- Visibility 605 Views
- Downloads 45 Downloads
- Permissions
- DOI 10.18231/j.ijn.2023.041
-
CrossMark
- Citation
Survival and analysis of patients with various central nervous tumors who received post-operative radiation therapy: A retrospective study
- Author Details:
-
Virendra Bhandari *
-
Saloni Singhal
-
Ashar Lodi
-
Amresh Kumar
Abstract
Introduction: Central Nervous Tumors constitute 3% of cancer cases worldwide. The incidence of CNS tumors in India ranges from 5-10 per 100,000 population, ranking 14th among all other tumors and accounting for 2% of all malignancies.
Materials and Methods: The five most frequent tumors are astrocytoma (47.3%), Medulloblastoma (11.4%), craniopharyngioma (9.7%), ependymal tumors (4.8%), and nerve sheath tumors (4.1%). The tumor spectrum varies among different ages and sexes. The medical records of 238 patients were evaluated, out of which only 102 were fit for the study as per the inclusion and exclusion criteria.
Result: The 3-year median overall survival (OS) of 8 years and Progression Free Survival (PFS) of 7 years, while the 5-year median OS of 9 years and PFS of 7 years is recorded. Glioblastoma (GBM) is the most aggressive out of all histologies, with a 2-year survival of 31% and a median OS of 8 months, as per our study. We got some good results with brainstem glioma as well, with a 2-year survival of 40% and a median OS of 18 months.
Conclusion: The survival in CNS tumours has improved widely with adjuvant concurrent chemotherapy with temozolamide along with radiation postoperatively and then adjuvant for 6months to 1 year and it was also seen that more complete the tumour resection done, the better was the survival seen.
Introduction
Central Nervous Tumors (CNS) constitutes 3% of cancer cases worldwide. The incidence of CNS tumors in India ranges from 5-10 per 100,000 population, ranking 14th among all other tumors and accounting for 2% of malignancies.[1] According to Global Cancer Incidence, Mortality and Prevalence (GLOBOCAN) 2020, an incidence of 308102 new cases of CNS were reported, ranking 20th among all other tumors, causing 251329 deaths and 5-year survival of 837152.[2] The types of Primary Brain Tumors are Gliomas and Non-Gliomas. The Gliomas include Astrocytoma, Oligodendrogliomas, Ependymoma, and Brain Stem Glioma. The Non-Gliomas include Meningiomas, Pituitary gland and Pineal gland Tumors, Primary CNS Lymphomas, Medulloblastomas, Craniopharyngiomas, and Schwannomas. [3] The five most frequent tumors were astrocytoma (47.3%), Medulloblastoma (11.4%), craniopharyngioma (9.7%), ependymal tumors (4.8%), and nerve sheath tumors (4.1%). The tumor spectrum varies among different ages and sexes. According to the Central Brain Tumor Registry of The US (CBTRUS) data, glioblastoma (17.7%) and anaplastic astrocytoma (2.1%) were the most common malignant tumors in adults, whereas Medulloblastoma, germ cell tumors, and glioblastoma are more common among children and teenagers. [4]
Materials and Methods
This is a single-institute ecological study. All the patients of CNS tumours who attended the Department of Radiation Oncology, between October 2010 to December 2019 are included in the study. Total 595 patients attended our Outpatient Department (OPD) over these 10 years. All patients have treatment and follow-up data available in their medical charts, which were extracted for this study, and evaluated using a number of potential predictors of survival based on age, gender, primary tumor stage, control of primary tumor, post-operative tumor volume, after the approval from the ethical committee of the institution. The records of 238 patients could be evaluated, and only 102 patients were fit for the study as per the inclusion criteria, i.e., they completed definitive treatment as per their histology and exclusion criteria, i.e., the patients with a mode of death other than the progression of disease were excluded. The survival was confirmed by telephonic or physical follow-up and assessed using the Kaplan-Meier method.
Results
The medical records of 238 patients were evaluated, out of which only 102 were fit for the study as these completed the complete treatment by post operative radiotherapy. Out of 102, 41% are female, and 59% are male; hence our study showed a higher incidence to be in males than in females. The glioma being the most common histology, we got 75% of patients with glioma including all the histologies, 8% of Brainstem glioma, 5% pituitary adenoma, 4% medulloblastoma, 3% recurrent Meningioma, 2% meningioma, 2% pituitary craniopharyngioma and 1% pineoblastoma. The most commonly seen patients were of grade II among all histologies. The most common location of the tumor was frontoparietal or parietal lobe.All the patients were given post operative radioteharpy 55 to 60 Gray in six weeks on Linear accelerator along with Temozolamide where required.
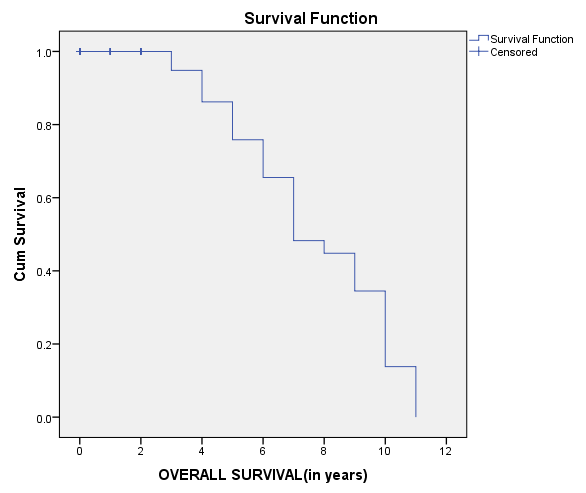
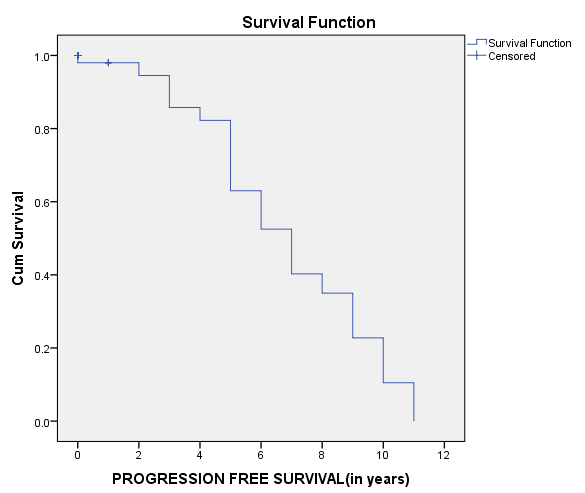
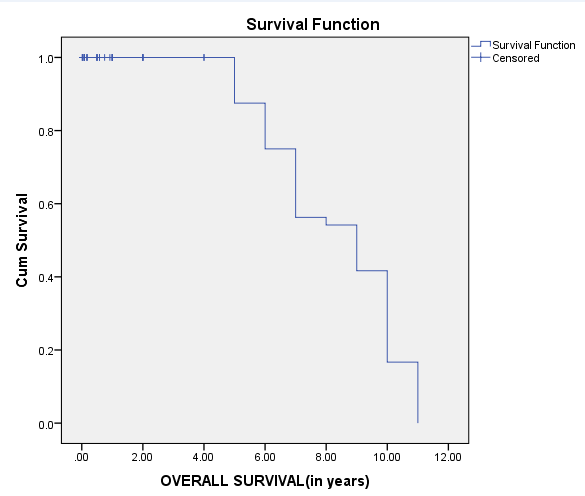
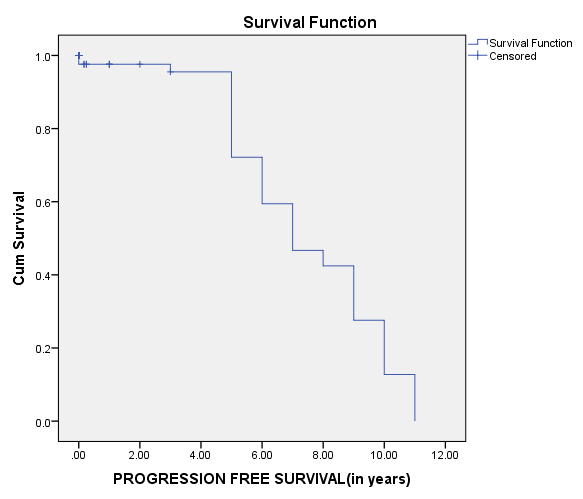
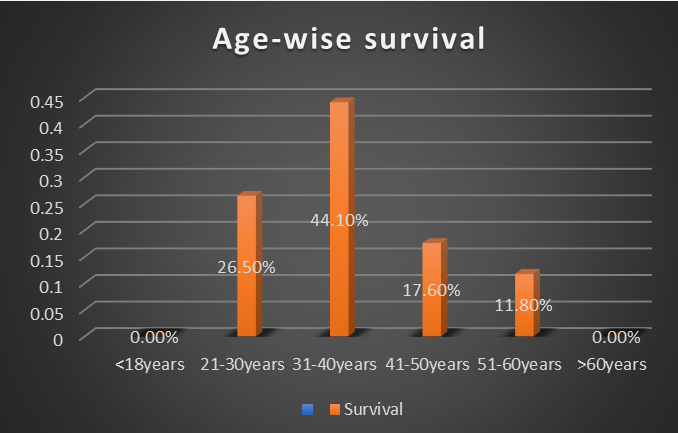
In our study, maximum survival was seen among patients from 21-40 years of age, i.e., middle-aged people with 44.1% among the 31-40years age group followed by 26.5% among the 21-30years of age group. The 3-year median overall survival (OS) of 8 years is shown. ([Figure 1]) and Progression Free Survival (PFS) of 7 years ([Figure 2]), while the 5-year median OS of 9 years ([Figure 3]) and PFS of 7 years are recorded. ([Figure 4])
Glioblastoma (GBM) is the most aggressive out of all histologies, with a 2-year survival of 31% and a median OS of 8 months, as per our study. We got some good results with brainstem glioma as well, with a 2-year survival of 40% and a median OS of 18 months. In patients with glioma or astrocytoma, grade II was the dominant histology with 77% of 3-year survival. The maximum survival was seen among patients from 31-50 years of age, i.e., middle-aged people, with 31.7% among the 31-40years of age group followed by 26.8% among the 41-50years of age group as shown. ([Figure 5]) On the basis of sex, females had better survival than males, with 42% of survival. The patients with lesser or no post-operative residual volume had better survival, with 73.5% of survival.
Discussion
According to a study by Kimberly R et al., over 18,000 CNS tumour patients, the male and female populations with malignant tumour were almost similar, with higher 2-year and 5-year survival in females,[5] while in our study, we had 59% males and 41% females with a 3-year survival of 42% among females and 40% in males.
In a study done by Brigitte Schlehofer et al., menopausal women had a higher risk of glioma than pre-menopausal women, whereas intake of female steroid hormones was significantly associated with a decreased risk of glioma.[6] As per their data, the pediatric population comprised 7% of patients with a higher survival rate, and the geriatric population with 37% of patients and lowest survival rate. Among adults, the maximum number of patients were above 35 years of age, with maximum survival rates among 20 to 34yrs of age. In our study, incidence among pediatric and geriatric populations were found to be the lowest, with insignificant data on their survival. The maximum number of patients were between 21-40 years of age, showing maximum survival rates of survival.
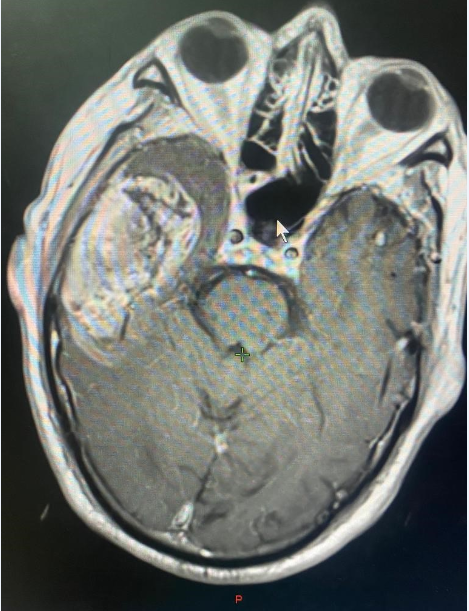
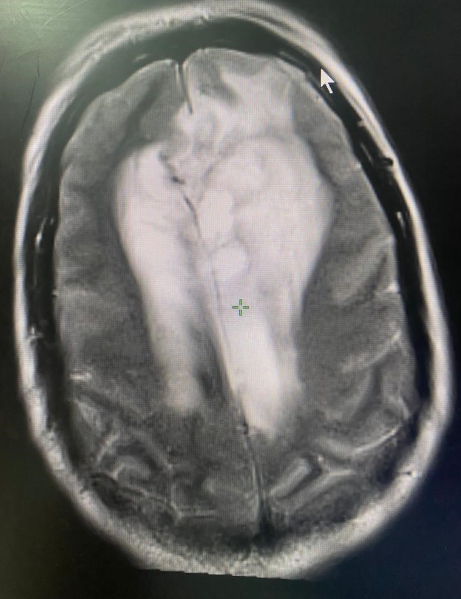
The presence of contrast enhancement on Magnetic Resonance Imaging (MRI) is even used as a criterion to discriminate anaplastic oligodendrogliomas from low-grade oligodendrogliomas. In our study, however, 23% of low-grade tumors showed contrast enhancement, while 35% of high-grade tumors had no visible contrast enhancement. As per studies, in grade II and grade III gliomas, the non-enhancing component represents the maximum proportion of the whole tumor ([Figure 6]), and it can be demonstrated by comparison of Fluid Attenuated Inversion Recovery (FLAIR) and contrast-enhanced T1 weighted images. The gliomas with high-grade lesions are heterogeneous in appearance, and gene expression with ill-defined boundaries, and the breakdown of the blood–brain barrier leads to an increase in enhancement and vasogenic edema. The glioblastomas are associated with epidermal growth factor receptor amplification and are associated with larger enhancing components ([Figure 7]) and ill-defined margins. [7]
In a literature search conducted by Nadir Sanai et al., including a database from January 1990 to December 2007, adult patients with hemispheric glioma were identified. In most of the studies, the extent of resection (EOR) was defined on the basis of gross total versus subtotal resection, and the effect of a greater EOR was more pronounced in the low-grade glioma studies, in which the mean survival increased from 61.1 to 90.5 months than the high-grade gliomas, in which the survival increased from 64.9 to 75.2 months in WHO Grade III gliomas and from 11.3 to 14.2 months in WHO Grade IV tumors.[8] In our study, we included only the patients who underwent surgery followed by definitive radiation; the postoperative CT scan or the radiotherapy planning CT scan was looked for the post-operative volume, and the survival was calculated as per the post-operative volume, which was found to be 73.5% including all histologies and grades of tumor, in patients who had lesser or no post-operative residual volume, hence concluding better survival among patients who underwent complete resection.
|
Author |
Histology of included patients |
Number of patients included |
Treatment strategy |
Median OS (in months) |
|
Jalali et al. [9] |
GBM |
42 |
RT+TMZ+ 6# TMZ |
16.4 |
|
Anand et al. [10] |
High-grade glioma |
46 |
RT+TMZ+ 6# TMZ |
15 |
|
Julka et al. [11] |
GBM |
215 |
RT+TMZ+ 6# TMZ |
13 |
|
Jalali et al. [12] |
Brainstem Glioma |
20 |
RT+TMZ(54Gy/30#) |
9.15 |
|
Singhal et al ( Present Study) |
GBM |
48 |
RT+TMZ+ 6# TMZ |
8 |
|
Brain Stem Glioma |
22 |
RT+TMZ+ 6# TMZ |
18 |
The standard management of high-grade glioma in the form of maximal safe resection followed by adjuvant radiotherapy (RT) along with concurrent Temozolomide (TMZ), followed by 6–12 cycles of adjuvant TMZ has been well established in the last decade. TMZ for radical treatment of newly diagnosed GBM was introduced in 2001 at TMH, with the first Indian data reported in 2007, which revealed 2 years survival rate of 28%, consistent with the Stupp's results of the landmark European Organisation for Research and Treatment of Cancer/National Cancer Institute of Canada study. [13], [14]
Comparing our results with the temozolomide arm of the study by Stupp et al.[13] The 3-year OS and 5-year OS rates of 58% and 42%, respectively, in our study reveal comparable results. Though the design of the trial by Stupp et al. was different from this study, and a strict comparison of the results cannot be done, the results seem to be comparable. The study by Stupp et al. is a randomized multi-institutional trial that included only patients of glioblastoma, while our study is a single-arm retrospective but mono-institutional, including all the histologies and grades of CNS tumors, and the median age of our patients is less than those in the study by Stupp et al.[13] Median overall survival in our patients, including all histologies, is 8 years, and for GBM and brainstem glioma is 8 months and 18 months, respectively.[15] We compared our results and compiled the data of various Indian studies done on post-operative adjuvant radiotherapy along with Temozolomide given in the histologically proven cases of different types of glioma and glioblastoma. ([Table 1])
Conclusion
Our study showed a higher incidence of brain tumours in male population, more commonly seen in the middle-aged population. The most commonly found histology is glioma, and GBM having the worst prognosis among all the histologies. The patients with lesser or no residual post-operative volume had a better prognosis; hence, the better the resection, the better the survival. Concurrent chemoradiotherapy with TMZ followed by additional cycles of TMZ yields encouraging outcomes, even in our patient population without significant toxicity, validating the published results.
Source of Funding
None.
Conflict of Interest
None.
References
- Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Ca Cancer J Clin. 2021;71(3):209-49. [Google Scholar]
- Noia C, Grist J, Riemer F, Lyasheva M, Fabozzi M, Castelli M. Predicting Survival in Patients with Brain Tumors: Current State-of-the-Art of AI Methods Applied to MRI. Diagnostics. 2022;12(9). [Google Scholar] [Crossref]
- Grossman SA, Ye X, Piantadosi S, Desideri S, Nabors L, Rosenfeld M. Survival of patients with newly diagnosed glioblastoma treated with radiation and Temozolomide in research studies in the United States. Clin Cancer Res. 2010;16(8):2443-9. [Google Scholar]
- . Central Nervous System Tumors (Brain and Spinal Cord) - Childhood: Introduction Approved by the Cancer.Net Editorial Board. . 2022. [Google Scholar]
- Porter K, Mccarthy B, Freels S, Kim Y, Davis F. Prevalence estimates for primary brain tumors in the United States by age, gender, behavior, and histology. Neuro-oncology. 2010;12(6):520-7. [Google Scholar]
- Schlehofer B, Blettner M, Preston-Martin S, Niehoff D, Wahrendorf J, Arslan A. Role of medical history in brain tumour development. Results from the international adult brain tumour study. Int J Cancer. 1999;82(2):155-60. [Google Scholar]
- Upadhyay N, Waldman A. Conventional MRI evaluation of gliomas. Br J Radiol. 2011;84(Spec Iss 2):107-11. [Google Scholar]
- Sanai N, Berger M. Glioma extent of resection and its impact on patient outcome. Neurosurgery. 2008;62(4):753-66. [Google Scholar]
- Julka P, Sharma D, Mallick S, Gandhi A, Joshi N, Rath G. Post-operativePost-operative treatment of glioblastoma multiforme with radiation therapy plus concomitant and adjuvant Temozolomide: A monoinstitutional experience of 215 patients. J Cancer Res Ther. 2013;9(3):381-6. [Google Scholar]
- Anand A, Chaudhory A, Aggarwal H, Sachdeva P, Negi P, Sinha S. Survival outcome and neurotoxicity in patients of high-grade gliomas treated with conformal radiation and temozolamide. J Cancer Res Ther. 2012;8(1):50-6. [Google Scholar]
- Jalali R, Basu A, Gupta T, Munshi A, Menon H, Sarin R. Encouraging experience of concomitant Temozolomide with radiotherapy followed by adjuvant Temozolomide in newly diagnosed glioblastoma multiforme: single institution experience. Br J Neurosurg. 2007;21(6):583-7. [Google Scholar]
- Jalali R, Raut N, Arora B, Gupta T, Dutta D, Munshi A. Prospective evaluation of radiotherapy with concurrent and adjuvant Temozolomide in children with newly diagnosed diffuse intrinsic pontine glioma. Int J Radiat Oncol Biol Phy. 2010;77(1):113-8. [Google Scholar]
- Stupp R, Mason W, Bent MVD, Weller M, Fisher B, Taphoorn M. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005;352(10):987-96. [Google Scholar]
- Dasgupta A, Gupta T, Jalali R. Indian data on central nervous tumors: A summary of published work. South Asian J Cancer. 2016;5(3):147-53. [Google Scholar]
- Kumar N, Kumar P, Angurana S, Khosla D, Mukherjee K, Aggarwal R. Evaluation of outcome and prognostic factors in patients of glioblastoma multiforme: A single institution experience. J Neurosci Rural Pract. 2013;4(Suppl 1):46-55. [Google Scholar]
How to Cite This Article
Vancouver
Bhandari V, Singhal S, Lodi A, Kumar A. Survival and analysis of patients with various central nervous tumors who received post-operative radiation therapy: A retrospective study [Internet]. IP Indian J Neurosci. 2023 [cited 2025 Sep 30];9(4):209-213. Available from: https://doi.org/10.18231/j.ijn.2023.041
APA
Bhandari, V., Singhal, S., Lodi, A., Kumar, A. (2023). Survival and analysis of patients with various central nervous tumors who received post-operative radiation therapy: A retrospective study. IP Indian J Neurosci, 9(4), 209-213. https://doi.org/10.18231/j.ijn.2023.041
MLA
Bhandari, Virendra, Singhal, Saloni, Lodi, Ashar, Kumar, Amresh. "Survival and analysis of patients with various central nervous tumors who received post-operative radiation therapy: A retrospective study." IP Indian J Neurosci, vol. 9, no. 4, 2023, pp. 209-213. https://doi.org/10.18231/j.ijn.2023.041
Chicago
Bhandari, V., Singhal, S., Lodi, A., Kumar, A.. "Survival and analysis of patients with various central nervous tumors who received post-operative radiation therapy: A retrospective study." IP Indian J Neurosci 9, no. 4 (2023): 209-213. https://doi.org/10.18231/j.ijn.2023.041
