- Visibility 174 Views
- Downloads 30 Downloads
- DOI 10.18231/j.ijn.2023.032
-
CrossMark
- Citation
Double-barrel STA-MCA bypass for a giant thrombosed supraclinoid ICA aneurysm with gangliocapsular infarct – A case report
Introduction
Crowell and Yasargil published the first reported case of superficial temporal artery-middle cerebral artery (STA-MCA) bypass in 1969, in a patient with complete MCA occlusion.[1] STA-MCA bypass has been used successfully in the treatment of patients with giant aneurysms, cranial base tumours, moyamoya disease and steno-occlusive disease. Most surgeons have described this using the parietal branch of the STA to anastomose in an end-to-side fashion to a distal branch of the MCA.[2], [3], [4], [5], [6], [7] This technique is referred to as a “low-flow” bypass.[8], [9] In an attempt to augment the flow and toredirect flow to different ischemic areas of the brain, a “double-barrel” technique is used in which both branches of the STA are used to revascularize different MCA territories. It has also been shown to provide “high flow,” as measured by intraoperative quantitative flow measurement. The standard imaging evaluation for bypass candidates with steno-occlusive disease included Magnetic resonance imaging (MRI), 6-vessel Digital subtraction angiography (DSA), and CT perfusion (CTP) with acetazolamide challenge to assess for areas of ischemia, vascular occlusion, and collateralization, and regions of hypoperfusion with impaired cerebrovascular reserve.
Surgery was recommended for symptomatic patients with evidence of ischemia and impaired cerebrovascular reserve despite their receiving best medical management, in accordance with proposed clinical recommendations.[10], [11] The patient selection criteria was similar to that used for STA-MCA single barrel flow augmentation bypass. +Surgical technique includes using a linear incision following the parietal branch of the STA with a small frontal satellite incision, the two branches of the STA are harvested as donor vessels. These are anastomosed to recipient distal MCA vessel in temporal and proximal branches of frontal MCA. So this technique is used for augmentation of flow and to directly perfuse the hypoperfused regions of different areas of MCA territories.
Case Report
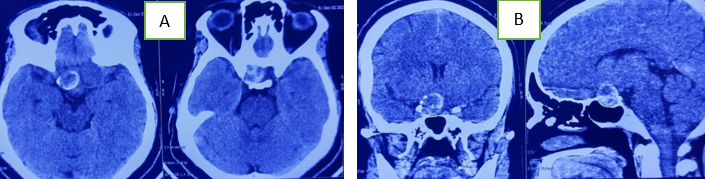
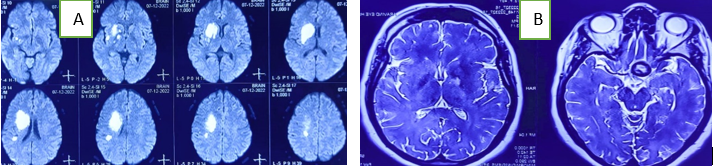
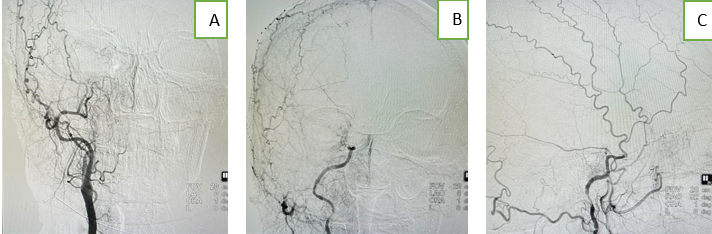
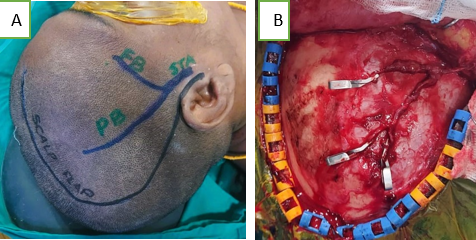
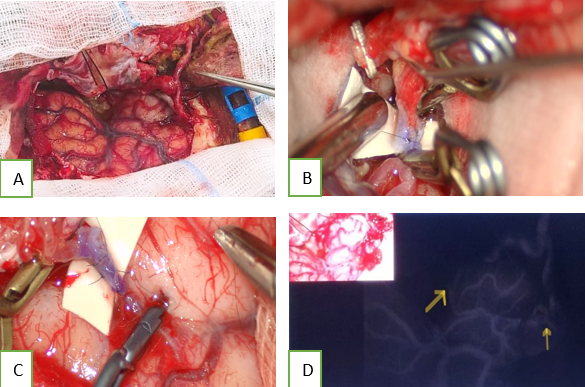
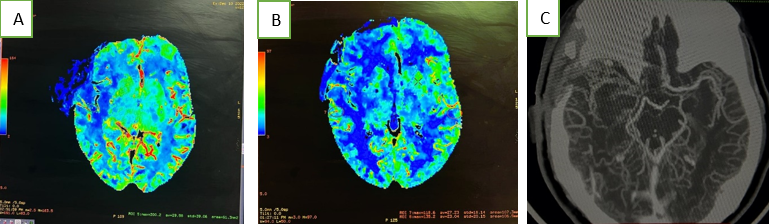
A 50 years old female presented to emergency department with history of progressive loss of vision on right side, head ache, not able to speak, difficulty in using left upper and lower limb and difficulty in walking for 10 days duration. She was apparently normal before 10 days then she noticed gradually decreased vision on her right eye in the form of blurring to complete loss of vision now. Head ache was right sided with constant dull aching in nature, not associated with vomiting. She was not able to use her left upper limb for her routine work and the weakness is progressively increasing. She was not able to walk due to the weakness of her left lower limb and able to walk only with support. She was not able to speak along with the onset of weakness. On examination patient was conscious, oriented, aphasic, no perception of light on right side with RAPD, left side vision was normal. On motor system examination on left side, upper limb power was grade 2/5 and lower limb was grade 3/5 with normal power on right side. MRI brain with MRA and MRV showed acute infarct seen in right basal ganglia, corona radiata and insular cortex (MCA territory). Contrast MRI shows decreased flow seen in cervical ICA, a giant thrombosed aneurysm measuring about 2.6*2.4 cm, arising from the supraclinoid segment of right ICA, the aneurysm shows mass effect over the right optic nerve and optic chiasma with no flow seen in aneurysm segment, minimal flow in right MCA and its cortical branches. DSA was done showed decreased filling of right ICA with no filling seen beyond clinoid segment with giant aneurysm in supraclinoid segment. Also shows no adequate flow across the A-com. In view of rapid progression of infarct, no flow beyond clinoid segment and no adequate flow across A-com, various treatment modality was discussed like aneurysm clipping with ICA reconstruction or double-barrel STA-MCA bypass surgery with parent vessel occlusion. Pros and cons of each surgical procedure was discussed in detail with the patient attenders and finally they were agreed to proceed with double-barrel STA-MCA bypass procedure. patient underwent double-barrel STA-MCA bypass surgery in which both branches of Right STA dissected to adequate length, right fronto temporal craniotomy was done, right frontal branch STA anastomosed with temporal cortical branch of MCA (M4 segment) and parietal branch of STA anastomosed with M3 branches of MCA using 10-0 ethilon under microscope. Flow across the anastomosis checked using Intra op ICG. Surgery was uneventful and patient was shifted to ICU. On post operative day (POD) 1, patient was started on tablet aspirin and clopidogrel. From POD 3 onwards patient showed improvement in left limb power. Two weeks after the surgery patient started verbalising the words and power in the left upper limb improved to 3/5 and in lower limb 4/5. By the end of one month after the surgery patient’s speech was improved and able to verbalize normally. Power in left upper and lower limb became 4+/5 and started to walk without support. On follow-up CT perfusion scan showed good perfusion seen in right ganglio capsular region, right peri sylvian region and good flow across the STA to MCA anastomosis with complete occlusion of ICA proximal to thrombosed aneurysm, on follow-up MRI brain, the size of aneurysm was regressed in size to 2.2*2.0 cm.
Discussion
STA-MCA bypass technique was first described by Woringer and Kunlin,[12] Donaghy and Yasargil,[13] performed the first STA-MCA bypass surgery.Usually surgeons performes a single-anastomosis STA-MCA bypass with the parietal branch and it is considered as a low-flow bypass which is inadequate for flow replacement. The single barrel -bypass can only irrigate either the frontal or the temporal MCA territory, but a double-barrel bypass can provide a significant amount of flow immediately and directly to different recipient territories. The quantitative flow measurements demonstrated that double-barrel bypass has significantly higher overall flow compared with single-anastomosis bypass (69 mL/min vs 39 mL/min). These flows are dynamic, and donor vessels can enlarge or regress based on demand. Bypass flows can be monitored by angiography, quantitative MRA,[14] and, transcranial Doppler ultrasound.[15], [16] When equal flow deficiencies are in both the superior and inferior MCA divisions, and the double-barrel technique augments the flow better than the single barrel technique. Outcomes of double barrel bypass surgery can be assessed by CT perfusion. Double-barrel bypass was helpful in secondary stroke prevention.
The complication rates are similar to that of single-barrel bypas.In aneurysm management, bypass surgery has its role in challenging and failed endovascular treatment cases.[17] Moreover, it is a rescue treatment for symptomatic flow diverter thrombosis.[18] Perioperative antiplatelet therapy and eptifibatide administration reduce the risk of graft thrombosis.[19] Indocyanine green angiography (ICGA) and microvascular doppler sonography (mDS) are used for intraoperative flow assesment.[20]
Conclusion
Double barrel STA-MCA bypass surgery might be a better option of treatment for selected cases, particularly giant complex thrombosed aneurysms with cerebral ischemia where endovascular techniques not feasible. The high rates of intraoperative and postoperative patency support the feasibility of dual-anastomosis STA-MCA bypass for revascularization. The perioperative complications are same of that of single barrel technique. The functional outcomes at follow-up and perfusion improvement postoperatively support the efficacy of this technique.
Declaration of Patient Consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Source of Funding
None.
Conflicts of Interest
There are no conflicts of interest.
References
- R M Crowell, M G Yasargil. Experimental microvascular autografting. Technical note. J Neurosurg 1969. [Google Scholar]
- WJ Powers, WR Clarke, RL Grubb, TO Videen, HP Adams Jr, CP Derdeyn. Extracranial-intracranial bypass surgery for stroke prevention in hemodynamic cerebral ischemia: the Carotid Occlusion Surgery Study randomized trial. JAMA 2011. [Google Scholar]
- Ec/Ic Bypass Study, Group. Failure of extracranial-intracranial arterial bypass to reduce the risk of ischemic stroke. Results of an international randomized trial. N Engl J Med 1985. [Google Scholar]
- RM Starke, RW Crowley, M Maltenfort. Moyamoya disorder in the United States. Neurosurgery 2012. [Google Scholar]
- BA Gross, R Du. STA-MCA bypass. Acta Neurochir (Wien) 2012. [Google Scholar]
- JE Wanebo, JM Zabramski, RF Spetzler. Superficial temporal artery-to-middle cerebral artery bypass grafting for cerebral revascularization. Neurosurgery 2004. [Google Scholar]
- DW Newell, MD Vilela. Superficial temporal artery to middle cerebral artery bypass. Neurosurgery 2004. [Google Scholar]
- JK Liu, P Kan, SV Karwande, WT Couldwell. Conduits for cerebrovascular bypass and lessons learned from the cardiovascular experience. Neurosurg Focus 2003. [Google Scholar]
- P Vajkoczy. Revival of extra-intracranial bypass surgery. Curr Opin Neurol 2009. [Google Scholar] [Crossref]
- G Esposito, S Amin-Hanjani, L Regli. Role of and Indications for Bypass Surgery After Carotid Occlusion Surgery Study (COSS)?. Stroke 2016. [Google Scholar] [Crossref]
- J Cherian, V Srinivasan, P Kan, EAM Duckworth. Double barrel STA-MCA bypass: can it be considered “high-flow”. Oper Neurosurg (Hagerstown) 2018. [Google Scholar]
- E Woringer, J Kunlin. Anastomosis between the common carotid and the intracranial carotid or the sylvian artery by a graft, using the suspended suture technic. Article in French. Neurochirurgie 1963. [Google Scholar]
- RMP Donaghy, MG Yasargil. . Extra-intracranial blood flow diversion. Paper presented at: American Association of Neurological Surgeons 1968. [Google Scholar]
- T Kim, JS Bang, OK Kwon. Hemodynamic changes after unilateral revascularization for moyamoya disease: serial assessment by quantitative magnetic resonance angiography. Neurosurgery 2017. [Google Scholar]
- C Hadley, R North, V Srinivasan. Elective sonolucent cranioplasty for real-time ultrasound monitoring of flow and patency of an extra- to intracranial bypass. J Craniofac Surg 2020. [Google Scholar]
- AR Flores, VM Srinivasan, J Seeley. Safety, feasibility, and patient-rated outcome of sonolucent cranioplasty in extracranial-intracranial bypass surgery to allow for transcranioplasty ultrasound assessment. World Neurosurg 2020. [Google Scholar] [Crossref]
- MD Vilela, DW Newell. Superficial temporal artery to middle cerebral artery bypass: past, present, and future. Neurosurg Focus 2008. [Google Scholar] [Crossref]
- LA Lanterna, A Lunghi, C Brembilla, P Gritti, C Bernucci. Extraintracranial Bypass as a Rescue Therapy for Symptomatic Flow Diverter Thrombosis. Case Rep Neurol Med 2015. [Google Scholar] [Crossref]
- V Stambolija, G Mrak, M Lozic, J Ljevak, M Miklic Ublic, M Scap. Intraoperative Eptifibatide Administration During Urgent Arterial Bypass in Neurosurgery. World Neurosurg 2017. [Google Scholar] [Crossref]
- J Woitzik, P Horn, P Vajkoczy, P Schmiedek. Intraoperative control of extracranial-intracranial bypass patency by near-infrared indocyanine green video angiography. J Neurosurg 2005. [Google Scholar] [Crossref]
How to Cite This Article
Vancouver
Venkatesan S, Balaji S. Double-barrel STA-MCA bypass for a giant thrombosed supraclinoid ICA aneurysm with gangliocapsular infarct – A case report [Internet]. IP Indian J Neurosci. 2025 [cited 2025 Sep 06];9(3):165-169. Available from: https://doi.org/10.18231/j.ijn.2023.032
APA
Venkatesan, S., Balaji, S. (2025). Double-barrel STA-MCA bypass for a giant thrombosed supraclinoid ICA aneurysm with gangliocapsular infarct – A case report. IP Indian J Neurosci, 9(3), 165-169. https://doi.org/10.18231/j.ijn.2023.032
MLA
Venkatesan, S., Balaji, S.. "Double-barrel STA-MCA bypass for a giant thrombosed supraclinoid ICA aneurysm with gangliocapsular infarct – A case report." IP Indian J Neurosci, vol. 9, no. 3, 2025, pp. 165-169. https://doi.org/10.18231/j.ijn.2023.032
Chicago
Venkatesan, S., Balaji, S.. "Double-barrel STA-MCA bypass for a giant thrombosed supraclinoid ICA aneurysm with gangliocapsular infarct – A case report." IP Indian J Neurosci 9, no. 3 (2025): 165-169. https://doi.org/10.18231/j.ijn.2023.032
