[7] A concept of genetic insight into such predilection is an important aspect yet to be explored.[8]
Conclusion
Post-encephalitic movement disorders can have a plethora of manifestations. Post-encephalitic parkinsonism with SN degeneration may require long-term levodopa. However, other PEMDs may resolve after a few years of illness.
Source of Funding
None.
Conflict of Interest
None.
References
- LA Hoffman,, JA Vilensky. Encephalitis lethargica: 100 years after the epidemic . Brain 2017. [Google Scholar]
- V Ravi, A Desai, PK Shenoy, P Satishchandra, A Chandramukhi, M Gourie-Devi. Persistence of Japanese encephalitis virus in the human nervous system. J Med Virol 1993. [Google Scholar]
- UA Murgod, UB Muthane, V Ravi, S Radhesh, A Desai. Persistent movement disorders following Japanese encephalitis. Neurology 2001. [Google Scholar]
- T Armangue, M Spatola, A Vlagea. Frequency, symptoms, risk factors, and outcomes of autoimmune encephalitis after herpes simplex encephalitis: a prospective observational study and retrospective analysis. Lancet Neurol 2018. [Google Scholar]
- UA Murgod, UB Muthane, V Ravi, S Radhesh, A Desai. Persistent movement disorders following Japanese encephalitis. Neurology 2001. [Google Scholar]
- K Jhunjhunwala, M Netravathi, PK Pal. Movement disorders of probable infectious origin. Ann Indian Acad Neurol 2014. [Google Scholar]
- UK Misra, J Kalita. Spectrum of movement disorders in encephalitis. J Neurol 2010. [Google Scholar]
- AD Lanie, TE Jayaratne, JP Sheldon, SLR Kardia, ES Anderson, M Feldbaum. Exploring the Public Understanding of Basic Genetic Concepts. J Genet Couns 2004. [Google Scholar]
