- Visibility 44 Views
- Downloads 9 Downloads
- DOI 10.18231/j.ijn.2023.011
-
CrossMark
- Citation
Rare case of double seronegative ocular myasthenia gravis and non-functional pituitary macroadenoma
Introduction
Myasthenia gravis (MG) is a disease of the neuromuscular junction characterized by an autoimmune response to cholinergic receptors. The range of symptoms and clinical manifestations of MG in different age group person make it difficult in diagnosis. The skeletal muscles of the classical presentation exhibit fluctuating weakness that gets worse with effort, especially in the muscles that are innervated by the motor nuclei of the brainstem. It can occur at any age and impacts over 700,000 individuals worldwide. Patients with MG experience excessive fatigue and can develop significant impairment. However, it is a treatable illness. MG may be fairly effectively managed in many people if the right diagnosis is obtained early and standardized therapy is provided.[1]
A proper diagnosis and plan of treatment are therefore vital. Acetylcholinesterase inhibitors, steroids, and immunosuppressant’s are indeed the main therapeutic choices. In 15% of MG patients, thymomas also exist, and tumor excision may improve MG symptoms. Clinicians must be aware of distinct symptom changes during the clinical course and conduct timely clinical testing to confirm the diagnosis in order to arrive at a precise diagnosis of MG.
Case Report
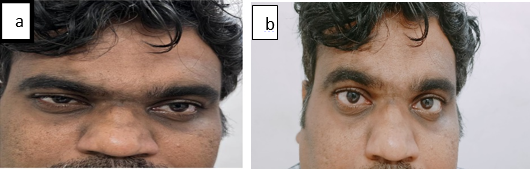
A 34 yrs old south Indian male patient was presented to our neurology clinic complaining of severe cephalgia, associated with ocular pain, dizziness, diplopia, ptosis of the unilateral right eye. These headache symptoms have started prior to 3 months of his visit he didn't have any speech disturbances voice was normal and had a history of generalized headache and cervical spondylosis which was treated symptomatically in other hospital and no as such increased icp values were noted at that time. On observation the patient had right eye unilateral ptosis which is fatigable and worsened at the end of the day.
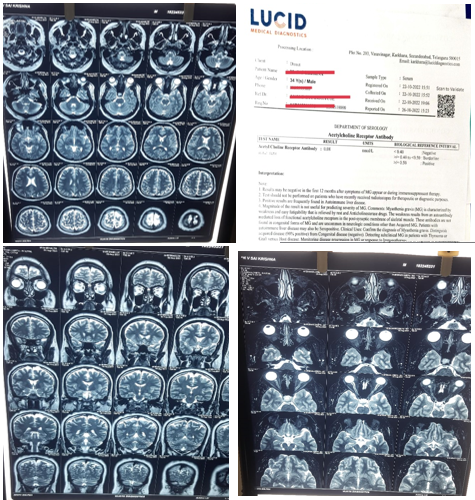
The patient was awake and even had a blood pressure of 110/70 mmHg, a 102-bpm pulse, a 16/pm respiratory rate, at 98% room air saturation, and a temperature of 36.5°C during the time of arrival. Physical examination demonstrated typical extraocular movements, normal pupils with light reflexes, and no aberrant neurological findings. The right lateral position, which was in the left rotatory position, was used to produce nystagmus from the supine position. Magnetic resonance imaging (MRI) was previously done s/o T2 flair hyperintense focal lesion is noted in the Sella with suprasellar extension, arising from the pituitary gland. The gland is not separately visualized from the lesion. Pituitary stalk is displaced towards left side. The lesion is in the midline and more towards right side .no obvious extensions into cavernous sinus is seen .no compression over optic chiasma/optic nerves-of concern for pituitary macroadenoma. Rest of the MR imaging is essentially normal, baseline laboratory tests were mentioned in [Table 1].
|
Test name |
Observed value |
Units |
Biological reference intervals |
|
Hemoglobin |
13.6 |
gms% |
13.0-17.0 |
|
Total RBC count |
4.64 |
mill/cumm |
4.5-5.5 |
|
Total WBC count |
8760 |
cells/cumm |
4000-11000 |
|
PCV/HCT |
41.0 |
vol% |
40-50 |
|
MCV |
88.3 |
fL |
76-96 |
|
MCH |
29.3 |
pg |
27-32 |
|
MCHC |
33.2 |
gm/dl |
31.4-55.5 |
|
Platelet count |
2.4 |
lakhs/cumm |
1.5-4.5 |
|
Neutrophils |
77 |
% |
40-75 |
|
Lymphocytes |
18 |
% |
20-40 |
|
Eosinophils |
02 |
% |
1-6 |
|
Monocytes |
03 |
% |
3-6 |
|
Basophils |
00 |
% |
0-1 |
|
E.S.R |
|
|
|
|
1ST hr |
17 |
mm/hr |
0-10 |
|
2ND hr |
42 |
mm/hr |
10-22 |
|
CRP |
9.89 |
mg/L |
<6.0 –Negative |
|
Acetylcholine receptor antibody |
0.08 |
nmol/L |
<0.40;Negative |
|
|
|
|
>/=0.50;Positive |
|
Anti-musk IFA |
<20 |
|
<20-Negative |
|
|
|
|
≥20 – Positive |
|
Serum prolactin |
8.09 |
ng/mL |
less than 20 |
|
Serum cortisol |
4.17 |
mcg/dL |
5 to 25 |
|
T3 |
118 |
ng/dl |
60-200 |
|
T4 |
8 |
µg/dL |
4.5-12 |
|
TSH |
4.8 |
mIU/ml |
0.3-5.5 |
|
Testosterone free |
7.95 |
pg/mL |
7.0-22.7 |
The presence of a pituitary macroadenoma which is non-functional was determined by laboratory tests and MRI characteristics. The patient was suggested for histopathology procedure and surgery to remove a trans-sphenoidal pituitary tumor. However, the patient was unwilling to have the procedure.After further examination, his repetitive nerve stimulation test was normal and all of his serum endocrine tests were negative. For his myasthenic symptoms, we recommended Pyridostigmine (60 mg/TID) and Prednisone (40mg/day); other complaints were treated symptomatically. His symptoms partially improved, and in the next visit which is after 20 days the patient complained about an abnormal increase in weight nearly 6-7 kgs so his prednisone was titred and azathioprine(50mg/od) was introduced. He responded to his prescriptions extremely effectively. His ptosis complaint improved.
We present a rare association between MG and a non-functional macroadenoma.
Two etiologiescontribute to the manifestations of pituitary adenomas. The first is the widespread impact of macroadenomas, which is likely probably caused by a patient's headache complaint. The second potential explanation involves hormones; in our instance, as the reports suggest that no evidence of increased hormone levels has been found, this explanation can be ruled out as non-functional. [2]
It is well known that MG has a high frequency of various autoimmune diseases, most notably thyroid disorders (5–10%), rheumatoid arthritis, systemic lupus erythematosus, polymyositis, and dermatomyositis. [3], [4]
Patient MRI OF BRAIN& ORBITS shows hyperintense focal lesion is noted in Sella with suprasellar extension, arising from the pituitary gland measuring- 13.7 x 15.5 x 16.9 mm (CC X TR X AP).Both his chest CT scan and CXR showed no signs of thymus problems and no significant sonological abnormality detected in our patient. [3], [4]
Thyroid function tests and a thyroid ultrasound, however, were both normal in our patient's situation. To test for muscular dystrophies, polymyositis, or any other myopathies, we additionally requested creatine kinase (CPK) which was also found to be normal.
Despite the fact that MG and pituitary macroadenoma is a common disorder in medical practice, their relationship in the literature is incredibly uncommon. In our study of the medical literature, we only discovered 9 published occurrences of an association between MG and pituitary adenomas. Prolactin-secreting adenomas were identified in five cases, in two cases, the GH-secreting adenoma was present and this case marks the third instance of a non-functional adenoma.
Small NFAs don't immediately manifest any symptoms. The pituitary gland, the brain, and the nerves could all be pressed against by the tumour’s as they grow. The majority of the time, they are not discovered until they are large enough to cause severe symptoms like Headaches, visual issues, including blurriness and loss of peripheral vision
Hormone issues may also result from the tumor pressing against your pituitary gland. You might have a malfunctioning gland. Your pituitary gland may not produce enough hormones if it isn't functioning properly. Hypopituitarism is a condition that you could develop. That may lead to: Fatigue, Weakness, Loss or increase of weight, sexual desire changes or infertility.
Alveolar endothelium and Ganglioneuroma were the 2 cases of non-functional pituitary adenomas.[5], [6] Negri and colleagues reported these occurrences in 1953 and 1976, respectively. Cahill et al. published the first description of the stimulating effect of PRL on the autoimmune activation of MG in 1980. [7], [8] Then, in 2006, Tsinzerling et al. reported two case reports and a cohort research examining the correlation between serum PRL levels and the severity of MG. [7], [8], [9] The function of PRL and possible therapeutic applications for MG were discussed by Harris et al. in 2013.[7], [9] The differential diagnosis of neurological symptoms in individuals with macroprolactinoma should be considered as MG, according to Zoli et al. in 2018.The literature is clear on the frequent link between endocrine dysfunction and myasthenia.
Improvement in symptoms with the administration of pyridostigmine suggests that this is the first instance of a pituitary non-functional macroadenoma with double seronegative ocular myasthenia gravis.
Due to seronegativity, our patient cannot be categorized as anything. despite the fact that he exhibits classic MG symptoms beneath the clinical manifestations of the disease. Axis dysfunction may contribute to the symptomatic manifestation of autoimmune diseases. Although surgical removal of the tumor frequently resulted in a marked improvement in the patient's condition, removal of the mass may also have been secondary to normalization of other hormone levels and may not have been entirely unconnected to MG per se.
As a result, no definite conclusions can be formed from a single instance, although we do provide it as a suggestion to other researchers.
Conclusion
It was quite unusual that the patient tested negative for both MuSK-Ab and AChR-Ab. With a better prognosis for the AChR-positive and MuSK-negative versions of the disease, recently published data have demonstrated that MuSK-positive and MuSK-negative MG are separate clinical entities. This highlights the predictive relevance of a patient's unique antibody profile in MG. There have only been a few other reported cases of concurrent MG and APS, and this suggests that some autoimmune disorders may be progressive. The pathogenesis and etiology of these related illnesses are poorly understood. In contrast to our situation. The relationship between MG and pituitary adenomas deserves additional investigation, despite the fact that it is uncommon, in order to determine the true frequency of this association and to investigate any potential underlying interactions between these two disorders. Contrarily, the presence of a headache in a myasthenic patient should draw attention to other potential causes, such as pituitary tumors.Since 15% of patients with generalized MG and 50% of those with ocular MG test negative for AchR and MuSK Ab, MG must still be considered in the differential diagnosis [9], [10] for patients who present with dysphagia. Early diagnosis leads to better results.
Conflicts of Interest
All contributing authors declare no conflicts of interest.
Source of Funding
None.
References
- DB Sanders, GI Wolfe, M Benatar, A Evoli, NE Gilhus, I Illa. International consensus guidance for management of myasthenia gravis Executive summary. Neurology 2016. [Google Scholar] [Crossref]
- BM Arafah, MP Nasrallah. Pituitary tumors: pathophysiology, clinical manifestations and management. Endocr Relat Cancer 2001. [Google Scholar] [Crossref]
- HH Yeh, YW Tung, CC Yang, JN Tung. Myasthenia gravis with thymoma and coexistence central hypothyroidism. J Chin Med Assoc 2009. [Google Scholar] [Crossref]
- DW Cahill, MS Sellman, M Saleman. Prolactinsecreting adenoma in a myasthenic patient. Neurosurgery 1980. [Google Scholar]
- J Lapresle, J Racadot, G Said. Thymoma and hypophyseal tumor associated with heterogeneous adenomatous proliferation and ganglioneuroma of Sella turcica. J Neurol Sci 1976. [Google Scholar]
- L Negri, G Weber. Telangiectasicthymoma with myasthenia gravis is associated with an unusual form of primary microadenoma so-called alveolar adenoepithelioma. Arch De Vecchi Anat Patol 1953. [Google Scholar]
- M Zoli, F Guaraldi, M Faustini, D Mazzatenta. Myasthenia gravis imitating pituitary apoplexy in macroprolactinoma. Hormones 2018. [Google Scholar] [Crossref]
- N Tsinzerling, R Pirskanen, G Matell, NM Zhulev, ML Chukhlovina, AK Lefvert. Raiser prolactin levels in myasthenia gravis: two case reports and a study of two patient populations. Acta Neurol Scand 2006. [Google Scholar] [Crossref]
- S M Harris, HM Leong, R Chowdhury, C Ellis, J Brennan, IN Scobie. Concomitant myasthenia gravis and macroprolactinoma: the immunomodulatory role of prolactin and its potential therapeutic use. Endocrine 2013. [Google Scholar] [Crossref]
- AE Dockry, S Colachis. Double-Seronegative Myasthenia Gravis (MG) in a Patient Presenting with Chronic Dysphagia: A Case Report. PM R 2020. [Google Scholar]
