Introduction
Primary Non-Hodgkin's lymphoma of the skull with extracranial and intracranial extension but no systemic or skeletal symptoms in an immunocompromised patient is highly uncommon. Only ten such cases have been documented in the literature to date, and none of them had the lesion placed in the midline.1
Case Presentation
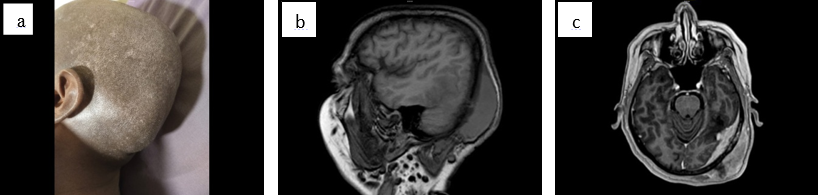
A 40 years old female was presented with a diffuse swelling in the left side of the scalp since 3 months of duration and progressively enlarging in size. On local Examination of the scalp, there was a diffuse swelling in the left parietal and occipital region of scalp. Magnetic resonance Imaging (MRI) showed contrast enhancing mass of size 8.3*3.5*5.2 cm arising from left parieto occipital bone with adjacent dura. The lesion is involving both marrow as well as cortex with infiltration of the adjacent dura with significant subgaleal component reported as differential diagnosis of 1) En plaque meningioma; 2 Solitary fibrous tumor of the dura; 3 Metastasis (Figure 1 a,b,c).
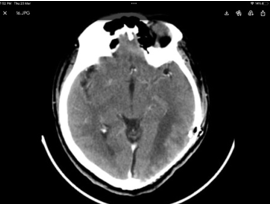
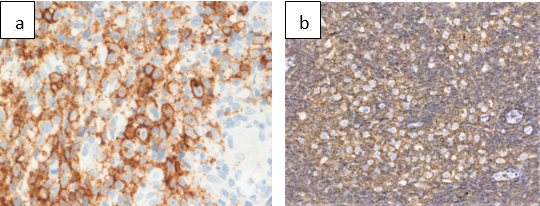
Patient underwent left parieto occipital craniotomy and gross total excision of the lesion (Figure 2) Histopathology reported as primary Non-Hodgkin’s lymphoma favoring diffuse large B cell lymphoma. (Figure 3). PET CT was done showed post-operative changes without any obvious metabolically active lesion in the brain parenchyma. Case was discussed in tumor board and has been planned for 4 cycles of chemotherapy with R-MPV (Rituximab, Methotrexate, Procarbazine and Vincristine) and then reassess.
Discussion
Because most primary cutaneous B-cell lymphomas (PCLs) involve the head and neck region, PCL of the scalp must be distinguished from primary malignant Non-Hodgkin's lymphoma of the cranial vault, which is more frequently associated with intracranial (extradural) extension. 2 Protruding tumorous angiolymphoid hyperplasia with eosinophilia (ALHE), Kimura's disease of the scalp, pseudolymphoma, cranial vault meningioma, and metastasis are all relevant clinicopathologic and radiological differential diagnoses. 3, 4 Primary NHL of the cranial vault has a shorter duration of symptomatology and an earlier onset of localized neurological impairments, a massive soft-tissue mass, and severe osteolytic lesions. In our case, the disease progressed slowly over a year, with no intracranial/orbital invasion and modest damage of underlying bones by the diffusely infiltrating soft tissue mass. 5 Despite this, primary malignant lymphoma of the skull can spread outside the cranium first and then within it, so at presentation, more than half of patients report a scalp lump rather than any neurological symptom. Subcutaneous malignant lymphoma, on the other hand, may eventually affect the underlying skull and dura. 6, 7 The majority of PCLs are hyperdense on unenhanced CT and show significant enhancement on postcontrast investigations. Magnetic resonance imaging is useful for assessing local and regional dissemination to detect if bone marrow, leptomeninges, or dural venous sinuses are involved 8. Gallium scanning can rule out or confirm extracutaneous involvement, and the presence or absence of activity in gallium avid lymphomas can aid to determine the type of remaining soft tissue masses after chemotherapy/radiation. The second most prevalent site of extranodal lymphoma is the skin. T-cell lymphomas account for 65% of them, with mycosis fungoides being the most prevalent form of low-grade malignant peripheral cutaneous T-cell lymphoma. B-cell lymphomas account for 25%, with rare variations or nonclassifiable lymphomas accounting for the remaining 10%. At the time of diagnosis, about 15 to 25% of cutaneous lymphomas had extracutaneous symptoms. Because the usual survival period following diagnosis is 12 to 14 years, 9 the prognosis is relatively good. We are reporting this case since it is unusual. We are reporting this case because of its rare occurrence. A diagnosis of primary lymphoma of the skull vault should always be considered in the differential diagnosis when such a lesion is encountered in middle aged and elderly patients.
Conclusion
A uncommon disease is primary non-Hodgkin's lymphoma of the cranial scalp and skull vault. Because most primary cutaneous B-cell lymphomas (PCLs) include the head and neck region, PCL of the scalp must be distinguished from primary malignant Non-Hodgkin's lymphoma of the cranial vault, which is more usually linked with intracranial (extradural) extension. Because the average survival period following diagnosis is 12 to 14 years, the prognosis is relatively good.