Introduction
Dengue is a mosquito-borne arbo-viral disease which is found in all the areas served and monitored by WHO. According to one estimate, there are 390 million dengue virus infections per year, of which 96 million manifest as disease.1 Neurological manifestations can occur in dengue infection of any severity and any serotype of dengue might be associated, yet serotype - 2 and serotype-3 are most regularly reported.2 Neurological manifestation of dengue fever was first detailed in 1972; 3 due to better reporting, incidence in past few years has ranged between 0.5% to 20%. 4
Neurological complications of dengue infection, till 2012 were grouped, in view of pathogenesis. Murthy, Marzia and colleages5 proposed order in specifically 3 classes: (1) Systemic complications, e.g., stroke (both hemorrhagic and ischemic), encephalopathy, hypokalemic paralysis.(2)Direct Viral invasion, which includes meningitis, myositis, encephalitis, and myelitis.(3) immune mediatd responses, which included acute disseminated encephalomyelitis, myelitis, encephalopathy, neuromyelitis optica(NMO), optic neuritis and Guillain-Barré syndrome(GBS). 6
The patho-physiological premise of neurological complication in patients of dengue has been credited to three components. These are 1) systemic complications: like cortical anoxia, cerebral edema, intracranial bleed, electrolyte disturbance capillary leakage,hepatic and renal dysfunction, 2) direct viral injury and 3) immune mediated mechanisms. The beginning of manifestation of encephalitis in viremic stage during the early period of disease propose that the virus has the potency of crossing blood brain barrier and causing direct invasion of neurons causing neurological manifestation. The presence of dengue antigen in the cerebrospinal fluid severe dengue infection related with neurological manifestations additionally uphold the speculation behind neurotropicity of dengue virus. 7 Nearly in every case of dengue there is a present of responses from immne system and alteration in metabolites. 8 A couple of studies have discovered dengue infection antigen in cerebral tissue or dengue viral RNA in CSF samples. 9
Recent studies have suggested the role of neuroinflammation in dengue viral disease. The non structural 1 antigen (NS1Ag) is a secreted glycoprotein which functions as a cofactor for viral RNA replication and triggers cytokine release. The natural killer cells are tremendously involved in the pathogenesis of neurological manifestations as evidenced by their early activation and subsequently activate T helper (Th) cells. These Th cells divide and get converted to Th17 and Th9 cells, and promote further release of proinflammatory cytokines like interferon gamma, interleukin (IL) 12, IL-4 and transforming growth factor beta. These cytokines further damage the blood–brain barrier and subsequently facilitate the entry of other immune mediators into the brain and cause neuroinflammation. 10
In this review, we present some atypical findings of dengue virus infection when it affects the nervous system and attempt to highlight the need for its detection and management.
Materials and Methods
During the period from July 22 to September 2022, there were a total of about 356 cases of seropositive dengue infection. Out of these, about 22 patients had predominant neurological manifestations. In this case review, we present a total of seven confirmed cases of dengue to highlight the varied neurological presentation of dengue with a review of literature for the same. The clinical details of the cases have been obtained from retrospective analysis of the hospital records of the patients who were referred to or admitted at the Neurology Department , MLB, MC, Jhansi.
Laboratory diagnosis of dengue
To confirm the diagnosis of dengue infection in cases presented with neurological manifestations with fever, serum and CSF was subjected to assay Non-structural protein 1 (NS 1) Antigen( which is the only marker present in initial 3 days and disappear there after) and/or enzyme-linked immunosorbent assay (ELISA) for IgM (which is present from day 3-10 and is widely used as a diagnostic tools) and IgG antibody( mostly indicating past or resolving disease) against dengue virus and/or Polymerase chain reaction (PCR) study for dengue infection confirmation.
To differentiate dengue encephalitis from encephalopathy, detection of dengue virus, NS1 antigen or dengue virus-specific IgM antibodies in the cerebrospinal fluid (CSF) is helpful. In these cases, the sensitivity of RT-PCR is low in CSF as compared to serum due to low viral load. Abnormalities in CSF such as lymphocytic pleocytosis with mild increase in protein can support the diagnosis of dengue encephalitis.
Case Descriptions
Central Nervous System
Dengue encephalitis
Encephalitis among all the neurological complication of dengue encephalitis is the most severe one, and is reported in all 3 groups of disease .The criteria for Diagnosis of dengue encephalitis is proposed by Soares and Marzia (2014) 11 1) Presence of fever 2) Acute signs of cerebral involvement such as altered consciousness or personality and/or seizures and/or focal neurological signs 3) Reactive IgM dengue antibody, NS1 antigen or positive dengue PCR on serum and/or cerebrospinal fluid. The choice of one of these laboratorial methods should be performed according to the time of infection onset; 4) Exclusion of other causes of viral encephalitis and encephalopathy.
Although previously considered non-neurotropic, serotypes DEN-2 and DEN-3 are the most common ones implicated in causing an encephalitic presentation. In a recent Indian study serotypes DEN-1 and 2 were commonly found. 12 DEN-2 virus has been demonstrated in the cerebrospinal fluid of dengue patients and DEN-4 virus has been isolated by immunohistochemistry from medulla and cerebellum. There is no specific imaging pattern in MRI which suggest dengue encephalitis but according to some studies thalamic hyper intensity was found, which was found in our patient.
Case 1
A 28-year-old female presented with a history of high-grade fever followed by altered sensorium and an episode of seizure on the 6th day of illness. The patient was having GCS of 9 without menigeal signs and normal pupil size and reaction. Dengue serology of IgM anti body was positive with CSF having 15 cells (all lymphocytes) with mildly elevated protein and normal sugar.
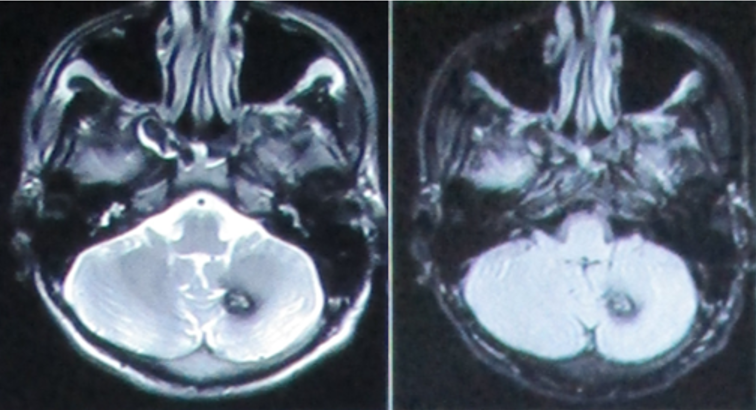
MRI brain was showing T2 flair hyper intensity in Right Midbrain and splenium (Figure 1). Though it was not specific for dengue encephalitis it was consistent with viral encephalitis.
The patient was treated conservatively and was recovered fully at discharged.
Case 2
It was a male patient of 34yrs. He was having fever and headache for 3 days which was followed by 1 episode of seizure and altered sensorium. The patient was vitally stable with GCS of 11. No meningeal signs or pupillary abnormality. CSF showed normal cells with elevated protein (110mg/dl) and normal sugar. MRI brain showed T2/FLAIR hyperintensity in temporal and thalamic regions consistent with dengue encephalitis (Figure 2A,B). The patient was treated conservatively and was discharged after 14 days.
Intracerebral bleed
Intracranial hemorrhage (ICH) is one of the rare manifestations of the central nervous system (CNS) involvement by dengue as a part of EDS. The pathogenesis is multifactorial attributed to the complex interplay of vasculopathy, coagulopathy, platelet dysfunction, and thrombocytopenia. 13
Vargas-Sánchez et al. (2014). In his study summarized cases of intracerebral bleed associated with dengue infection, in between 2001 and 2014. In these cases, DENV2 was detected in 5 patients and DENV3 in 1 patient. It involved various regions including the pons, basal ganglia, cerebellum and various lobes of cortex in brain. 14
Figure 1
A: MRI barin showing T2 flair hyperintensity of left splenium; B: MRI barin showing T2 hyperintensity of right mid Brain

Figure 2
A: MRI barin showing T2 hyperintensity of right thalamus; B: MRI barin showing T2 flair hyperintensity of right temporal lobe.
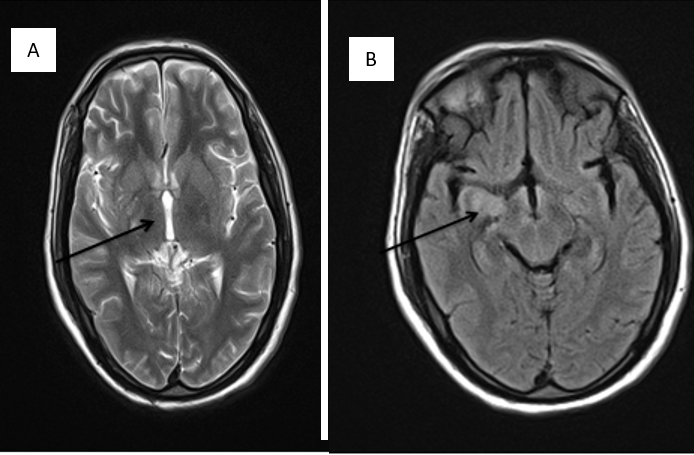
Figure 4
MRI cervical and dorsal spine; A,B: (coronal)- T2 hyperintensity of cord from C4 to T1; C,D: (axial)- T2 hyperintensity in cerical spine.
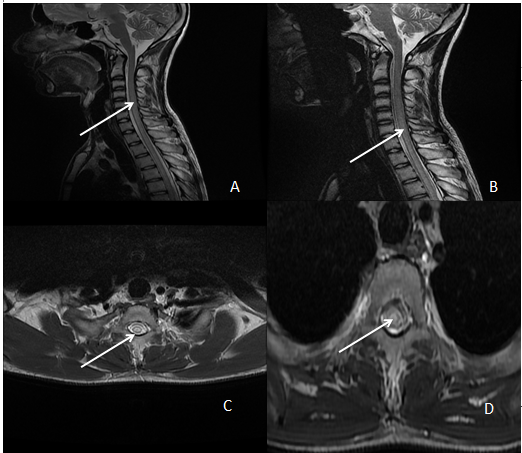
Table 1
Summary of cases
Case 3
A 34 yr male with history of fever with body ache for 4 days suddenly developed headache and vomting with instability of gait. Cerebellar signs were present on left side of the body. GCS was 15 with normal pupils. NS1 and IgM antibody for dengue was positive and MRI brain showed left cerebellar bleed.(Figure 3) Interestingly the platelet counts and coagulation profile were normal. The patient was treated conservativey and discharged after full recovery.
Transverse myelitis
Transverse myelitis (TM) is characterized by acute onset of sensory and motor symptoms along with bladder and bowel involvement attributed to inflammatory demyelinating lesions.15
In case of dengue infection pathogenesis of myelitis is attributed to invasion of virus. Dengue IgG production inside the thecal area also provide evidence of its affinity to spinal region.16 Secondly immune mediated mechanism is also involved in the pathogenesis of myelitis. 17 In these cases, the spinal cord involvement could represent a partial phenotypic manifestation of acute disseminated encephalomyelitis post-viral, which is an idiopathic inflammatory demyelinating disease related to infections or vaccinations.
Case 4
A 32 year female with a history of fever for 6 days with dengue IgM positive, presented with acute onset weakness of all 4 limbs with bladder involvement. There was associated back pain. Sensory level was t2. MRI Spine showed T2 hyperintensity from C4 to T1 S/O of LETM.(Figure 4) The patient was treated with methyl prednisolone pulse and was recovering on discharge. On follow up after 3 months the patient was having full recovery.
Peripheral nervous system
Dengue infection also involves peripheral nervous system and its manifestations are very debilitating but reversible. They must be suspected when a dengue serology positive patient present with sensory or flaccid paralytic complains. The conditions described in association with dengue virus infection include acute polyradiculoneuritis, lumbosacral plexopathy, Guillain Barre Syndrome (GBS), Miller Fisher syndrome and mononeuropathies such as phrenic neuropathy, long thoracic neuropathy, isolated Bell’s palsy, abducens nerve palsy and oculomotor palsy.
Gullian barre syndrome
In literature there are few cases of GBS reported in association with dengue.18, 19 In dengue, due to abberant immune response, cross reacting with the peripheral nerve through molecular mimicry.20 Various Pro-inflammatory matters for example TNF, IL, and the complement thought to have a major hand in pathogenesis of GBS.21 In dengue infection signs of GBS develop within the period of 1-19 days. In study of Simon et al. Gullian Barre syndrome was found to happen early in Dengue Fever with an average time between fever and neurological symptoms has been 2 days, range (1 to 3 days) 18
Case 5
The patient a 30 year male with a history of dengue fever 8 days back presented with acute onset ascending quadriparesis without bladder bowel involvement and sensory level and the patient was bed ridden in 48 yrs. NCV was done and AMAN pattern was found. Serum potassium level was normal. CSF showed akbumino-cytologica dissociation. The patient was graded as GBS and was given IVIg for 5 days. The patient started improving from 5th day and on 4 week follow up his motor recovery was full with mild sensory symptoms.
Hypokalemic paralysis
Various authors has observed Dengue-associated hypokalemic paralysis in numerous case report and case series. 22, 23 Hypokalemia causes ischemia of muscle and constriction of vessels which thought to be the reason behind increased CPK. 24 It is being stipulated the mechanism behind the genesis of hypokalemic paralysis in dengue is due to redistribution of pottasium in cells and temporary renal tubular malfunction causing increase in potassium excretion in urine. 25
Case 6
A 42 yr old female with history of fever for 2 days presented with acute onset weakness of all for limbs with pain in thigh. There was no bladder bowel or sensory symptoms. On examination the patient was areflexic with flexor planter. After doing NCV AMAN pattern of was found. Serum potassium came to be 2.1 meq/dl. Serum CPK was high. The patient was supplemented with potassium intravenously after which he made full recovery in 48hrs. in next 2 days the fever subsided and was discharged. Throughout the course of illness the platelet level was normal.
Mono neuritis multipex
To our knowledge, mononeuritis multiplex as a complication of Dengue infection has been described in a recent article where the patient after dengue fever presented with foot drop. 26 Another publication by medical department of the US Navy analyzed the complications of dengue fever following an outbreak in the Central Pacific in 1924. Mono neuropathies including facial, ulnar, peroneal nerves were reported. There was no history of recent illness or trauma, but no nerve conduction study was conducted in the patients. Follow up on the patients recovery was also not done. 27
Case 7
A female 26 years old presented with a history of fever 9 days back and was diagnosed as dengue. It was treated conservatively and on the 8th day the patient started having pain and tingling sensation in the left hand. The fever subsided on the 6th day but the symptoms on the left upper limb progressed. There was no complaining in any other limbs. Wrist grip in left hand was weak with all other normal examination finding. NCV was done and sensory motor axonal neuropathy was seen in median and ulnar nerve of left hand. The patient was put on oral steroids for 14 days and recovered fully on follow-up.
Principles of treatment
Management is supportive mostly. Control of fever with anti pyretic and cold sponging calculated fluid supplementation is mostly required in dengue fever from day-3 of fever onset till the disease subside its prudent to monitor platelet level and hematocrit on daily basis, along with TLC and LFT. Dengue Hemmoragic Fever warrants aggressive fluid management to avoid dehydration and shock. Increment of hematocrit by 20 % warrants aggressive fliud therapy to avoid circulatory collapse. Lack of antivirals for dengue make the management mainly supportive. Trials of vaccine development against dengue is in pipeline.
There is no specific treatment available for most of the neurological complication. Encephalitis is managed supportively and symptomatically for example anti epileptic drugs for seizures, decongestant for increased ICT. Inotropes can used in the case of myocarditis. In myelitis and myositis steroids are used. IVIg therapy is employed in GBS. Potassium in hypokalemic paralysis.
Conclusion
The pathogenesis of dengue associated neurological complications are multimodal. Through these cases we have tried to show that in certain disease with less latency period direct viral invasion is primodal mode of pathogenesis while those with longer latency period it is immune mediated. There is upcoming evidence of neurotropism and neuroinvasion in cases of dengue infection. Through supportive and disease specific interventions, the neurological complications are mostly manageable with very less mortality. Cases like hypokalemic paralysis and mononeuritis multiplex can occur following dengue and a knowledge of this can help in reducing the over evaluation of the patient saving time and money. These manifestations are mostly reversible and patients have full recovery with appropriate treatment. Thus it’s imperative to promptly identify and treat the diseases. Previously dengue was thought to be non- neurotropic virus but with knowledge of these cases it can be definitely said that it has varied neurological manifestations. With this knowledge of manifestation, early and prompt diagnosis and effective treatment can be given without spending time and fortune in finding other causes.