Introduction
Stroke which occurs due to the sudden loss of blood flow to an area of the brain with the resulting loss of neurologic function, is a leading cause of disability and death globally. It remains a significant public health concern in India. 1 With its complex interplay of risk factors, including lifestyle, genetics, and demographic changes, stroke imposes a substantial burden on healthcare systems and individuals alike.
Stroke is no longer an affliction of the elderly. India has witnessed an alarming increase in the incidence of stroke among younger individuals in recent years. 2 This shift can be attributed to a rising prevalence of risk factors such as hypertension, diabetes, and unhealthy lifestyles, including poor diet and physical inactivity. As of 2021, the estimated prevalence of stroke in India stood at approximately 119-145 cases per 100,000 populations, making it one of the highest in the world. 3 Furthermore, the burden of stroke in India is compounded by the lack of awareness and access to healthcare services in rural areas, resulting in delayed treatment and poorer outcomes.
Rehabilitation is also a major part of stroke patient care. There is evidence to support that rehabilitation in a well-coordinated manner could make recovery faster. Potentially beneficial treatment options include constraint-induced movement therapy and robotics. Promising interventions that could be beneficial to improve aspects of gait include fitness training, high-intensity therapy, and repetitive-task training. 4 Occupational therapies can improve activities of daily living; however, information about the clinical effect of various strategies of cognitive rehabilitation and strategies for aphasia and dysarthria is scarce. Several large trials of rehabilitation practice and novel therapies are underway to inform future practice. In this study, we delve into the prevalence, treatment, pharmacotherapy, epidemiology, and prescription behavior concerning strokes in India. We also explored the therapeutic and pharmaceutical options available for stroke management in the country.
Materials and Methods
In this study, a cross sectional, multiple-response questionnaire based survey was carried out among doctors in cardiology practice in major Indian cities. This Indian survey on stroke was conducted from June 2022 to December 2022. The questionnaire booklet titled “The Stroke Study” was sent to the doctors who were willing to participate. The study questionnaire included questions on prevalence, diagnosis, co-morbidities, lifestyle, patient awareness, compliance, and pharmacotherapy. The study was conducted after receiving approval from Bangalore Ethics, an Independent Ethics Committee which is recognized by the Indian regulatory authority, Drug Controller General of India.
An invitation was sent to leading specialists in managing stroke in the month of March 2022 for participation in this Indian survey. About 93 consultants from major cities of all Indian states representing the geographical distribution shared their willingness to participate and provide necessary data. Stroke specialists were asked to complete the questionnaire without discussing with peers. A written informed consent was obtained from each clinician’s prior initiation of the study.
The data were analysed using descriptive statistics. Categorical variables were presented as percentages to provide a clear understanding of their distribution. The frequency of occurrence and the corresponding percentage were used to represent the distribution of each variable.
Results
In this survey, 43% of doctors see 11-20 stroke patients per month while another 26% of doctors see 21-30 stroke patients per month. This survey shows that acute stroke patients are more in the age group of 41-50 years (34%). About 24% of doctors observed stroke patients were in the 51-60 years’ age group while 25% of doctors saw stroke in the age group of 31-40 years of age group. More than half of the doctors surveyed observed vertigo prevailed equally in both genders. Also, 28% of the doctors said it prevailed in males and 21% of the doctors said it prevailed more among females (21%).
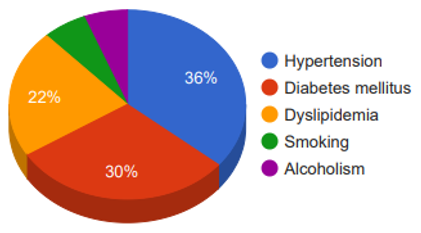
Nearly 50% of the doctors expressed that ischaemic stroke is the most often seen type of stroke, followed by cerebral hemorrhage (25%), hemorrhagic stroke (12%), and subarachnoid hemorrhage (8%). Hypertension is the most observed risk factor associated with stroke by 36% of the doctors in our survey. While 30% of doctors expressed that diabetes mellitus is the next most associated with stroke. Dyslipidemia is the third most observed associated risk factor with stroke. Smoking and alcoholism were other risk factors (Figure 1).
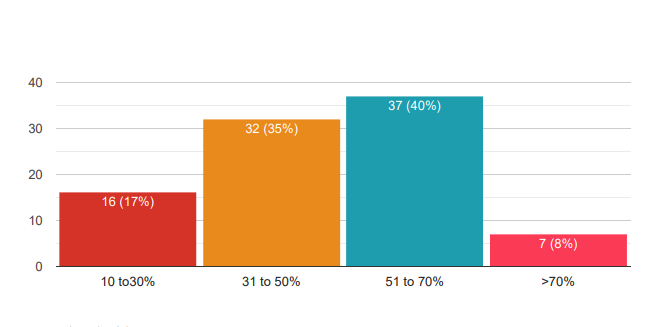
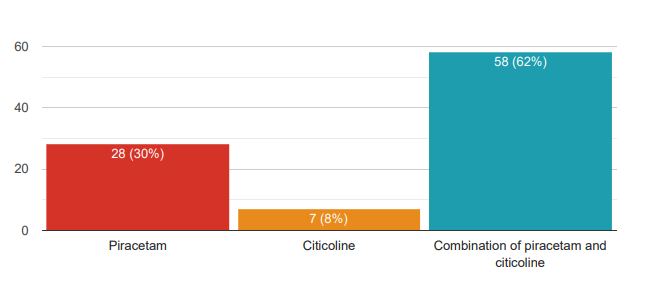
About 40% of the doctors prescribe to the extent of 51-70% of their patients, followed by 35% of doctors who prescribe to 31 to 50% of their patients. The third most significant percentage of neuroprotective agents is mentioned by 17% of doctors (Figure 2). In that, the most prescribed neuroprotective agent is the combination of piracetam and citicoline by 62% of doctors. Another 30% of doctors prescribe plain piracetam while only 8% of doctors mentioned citicoline as the prescribed neuroprotective agent (Figure 3). Piracetam is prescribed most for 3-6 months by 42% of doctors while another 38% of doctors prescribe for 1-3 months. On the other hand, 16% of the doctors prescribe piracetam for more than 6 months. In addition, piracetam 800 mg is recommended by 74% of doctors while other dosage strengths 400 mg is prescribed by only 12% and 1200 mg is prescribed by only 9% of doctors.
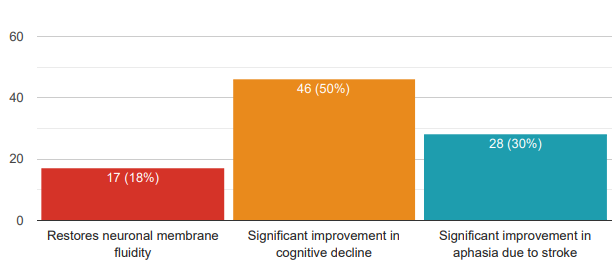
Furthermore, 50% of the doctors observed there is a significant improvement in cognitive decline. 30% of the doctors said there is a significant improvement in aphasia due to stroke and another 18% felt that it restores neuronal membrane fluidity (Figure 4). 93% of doctors surveyed in this study agreed with the opinion showing that using piracetam is good for cognitive improvement in post-surgery. When doctors in the survey were asked to rate patient compliance with piracetam, 39% of doctors rated it as very good while another 36% of doctors rated it excellent. Hence, both excellent to very good, 75% of doctor’s rate highly positive. Even another 20% rate is good. Only 5% rate it as satisfactory.
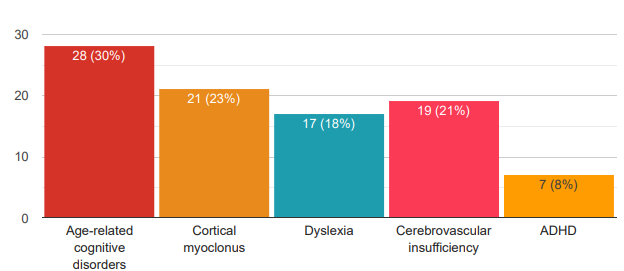
Moreover, this study indicates that 30% of doctors in the survey consider piracetam to be an effective option for age-related cognitive disorders. Another 23% of doctors indicate piracetam is effective for cortical myoclonus and 18% of doctors consider piracetam is an effective option for dyslexia. Another 21% of doctors said that the drug is an effective option for cerebrovascular insufficiency (Figure 5).
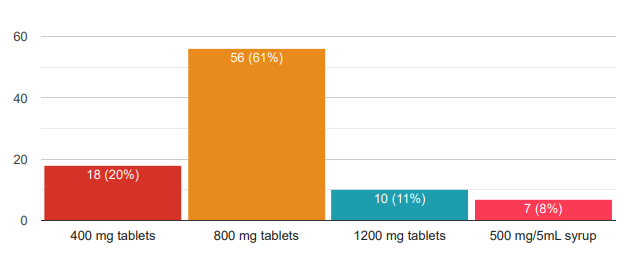
More than half of the doctors see 11-20 cases of vertigo per week which is most of the study group. 27% of the doctors see less than 10 cases while 17% of the doctors see 21 to 30 vertigo cases. One-fourth of doctors (25%) observed that vertigo prevailed among both the 21-30 years and 41-50 years’ age groups the most. 21% of doctors observed that vertigo is seen next most among the age group of 31-40 years.Figure 6 15% of doctors found it next most in the age group of 11-20 years while another 10% of doctors observed vertigo is seen among more than 50 years of the age group. This study indicates that 61% of doctors prefer 800 mg as the most preferred dose of piracetam for the management of vertigo. 20% of the respondents prefer 400 mg tablets while another 11% of doctors prefer 1200 mg for vertigo. Only 8% of respondents prefer 500 mg/5 ml syrup.
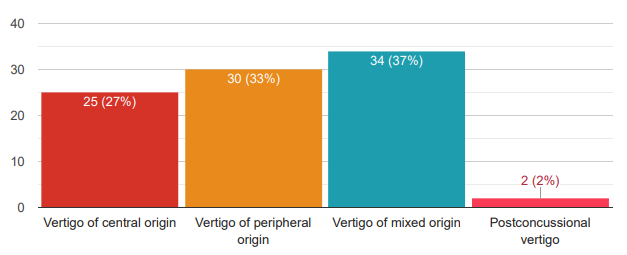
Doctors in the survey indicated that 37% of them prefer piracetam for Vertigo of mixed origin. One-third of doctors consider piracetam for Vertigo of peripheral origin. 27% of the doctors prefer piracetam for Vertigo of central origin (Figure 7). 46% of the doctors in the survey have the opinion that it lowers the severity of the vestibular & associated disorders of vertiginous attacks. Another 29% of the doctors have an opinion that piracetam decreases the frequency of exacerbations of vertiginous attacks. 23% of the doctors felt that the duration of the vestibular and associated disorders of vertiginous attacks.
Discussion
The present study examined the prevalence, clinical characteristics, management of stroke, and the usage of piracetam therapy in clinical practice using data collected from a substantial sample of over 100 doctors, achieving an impressive response rate of 93%. This high response rate indicates a strong engagement of healthcare professionals in the research. The study provides insights into the caseload of doctors regarding stroke patients. A significant proportion of doctors, 43%, reported seeing 11-30 stroke patients per month. This information is valuable for understanding the demand for stroke-related healthcare services. Understanding the age groups most affected by acute stroke is critical for targeting prevention and intervention efforts. 5 The study found that a substantial number of doctors (34%) reported a higher incidence of acute stroke among individuals aged 41-50 years. Various studies show that the mean age of ischemic stroke patients was 71.0±14.6 years, and older patients were more likely to have a history of atrial fibrillation or hypertension. 6 The study explored the diagnosis of vertigo and found that more than half of the doctors observed that vertigo is equally prevalent in both genders. This gender-neutral distribution is an interesting finding and could guide further research into the factors contributing to vertigo. Beyond the epidemiological gender-related differences, previous study data suggest that gender has a potential role as an etiopathogenetic factor in audio-vestibular disorders and it is probably responsible for the different clinical features observed. 7 Ischemic stroke emerged as the most observed type of stroke among patients, as reported by 50% of the doctors. This information highlights the importance of preventive measures and treatments targeting ischemic strokes. Previous studies also show a similar finding that ischemic stroke caused by arterial occlusion is the most common type of stroke. 8 Hypertension and diabetes were identified as the leading risk factors associated with stroke, according to 36% and 30% of the doctors, respectively. These findings underscore the importance of managing these risk factors to reduce the incidence of strokes. High blood pressure damages arteries throughout the body, creating conditions in which they can burst or clog more easily. 9 Weakened or blocked arteries in the brain put you at a much higher risk for stroke. The connection between diabetes and stroke is linked to how the body handles blood glucose to make energy. People with untreated diabetes end up with too much glucose in their blood, leaving their cells unable to receive enough energy. 10 Over time, excessive blood glucose can increase fatty deposits or clots in blood vessels that may lead to stroke. A significant portion of doctors (40%) reported prescribing neuroprotective agents to 51-70% of their patients. This insight sheds light on the prevalence of neuroprotective agent uses in stroke management. The study found that the combination of piracetam and citicoline is the most frequently prescribed neuroprotective agent, as reported by 62% of the doctors. The study also revealed that 42% of doctors prescribe piracetam for 3-6 months, indicating a standard treatment duration. Various studies have shown that Piracetam increases cerebral blood flow, enhance oxygen extraction, restore membrane fluidity and modulate neurotransmission. Likewise, citicoline has been shown to positively influence cerebral plasticity and neurorepair processes. 11 Hence, understanding the recommended dosage and duration of neuroprotective agents like piracetam is vital for the effective management of acute stroke and post-stroke sequelae. Doctors' opinions on the benefits of piracetam and citicoline for post-stroke recovery were diverse. While 50% observed a significant improvement in cognitive decline, 30% noted improvements in aphasia, and 18% believed it restored neuronal membrane fluidity. These findings reflect the multifaceted nature of stroke recovery. 12 A notable finding is that 93% of doctors in the study agreed with research showing that piracetam improves cognitive function post-surgery. This consensus among healthcare professionals supports the efficacy of piracetam in post-operative cognitive management.13 The cognitive performance one-week post-surgery was significantly better after surgery. The study assessed patient compliance with piracetam, with a substantial 75% of doctors rating it as "Excellent" to "Very good”. This high compliance rate suggests that patients are generally receptive to the treatment.14 Doctors' opinions on the effectiveness of piracetam for different conditions provide valuable insights. For example, 30% considered it effective for age-related cognitive disorders, indicating its potential in managing cognitive decline. Understanding the prevalence of vertigo cases among patients is essential for healthcare planning.15 The study found that more than half of the surveyed doctors see 11-20 vertigo cases per week. The study indicated that vertigo is prevalent across various age groups, with 25% of doctors reporting its occurrence in both the 21-30 and 41-50 age groups. This wide age range highlights the need for diverse approaches to managing vertigo. The majority of doctors (61%) prefer 800 mg as the most suitable dose of piracetam for managing vertigo, aligning with common practice. Doctors in the survey indicate that 37% of them prefer piracetam for Vertigo of mixed origin. One-third of doctors consider piracetam for Vertigo of peripheral origin. 27% of the doctors prefer piracetam for Vertigo of central origin. 46% of the doctors have the opinion that it lowers the severity of the vestibular & associated disorders of vertiginous attacks. A similar finding was seen in various studies where piracetam relieves vertiginous symptoms after a head injury or central vertigo, particularly in case of vertebrobasilar insufficiency.16 It helps to reduce the frequency of the vertigo but not the severity of the vertigo in case of recurrent or chronic vertigo. The dosage of piracetam usually described in studies for vertigo treatment is 2.4-4.8 g daily.
Conclusion
The study revealed that acute stroke patients were more prevalent among the age group of 41-50 years and more than half of the doctors surveyed observed an equal prevalence of vertigo in both genders. Ischemic stroke was reported as the most often seen type followed by cerebral hemorrhage. The combination of piracetam and citicoline was the most prescribed neuroprotective agent. Further, the specialists noted several benefits of piracetam and citicoline, including significant improvement in cognitive decline and aphasia due to stroke. These insights can inform healthcare strategies and guide further research in the field of stroke and vertigo management.