- Visibility 65 Views
- Downloads 12 Downloads
- DOI 10.18231/j.ijn.2023.020
-
CrossMark
- Citation
A case series of posterior circulation ischaemic stroke following viper snake bite
Introduction
Snakebite is a health hazard often faced by the rural population in tropical and subtropical countries with heavy rainfall and humid climate.[1] Snakebite is a common cause of morbidity and mortality in India. According to older estimates, approximately 2,00,000 fall prey to snake bites annually in India, with an estimated mortality ranging from 20,000 to 50,000 cases. Mohapatra et al. estimated 45,900 annual snakebite deaths nationally or an annual age-standardized rate of 4.1/100,000, with higher rates in rural areas (5.4) and with the highest rate in the state of Andhra Pradesh (6.2).[2]
Viperidae species consisting of Russell's viper (Daboia russelli) is India's most common cause of fatal snake bites.[3], [4] Viper bites are more common in South India than in North India.[4] The common clinical characteristics of viper bite include local cellulitis, renal failure, and systemic hemorrhagic manifestation, including intracranial and subarachnoid hemorrhage. The neurological manifestations are mostly confined to the cranial nerves, commonly causing ptosis and external ophthalmoplegia. Only a few authors have described ischemic infarction following viper envenomation.[5], [6], [7], [8], [9] In all of these cases, ischemic infarction involved the anterior circulation. Only five cases of posterior circulation infarcts after snakebite have been reported to date,[10], [11], [12], [13], [14] out of which only three have been documented after a viper bite.[12], [13], [14] Paraplegia following snake bite is a rarely reported manifestation, only reported once previously.[15] We report 5 cases with the unusual presentation of posterior circulation infarct following a viper snake bite.
Case Report
Patient A
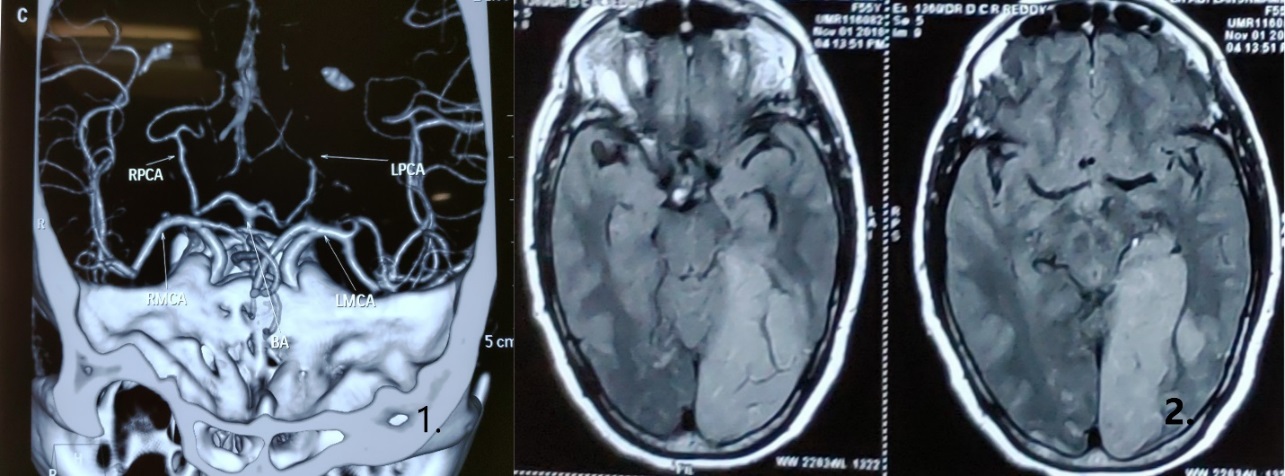
A previously healthy 50-year-old woman was bitten by a snake on her left leg while working in a paddy field. She presented to a nearby primary health centre with progressively worsening sensorium, bilateral lower limb weakness, and respiratory distress. Her left foot had two deep bite marks with local swelling, redness, and cellulitis. Onlookers identified the snake as a Viper. She was intubated, put on ventilator support, and administered 20 equine polyvalent anti-snake venom vials. Her GCS was E2VtM3. Platelet counts, Bleeding time, clotting time, and APTT were within normal limits. Intracerebral haemorrhage was suspected, and CT Brain showed an evolving left PCA territory infarct. MRI Brain done 24 hours later confirmed it to be Left PCA territory Infarct (Figure 1 (1). CT Angiogram showed a significantly attenuated left-sided posterior cerebral artery from the P2 segment. (Figure 1(2)). She was started on anti-platelets, statins, Low molecular weight heparin, and antibiotics. She developed severe pulmonary oedema and died two days later.
Patient B
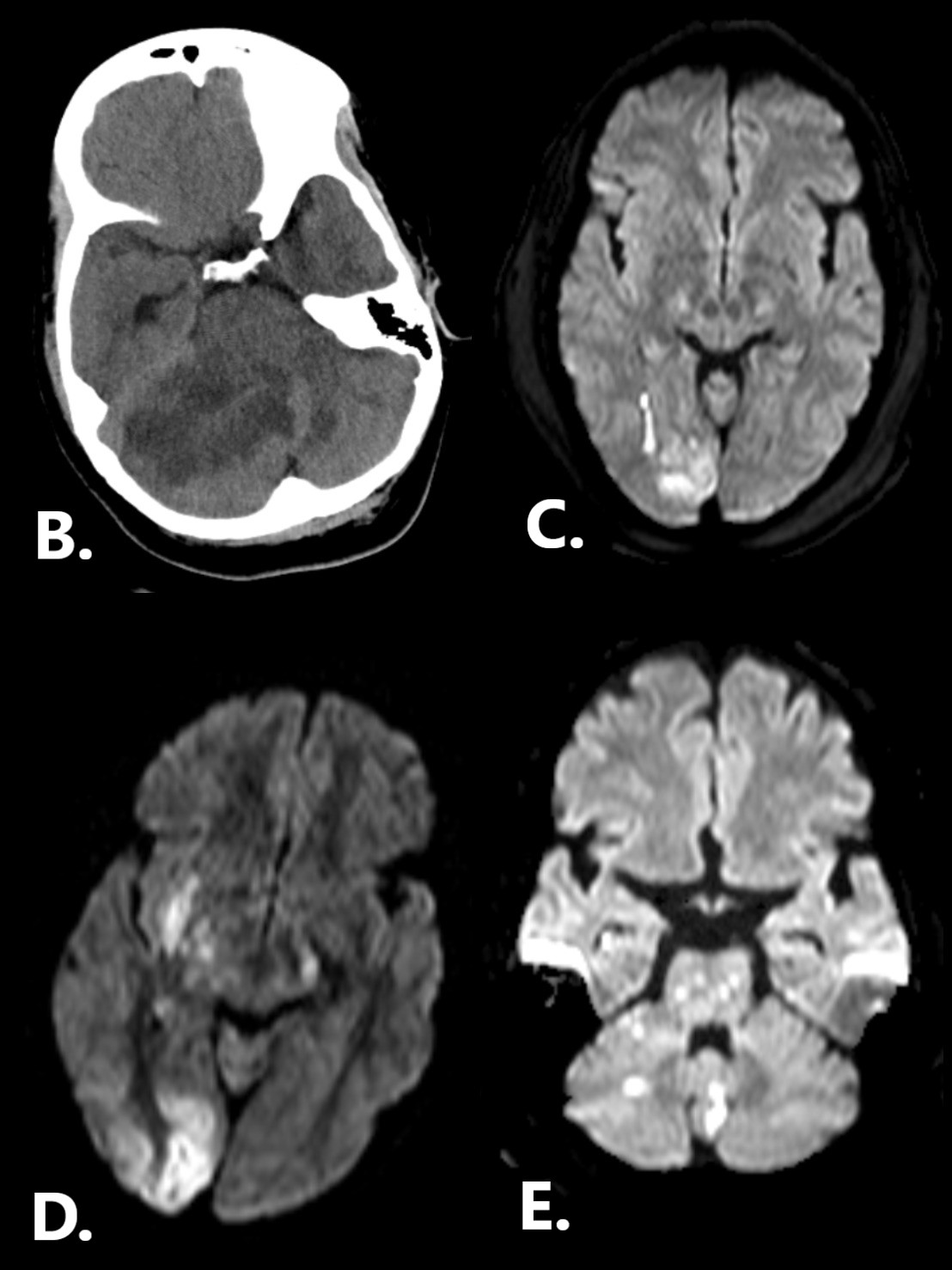
A 37-year-old lady with no known comorbidities presented with a viper snake bite over her right calf, following which she developed local swelling and pain over the right leg. She was started on ASV but developed an allergic reaction; hence it was stopped. She had seizures, and thus CT brain revealed a large right cerebellar infarction with ventricular dilatation ([Figure 2]B). The platelet count was low. It was corrected, and she underwent decompressive posterior fossa craniotomy because of the mass effect. She made a good recovery and was discharged without any sequelae.
Patient C
A 54-year-old male had a viper snake bite while working on the farm on a rainy day. He presented to the hospital in an unconscious state and was intubated. The platelet count was 28,000. Urea and creatine were elevated, and he was started on dialysis. MRI showed multiple infarcts – Right PCA, Left MCA territory lacunar infarcts ([Figure 2]C). He was tracheostomised. He had a gradual recovery.
Patient D
A fifty-eight-year-old gentleman presented with a history of snakebite over the left leg. After half an hour, he was found to be unresponsive. He was started on 15 vials of ASV (within 2 to 3 hours), and he was intubated given the low GCS. There was bleeding from the snakebite site. INR was 3.68, and he was transfused 4 units of FFP.CPK was elevated (3717 U/L). D-Dimer was 4.19 g/L. The platelet count was 6,04,000. MRI brain showed acute infarct predominantly involving cerebral cortices in the right parieto-occipital posterior frontal regions, capsulo-ganglionic region, caudate nucleus, hippocampal region, bilateral thalamus, and both cerebellar cortical grey mater ([Figure 2]D). He recovered over ten days and was extubated. He had residual mild lower limb weakness.
Patient E
A 55-year gentleman with a viper bite presented to the hospital with seizures, hemiparesis, and bleeding manifestations. He received 11 vials of ASV and was intubated because of prolonged status epilepticus. Baseline investigation revealed prolonged bleeding time (>15 mins), clotting time (>60 mins), leucocytosis, and elevated CPK(3571 U/L). He required increasing doses of inotropes. MRI Brain showed multiple acute infarcts in the brainstem, Cerebellum, and right caudate ([Figure 2]E). There was no improvement of consciousness, and as brainstem reflexes were absent, he was declared brain dead.
|
Patient |
Age |
Sex |
Location of stroke |
Lab Findings |
Outcome |
|
A |
50 |
Female |
Left PCA |
Normal |
Death |
|
B |
37 |
Female |
Right cerebellar infarct with mass effect and Hydrocephalus |
Thrombocytopenia |
Underwent posterior fossa decompression surgery- recovery |
|
C |
54 |
Male |
Right PCA + Left MCA lacunar |
Thrombocytopenia Elevated urea, creatinine, CPK |
Sequalae- Hemianopia |
|
D |
58 |
Male |
Right PCA+ Right gangliocapsular+ Bilateral thalamus |
INR- 3.68, elevated CPK Thrombocytopenia |
Sequalae- Lower limb weakness |
|
E |
55 |
Male |
Brainstem, Cerebellum, right caudate |
Elevated bleeding time, clotting time and CPK, Thrombocytopenia |
Death |
|
Case Reports |
Age sex |
Presentation |
Snake |
Labs |
Diagnosis |
Outcome |
|
Krishnan et al [10] |
14 M |
Ptosis + Altered sensorium. Unequal & Sluggish pupils, Hypotonia, Plantar- Extensors |
Not Known |
BT,CT, Platelets - Normal |
CT Brain - Bilateral Cerebellar +Rt Occipital Infarct with mass effect |
Death |
|
Gouda et al. [12] |
40 F |
Altered sensorium, GCS 9/15 Hypotonia, Plantar-Extensor |
Viper |
PT, APTT prolonged INR-4.44 CPK Elevated |
CT & MRI – B/L cerebellum + Occipital Infarct |
Recovered with residual gait ataxia |
|
Gunchan et al. [11] |
36 M |
Seizures, Anisocoria, Gaze palsy, Hypotonia, plantars Extensor |
Not Known |
Normal coagulation profile |
MRI- Left Cerebellum + Bilateral occipital+ Bilateral Thalamus |
Recovered |
|
Gupta et al. [13] |
48 F |
Hematuria, hematemesis. Drowsiness (3rd day), Hypotonia, Plantar extensor |
Viper |
Prolonged BT, CT Xray – Pulmonary edema |
CT- Left Cerebellum with mass effect + Hydrocephalus |
External Ventricular Drain Recovered |
|
Deepu et al. [14] |
48 F |
Altered sensorium, respiratory distress GCS 10 |
Viper |
Normal coagulation |
Ct- Right Cerebellum with mass effect and midline shift |
Death |
Discussion
The most typical cause of snakebite in India is due to the Viper species. [3], [4] Clinical manifestations depend on the severity of envenomation. Viper venom contains procoagulant arginine ester hydrolase, an enzyme similar to thrombin that clots fibrinogen and aggregates platelets, forming intravascular fibrin microthrombi. [16] This causes consumptive coagulopathy and leads to bleeding. The viper venom also contains several anticoagulant proteins that activate factors V, IX, X, XIII or cause fibrinolysis and hemorrhage.[17] These hemorrhagins and hemolysins cause damage to the vessel wall and, along with the coagulation defects, may result in severe bleeding. Due to this 'pro-bleeding' background, the common neurological manifestations are due to intra-cerebral or subarachnoid haemorrhage, with a rare occurrence of ischaemic infarctions. Mosquera Et al.[18] have reported strokes in only 8 out of the 309 patients (2.6%) in their series of snake bites. Of these, 7 were hemorrhagic strokes, and only one was ischaemic.
Previous studies have proposed the following mechanisms for the occurrence of infarctions.
Hypotension - Sweating, vomiting, reduced fluid intake, and bleeding tendencies lead to hypovolemia and hypotension. Loss of vasomotor tone due to viper toxin leads to hypotension. This hypotension leads to poor perfusion and watershed infarcts.
Hypercoagulability – due to the procoagulant activity of viper venom or consumptive coagulopathy causing procoagulant state.
Endothelial injury - due to toxic vasculitis can lead to thrombosis.
Cardiotoxicity – Dysarrythmia due to the effect of viper venom may lead to cardiac thromboembolism.
The infarcts in our patients are not in the classical watershed territory and therefore do not suggest hypotension as a cause. Bleeding and Clotting time was normal and ruled out coagulopathy as a cause in Patient A. The possible reason for infarct in this patient's posterior circulation is toxic vasculitis caused by injury to the endothelium by snake venom toxin. Only the posterior circulation is affected, and the anterior circulation is spared. Ct Angiogram ruled out any pre-existing abnormality in the posterior circulatory blood vessel wall that could be considered as a cause for the infarct. However, we do not have DSA studies to prove this. Previous case reports have discussed similar cases where the patient died despite normal coagulation parameters. [10], [14] Patient A also had paraplegia that could be explained as an MRI of the spine could not be done. Singh et al.[15] have reported a case of paraplegia following a viper bite due to dorsal spinal cord involvement.
Four of the five patients had some form of coagulopathy (80%). All Four had thrombocytopenia at presentation, out of which two (Patients D & E) had both thrombocytopenia and elevated clotting time suggestive of consumptive coagulopathy (DIC) as the cause of the infarct. The other two patients (B, C) had only thrombocytopenia with normal clotting time suggestive of early/mild DIC; hence a combination of toxic vasculitis and DIC could explain the infarct.
In our series, two patients presented with seizures despite having only posterior fossa infarcts (B, E). Previously Guncha et al.[11] have reported a similar patient who presented with seizures. Most patients in our series and literature have presented with altered sensorium, drowsiness, and local limb swelling. Altered sensorium after a snake bite may be related to the vasculitis caused by the venom resulting in cerebral oedema or toxic encephalopathy. Thus it may be difficult to diagnose a patient with a posterior circulation stroke based on clinical presentation alone, and a high degree of suspicion is needed.
The high mortality rate among patients with posterior circulation infarcts after snake bites has been documented in the literature. In our series, mortality was 40%. This corresponds to earlier case reports.[10], [11], [12], [13], [14] The clinical outcome is better in patients with supratentorial infarcts following snake bite than posterior fossa infarcts.[5], [6], [7], [8], [9] This may be due to the rapid rise of intracranial pressure associated with posterior fossa infarcts. Patient B underwent a Decompressive craniectomy due to the mass effect and recovered well after normalisation of ICP. Deepu et al.[14] reported a patient presenting with a cerebellar infarct 20 hours after a snake bite. Here despite surgery, the patient died. This could be due to the late presentation and higher envenomation.
This case series emphasises the need for high suspicion of posterior circulation infarcts following snake bite as they can be fatal. Early diagnosis and reduction of ICP help decrease mortality. Hydration, blood pressure, and CVP should be kept optimal in all snakebite patients. ASV, if indicated, administered early may help prevent coagulopathies and prevent infarcts. Thomas et al. [19] discussed that thrombotic complications were prevented by administering ASV within 6 hours. Local infection should be treated aggressively with antibiotics and antiseptic dressings. Normal platelet counts and coagulation profiles may conceal the early stages of DIC. Snakebite should be considered an essential differential in young patients with stroke, especially in rural areas.
Conclusion
Posterior Circulation Stroke is a rare but lethal complication after Russel Viper's snake bite. Due to the non-specific presentation, a high degree of suspicion is necessary to diagnose it. Early diagnosis and reduction of ICP help in improving survival. Snakebite should be considered an important differential in young patients with stroke, especially in rural areas.
Conflict of Interest
None.
Source of Funding
None.
References
- G Mohfw. Management of Snake Bite - Standard Treatment Guidelines; Govt. of India. 2016. [Google Scholar]
- B Mohapatra, DA Warrell, W Suraweera, P Bhatia, N Dhingra, RM Jotkar. Snakebite Mortality in India: A Nationally Representative Mortality Survey. PLOS Neglected Trop Dis 2011. [Google Scholar] [Crossref]
- B Ganneru, BS Rao, G Brunda, RB Sashidhar. Epidemiological profile of snake-bite cases from Andhra Pradesh using immunoanalytical approach. Indian J Med Res 2007. [Google Scholar]
- . 4.Regional office for south East Asia; World Health Organisation. Guidelines for the Management of Snakebites. 2nd Edn.. 2016. [Google Scholar]
- JMK Murthy, LT Kishore. Case Report, Cerebral Infarction After Envenomation by Viper. J Computer Assisted Tomography 1997. [Google Scholar]
- R Bashir, J Jinkins. Cerebral Infarction in a Young Female Following Snake Bite. Stroke 1985. [Google Scholar] [Crossref]
- JN Panicker, S Madhusudanan. Cerebral Infarction in a Young Male Following Viper Envenomation. J Assoc Physicians India 2000. [Google Scholar]
- SK Narang, S Paleti, MA Azeez Asad, T Samina. Acute Ischemic Infarct in the Middle Cerebral Artery Territory Following a Russell’s Viper Bite. Neurology India 2009. [Google Scholar]
- VK Pothukuchi, A Kumar, C Teja, A Verma. A Rare Case Series of Ischemic Stroke Following Russell’s Viper Snake Bite in India. Acta Med Indones 2018. [Google Scholar]
- M Krishnan, K Thruvarutchelvan, S Sivakumar. Posterior Circulation Stroke in a Young Male Following Snake Bite. J Assoc Physicians India 2008. [Google Scholar]
- G Paul, BS Paul, S Puri. Snake bite and stroke: Our experience of two cases. Indian J Crit Care Med 2014. [Google Scholar] [Crossref]
- S Gouda, V Pandit, S Seshadri, R Valsalan, M Vikas. Posterior circulation ischemic stroke following Russell's viper envenomation. Ann Indian Acad Neurol 2011. [Google Scholar] [Crossref]
- S Gupta, A Tewari, V Nair. Cerebellar Infarct with Neurogenic Pulmonary Edema Following Viper Bite. J Neurosci Rural Pract 2012. [Google Scholar] [Crossref]
- D Deepu, H Hrishikesh, S Suma, Z Zoya. Posterior fossa infarct following Viper bite: a paradox. J Venom Anim Toxins incl Trop Dis 2011. [Google Scholar] [Crossref]
- S Singh, A Chattopadhya, A Sud, A Wanchu, P Bambery. Acute Paraplegia Following Viper Bite. J Assoc Physicians India 2002. [Google Scholar]
- S Gupta, A Tewari, V Nair. Cerebellar Infarct with Neurogenic Pulmonary Edema Following Viper Bite. J Neurosci Rural Pract 2012. [Google Scholar] [Crossref]
- M Bhojaraja, MM Prabhu, W Stanley, S Sanket, VKN Marimuthu, ST Kanakalakshmi. Snake Bite: An Unusual Cause of Ischaemic Stroke. Australasian Med J 2012. [Google Scholar] [Crossref]
- A Mosquera, L A Idrovo, A Tafur, O H Del Brutto. Stroke following Bothrops spp. snakebite. Neurology 2003. [Google Scholar] [Crossref]
- L Thomas, B Tyburn, B Bucher, F Pecout, J Ketterle, D Rieux. Prevention of thromboses in human patients with Bothrops lanceolatus envenoming in Martinique: failure of anticoagulants and efficacy of a monospecific antivenom. Research Group on Snake Bites in Martinique. Am J Trop Med Hyg 1995. [Google Scholar]
