- Visibility 145 Views
- Downloads 21 Downloads
- DOI 10.18231/j.ijn.2023.017
-
CrossMark
- Citation
Intraaxial epidermoid cyst: Report of a rare case and review of literature
Introduction
Epidermoid cysts were first discovered and described in a French medical school by an artist in 1807.[1] Later in 1829, the first full description was given by a French Pathologist Cruveilhier. [2] In 1922, for the first time this tumour was redefined by Cushing as epidermoid cyst of Central Nervous System. [3]
These cysts are benign slow growing extra-axial tumours that account for ∼1% of all intracranial tumours, [4] frequently discovered at the cerebellopontine angles and parasellar regions, insinuating between brain structures. The other common locations include parapontine, parasellar, middle cranial fossa, diploe, and spinal canal. Amongst the intracranial epidermoid cysts, intra-axial epidermoid cysts that are purely within brain parenchyma are even rarer (< 1%) [5] and very few cases have been reported till date. [6]
The authors discuss this case report for its exceptional location along with the clinical presentation, radiological imaging, differential diagnoses and the surgical management based on the review of the literature.
Case Report
A 25-year-old male had suffered from headache for 4years, followed by two episodes of seizures over a span of 1 month. On admission, no neurological deficits were noted. Non-Contrast Computed Tomography (NCCT) showed a well circumscribed intra-axial hypodense lesion in right frontal lobe causing effacement of the frontal horn of lateral ventricle [[Figure 1]a].
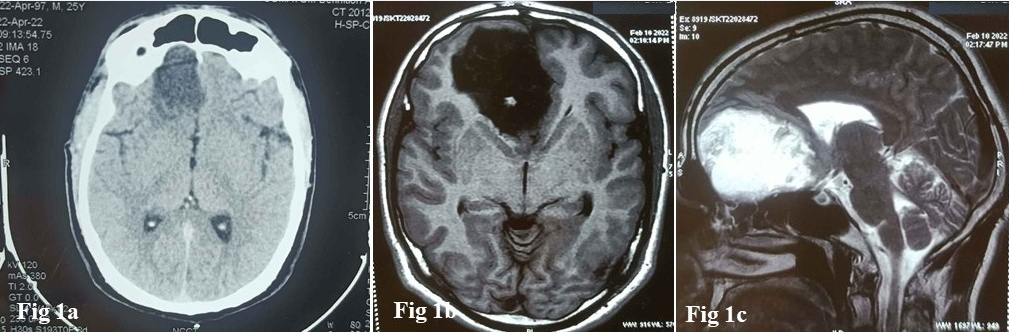
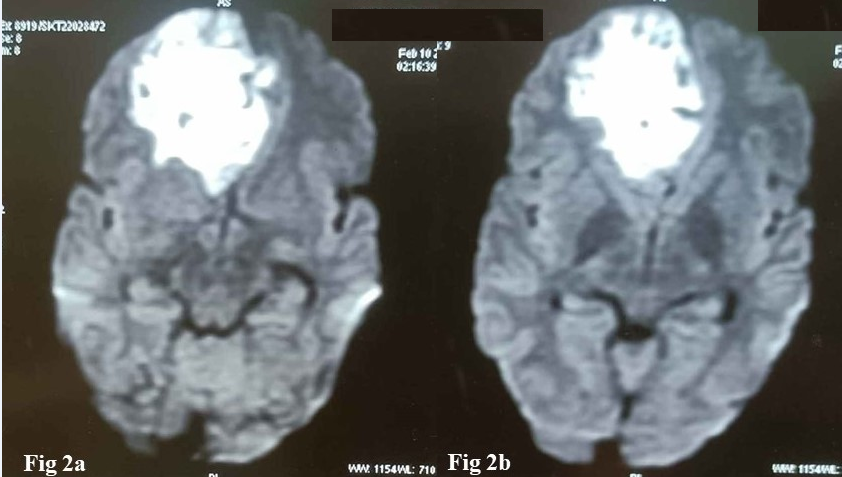
MRI studies showed a mass located in the right frontal lobe. The mass was distinctly intra-axial with a thin rim of cerebral parenchyma surrounding the mass from all sides. The mass was hypointense on T1-weighted images, hyperintense on T2-weighted images [[Figure 1]b,c] and hyperintense on diffusion weighted images (DWI) [[Figure 2]]. Radiologically, it was a solid cystic mass and possibilities of dermoid cyst vis-a-vis lipoma were considered. The patient underwent a right frontal craniotomy. After opening the dura, no abnormalities were detected on the cortical surface. The tumour was exposed through a cortical incision. The intraoperative findings revealed an abnormal mass with a pearly white glistening appearance and loose consistency. The cystic component was first aspirated. It consisted of milky fluid and was aspirated without any resistance. Subsequently, the solid portion was removed which was avascular soft and suckable. Attempts at total removal of the cyst wall were unsuccessful and abandoned due to its adherence to the surrounding parenchyma.
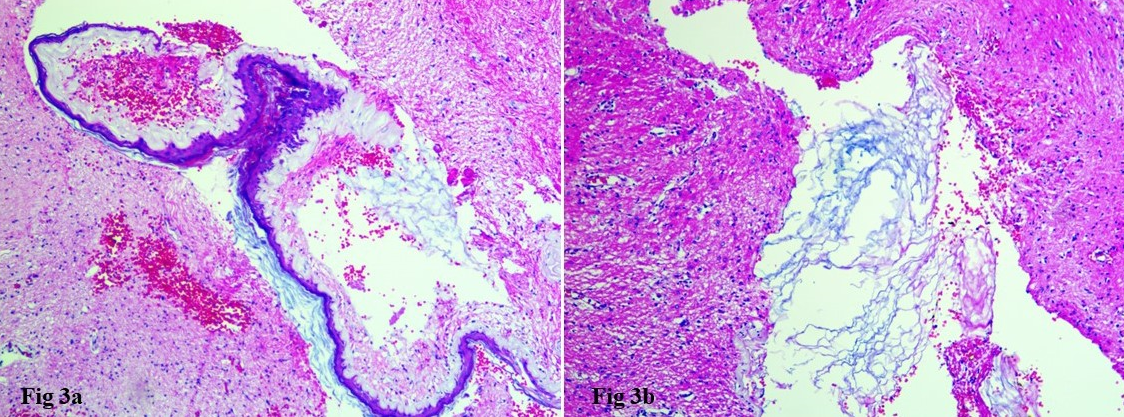
A perioperative diagnosis of a cyst was made and the tissue sent for histopathological examination. On gross inspection, the specimen consisted of multiple whitish, soft tissue pieces admixed with flaky material, which were subjected for crush cytology and paraffin section study. The cytological intraoperative smear preparations stained by Haematoxylin & Eosin (HE) and rapid Toluidine Blue method showed keratin flakes only. The remaining tissue was fixed in 10%buffered formalin and routinely processed. HE stained sections showed a cyst wall lined by stratified squamous epithelium surrounded by the glial tissue [[Figure 3]a]. Cystic cavity was filled with abundant lamellated keratin flakes, which were also found embedded in the glial tissue [[Figure 3]b]. Histopathological diagnosis of an intra-axial epidermoid cyst was made. The postoperative course was uneventful, and the patient was discharged. Follow up (12 months) is being done, and there are no signs of recurrence to date.
Discussion
Intracranial epidermoid cysts (ECs) are rare congenital lesions, postulated to develop from the sequestrated ectodermal cell rests during the third and fifth weeks of intrauterine life. Intraaxial epidermoid cysts are also supposed to result from the same pathogenesis as embryologically, these are derived from ectodermal inclusions during neural tube closure from the third to the fifth weeks of embryogenesis.[7] The final location possibly depends on the timing of sequestration, as suggested by Rengachary et al[8] that epidermoid cysts do occur because of an aberration of epithelial rests or congenital sequestration of ectodermal elements that occurs between the third and fifth weeks of intrauterine life when the medullary groove closes. Sequestration usually occurs either in the midline or in relation to optic and otic vesicles. Similarly, Chandler et al later[9] suggested that as a result of neural tube closure and division from the cutaneous ectoderm, remaining cells are left on the inner or outer surface, or within the neural tube ectoderm. This explains the occurrence of epidermoid cysts intraventricularly, on the surface, or within the brain.
As per the existing literature, most of the patients are of young or middle age and men are affected more than women (M: F= 1.6:1). Clinical manifestations depend on the tumor location, including dizziness, hearing loss, tinnitus, gait disruption, trigeminal neuralgia, diplopia, vision impairment, lethargy, and headache. Rupture of an epidermoid cyst is a rare but severe complication that may lead to meningitis and hydrocephalus.[10]
On computed tomographic (CT) scans, the typical appearance is that of a non-enhancing and hypo-attenuating extra-axial mass. Calcifications may be seen within these tumors in 10-25% of cases. Rarely these may appear hyper-attenuated on CT scans and show high signal intensity on T1-weighted images and low signal intensity on T2-weighted images due to high protein content therefore also referred to as white epidermoids.[11] Magnetic resonance imaging (MRI) is the best modality for evaluating these cysts. Characteristically, they are either isointense or slightly hyperintense relative to CSF on T1- and T2-weighted images. Most of the epidermoids have a typical appearance however their signal intensity may vary depending on the relative amounts of cholesterol and keratin within the tumour and seldom show contrast enhancement.[12] The radiological differential diagnoses of an epidermoid cyst includes Arachnoid cyst, Dermoid cyst, Colloid cyst, Rathke cleft cyst, Craniopharyngioma, Hydatid cyst, Neurocysticercosis, Neurenteric cyst or Cyst abscesses. FLAIR findings, DWI sequences and the location of the lesion helps in differentiating the typical epidermoid cyst from the other lesions.[10]
Histopathology of epidermoid cysts has typical diagnostic features comprising of a cyst wall showing keratinizing squamous epithelium. Cystic cavity is always filled with lamellated keratin. Foamy histiocytes, foreign-body giant-cells and cholesterol clefts with focal granulomatous inflammation are the other usual components.
Intra axial epidermoids are generally benign and therefore complete excision is the definitive treatment. In cases where the capsule is densely adherent to vital structures, leaving behind a part of the capsule is justified and safe.[13] Recurrences are rare. The location of the epidermoid cyst and the time taken from onset to diagnosis are the important factors for the prognosis than the size of tumor.
Conclusion
Intra-axial epidermoid cysts are very rare lesions. To the best of our knowledge, only few cases have been reported till date. Although simple to diagnose perioperatively and on histopathology, epidermoid cysts at unusual sites can pose a preoperative radiologic dilemma even with the current technology available. In this purview, epidermoids needs to be considered in the differential diagnosis of intraparenchymal lesions clinically and on radiology. Surgery is the only effective treatment, and its goal should be the radical resection of the lesion to avoid their recurrence. When radical resection of tumor capsule poses too great a risk, subtotal resection can be a wise option. The overall outcome is good in view of benign nature of the disease.
Conflict of Interest
None.
Source of Funding
None.
References
- FC Grant, GM Austin. Epidermoids: clinical evaluation and surgical results. Neurosurg 1950. [Google Scholar] [Crossref]
- J Cruveilhier. Anatomie Pathologique du Corps Humain. 1829. [Google Scholar]
- H Cushing. A large epidermal cholesteatoma of the parietotemporal region deforming the left hemisphere without cerebral symptoms. Surg Gynecol Obstet 1922. [Google Scholar]
- AG Osborn, MT Preece. Intracranial cysts: radiologic pathologic correlation and imaging approach. Radiology 2006. [Google Scholar]
- A Kumar, VP Maurya, S Kanjilal, KS Bhaisora, J Sardhara, KK Das. Clinicoradiological Features and Treatment Outcome of Supratentorial Intraparenchymal Epidermoid Cyst: A Report of Five Cases and Literature Review. J Neurosci Rural Pract 2021. [Google Scholar] [Crossref]
- NM Nagaraj, PR Bysani, S Dutta, SA Nagesh, BN Nandeesh, BS Pai. Rare case of atypical intraparenchymal epidermoid cyst. J Curr Res Sci Med 2018. [Google Scholar]
- T Kaido, A Okazaki, S-I Kurokawa, M Tsukamoto. Pathogenesis of intraparenchymal epidermoid cyst in the brain: a case report and review of the literature. Surg Neurol 2003. [Google Scholar] [Crossref]
- S Rengachary, PR Kishore, I Watanabe. Intradiploic epidermoid cyst of the occipital bone with torcular obstruction. Case report. J Neurosurg 1978. [Google Scholar] [Crossref]
- WF Chandler, SK Farhat, FJ Paufi. Intrathalamic epidermoid tumor. Case report. J Neurosurg 1975. [Google Scholar] [Crossref]
- MP Reddy, J Song, X Hong, Z Ma. Intracranial epidermoid cyst: characteristics, appearance, diagnosis, treatment and prognosis. Sci Lett 2015. [Google Scholar]
- WA Wagle, B Jaufmann, JE Mincy. Magnetic resonance imaging of the Fourth ventricular epidermoid tumors. Arch Neurol 1991. [Google Scholar] [Crossref]
- R Kachhara, RN Bhattacharya, VV Radhakrishnan. Epidermoid cyst involving the brain stem. Acta Neurochir (Wien) 2000. [Google Scholar] [Crossref]
- D Nagasawa, A Yew, M Safaee, B Fong, Q Gopen, AT Parsa. Clinical characteristics and diagnostic imaging of epidermoid tumors. J Clin Neurosci 2011. [Google Scholar] [Crossref]
