Introduction
Parkinson's disease (PD) is a neurodegenerative disorder characterised by the degeneration of dopaminergic nigrostriatal pathway. The cardinal features of PD were first described by an English physician James Parkinson in 1817.
In general population, its incidence is predicted to range from 1 to 2 per 1000. The disease can vary with age, as it affects 1% of a general population over 60 and around 4% in the elderly and is still rare below 50 years of age. PD is a complex neurological illness, characterised mainly by motor symptoms including resting tremors, muscle stiffness (rigidity), akinesia or bradykinesia and postural instability. Various nonmotor symptoms (NMS) are, however, also found in PD, liken sleep disturbances, mental illnesses, autonomic impairments and sensory disorders. These NMSs can impair the quality of life of the patient (QoL).
Parkinson’s disease (PD) has been traditionally defined as a movement disorder. Non-motor symptoms (NMS) in PD typically become prominent in the later stages and such deficits can manifest first across multiple systems.1
Pathologically, the degeneration of a dopaminergic nigrostriatal pathway is ascribed to the PD motor symptoms. However, growing evidence has demonstrated that Parkinson’s Disease is a multi-system disorder. While Pathogenesis of PD has been primarily focussed on the dopaminergic symptoms, neuronal degeneration and inclusion body formation can also affect the cholinergic neurons of the Nucleus Basalis of Meynert, norepinephrine neurons of locus ceruleus, serotonin neurons in the raphe nuclei of brainstem. There is also involvement of neurons of the olfactory system, cerebral hemispheres, spinal cord and peripheral nervous system.
Understanding the biology of motor symptoms has been the driving force behind the development of both pharmacological and surgical treatments that have allowed them to be successfully managed over the past several decades. The pathophysiology of the NMSs, on the other hand, is still little understood. Recently, the importance of non-motor symptoms (NMSs) has increased, and it is now known that they may occur before the occurrence of motor symptoms and hence they may be beneficial in identifying people who are at risk of developing Parkinson's disease in the future.
It is noteworthy that clinical investigations have revealed that olfactory impairments, eye movement sleep behaviour disorder (RBD), weariness, and depression may all be key indicators of the preclinical stages of Parkinson's disease.
In the presence of effective symptomatic therapies for the motor symptoms of Parkinson's disease, the non-motor symptoms have become the major prognostic factors determining the overall disease burden and everyday function in Parkinson’s disease patients.
Materials and Methods
Tools of study
Data to be entered in the pre-designed, semi –structured questionnaire after taking informed consent.
Patients were evaluated at outpatient and inpatient level.
Informed consent was taken.
They were examined and interviewed.
Demographic Data and clinical manifestations were recorded in each patient.
Following scales were used to assess Parameters in the study.
UPDRS III (Unified Parkinson’s Disease Rating Scale) – to assess the severity of motor symptoms.
NMSS (Non-Motor symptoms scale) – to assess the frequency and severity of NMS in Parkinson’s patients.
PDQ-39 (Parkinson’s Disease Questionnaire) – to assess quality of life in patients with Parkinson’s disease.
The NMSS was translated in local language whenever needed.
Results
Demographic data revealed that the mean age of study population was 68 yrs. Also, the mean duration of disease was 5yrs.
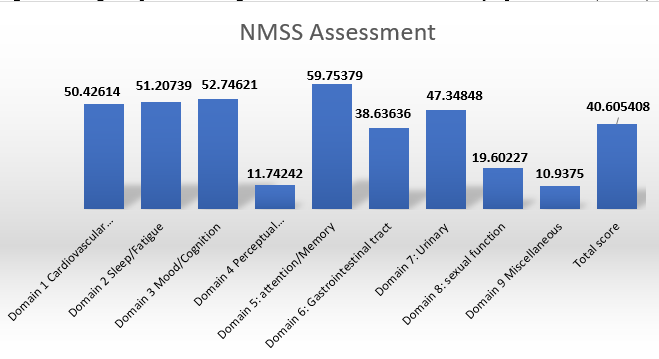
Amongst the Non motor symptoms, attention and memory was the most frequently reported domain in the study population (52 patients, 59.75 percent). The second most frequently reported domain was mood and cognition (46 patients, 52.74 percent) which included Anxiety, apathy, depression and mild cognitive impairment.
There were also a lot of people who had issues with sleep (45 patients, 51.2 percent) like insomnia, REM sleep behavioural disorders and restless leg syndrome. Cardiovascular symptoms including falls were reported in 50 percent study population.
Other non-motor symptoms reported in the study were urinary complaints (47.34 percent), gastrointestinal disturbances (38.63 percent), sexual dysfunctions (19.60 percent).
The least reported non-motor symptoms in the study were perceptual problems including delusions and hallucinations in 11.74 percent study population and miscellaneous domain (10.93 percent) which included pain, olfactory dysfunction, increased perspiration and weight fluctuations.
The mean UPDRS (part 3) score in the study population was found to be 33.24± 17.37 with values ranging from 3.57 (mild motor impairment) to 44.64 (severe motor impairment).
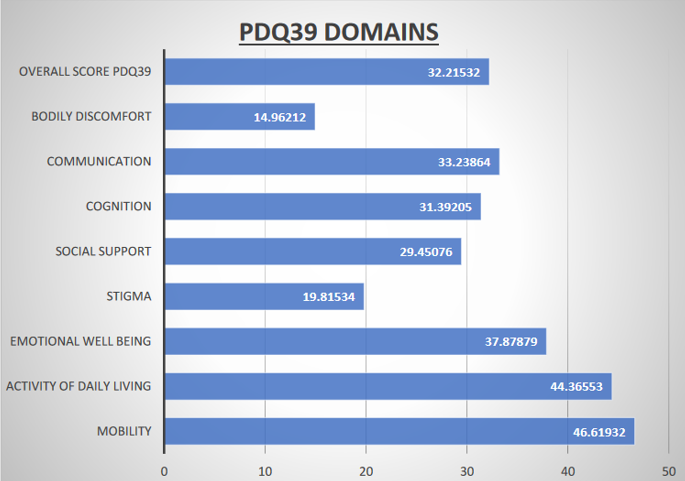
The Quality-of-Life assessment by PDQ-39 showed that impairment of Mobility had a major impact on quality of life followed by activities of daily living and emotional well-being. The domain least affected was bodily discomfort followed by Stigma amongst the study population.
Correlation between UPDRS (part 3) score and PDQ-39 domains (1 and 2) comprising of mobility and activities of daily living showed significant correlation suggesting that motor impairment had significant impact on quality of life in PD patients. Table 1, Table 2, Table 3, Table 4
Correlation between Non-motor symptoms and PDQ-39 revealed that mood, cognition and perceptual problems including hallucinations had an adverse outcome on the emotional well-being in PD patients. It also revealed that deficit in attention and memory had significant outcomes on communication.Figure 1, Figure 2
Table 1
Showing demographic data of the study population and mean duration of disease.
Table 2
Showing assessment of NMSS in different domains.
Table 3
Showing average scores of different domains in PDQ-39.
Discussion
This study is a Cross-sectional, one point in time evaluation study aimed at studying the frequency and severity of non-motor symptoms in PD and its impact on quality of life. Attention and memory issues, as well as mood/cognition disorders, were found in 59.75 percent & 52.74 percent of patients in our research, respectively, which were the non-motor symptoms which had the greatest impact on overall quality of life.
Study done by Chaudhary KR et al showed that sleep disturbances, cognitive impairment and bowel/bladder disturbances were frequent in PD.2
Shulman and Colleagues reported that NMS complex is frequently unrecognised and/or neglected by healthcare professionals. 3
Another International survey showed that 62.5% of NMS in PD remain unknown to healthcare professionals because patients are either too embarrassed to reveal them or are unaware that these symptoms are linked to PD. 4
Among the novel contributions of the present study is that it examines the data overall and employs scales such as the NMSS, that are particularly meant to address non-motor symptoms, as well as trying to compare the weighting of non-motor symptoms with that of motor symptoms assessed by component III of the UPDRS, and assesses its impact on quality of life.
In this research, we discovered that individuals with Parkinson's disease have the greatest effect on the quality of life because of their impairment in mobility and activities of daily living followed by emotional and cognitive symptoms.
The literature indicates that patients with axial symptoms appear to deteriorate in a much more linear manner; patients with problems associated with dopaminergic deficiencies (bradykinesia, rigidity), on either hand, have seemed to deteriorate in an exponential manner, with much more marked deterioration occurring during the early years of a disease.
Study done by Amruta Ravan et al on Parkinson’s disease patients in Indian cohort revealed that the number of symptoms correlates with disease duration and severity. When compared with control patients, it was shown that PD patients had significantly higher scores than controls concerning complaints of dribbling, impaired taste/smell, altered swallowing, constipation, urinary urgency, weight loss, forgetfulness, sadness, altered concentration, hallucinations, anxiety, sexual dysfunction, falling, daytime sleepiness, vivid dreams and sweating. 5
Another study conducted in the UK, USA, Germany, Israel, Japan and Italy comprising of 547 patients reported that the mean total NMS score was 10.3 ± 5.4 (SD). 6 It was found that nocturia (61.9%) was reported as the most frequent symptom while incontinence of faeces was the least prevalent symptom (8.21%).
Only 8 (1.6%) patients in this study did not report any NMS in this study. It was also found that depression/anxiety, sexual dysfunction, and cardiovascular and miscellaneous NMS were more prevalent in women.
Certain NMS of Parkinson’s disease have a wide scope of research, including sleep disturbances like EDS, as well as dementia and depression.
The first study done in India and among the few from Asia by Krishnan et al., compared 174 patients and 128 normal controls. It was done to assess the prevalence of non-motor symptoms and to document its relation to disease progression measured by the Hoehn and Yahr scale. It reported a higher frequency of NMS in all nine domains in patients with PD compared with controls. 7
Recent clinical study which was done by Yuan-Yuan Xu et al. examining depression in PD patients found it to be a persistent condition at 30 months of follow-up. 8 It was found that PD patients who suffered from depression at baseline persist with the condition and their mood disorder worsened significantly which was indicated by declining MMSE scores and increasing UPDRS scores. 8 This is especially significant due to the impact depression has on quality of life, often increasing cognitive decline due to disease morbidity. 8
Sleep disturbance as a NMS of Parkinson’s disease has been a topic of great interest recently. Videnovic et al. reviewed circadian rhythms in PD patients, discussing diurnal variations in motor symptoms of PD, as well as autonomic function, like blood pressure variability, and sleep disturbances, while accounting for improved dopaminergic medication pharmacokinetics. 9
Multivariate analyses conducted by Yonas E. Geda et al showed that apathy agitation, anxiety, irritability, and depression were most prevalent amongst patients with MCI. The OR was highest for delusion however, it was rare in both subjects with MCI and those with normal cognition. 10
An international pilot study of 96 healthy controls and 123 patients with various stages of treated and untreated PD was conducted by K. Ray Chaudhuri et al to demonstrate that the NMSQuest is a feasible, valid, and accepted tool. It showed that the NMSQuest accurately detects the NMS, and that the NMSS closely correlates with quality of life for PD patients. 11, 12, 13
It is important to involve allied healthcare professionals in providing care to PD patients, including physiotherapists, occupational therapists, and speech language therapists, among others.14 Literature mentions that they augment care, with patients benefiting in a variety of ways including improved gait, balance, and posture. 14
A restrospective analysis conducted by Alan Sadural et al showed that occupational therapy (OT) services are indicated for people with early Parkinson's disease (PD). It described the development and evaluation of a proactive, consultative OT program for people with early PD as a part of an integrated care approach. 15
Since non-motor symptoms have a serious impact on quality of life of patients, we need to broaden the conversation of Parkinson’s disease (PD) therapy to include debilitating non-motor symptoms (NMS).
Many of the non-motor symptoms precede the onset of PD by years or decades, like hyposmia, REM sleep disorder, constipation, depression, excessive day time sleepiness, fatigue, pain, and erectile dysfunction (ED). Hence, it is mandatory to include a screening tool for patients with common predictive mood, autonomic, cognitive, or sensory disturbances. This is important for patients with a positive family history of Parkinson’s disease, or with other positively correlated co-morbid conditions.
Conclusion
This study highlights the fact that non-motor symptoms in PD significantly impair quality of life and their timely treatment is an integral part of the overall management in PD patients. Bedside scales for assessment and evaluation of NMS such as the NMS Questionnaire can be useful in assessing the burden of NMS in Parkinson’s patients.
Clinicians should educate the patient and their family to help treat and decrease the impact of these symptoms. Regardless, education of both clinicians and patients will be an important factor in redefining the management of patients with PD.