Introduction
Traumatic brain injury (TBI) due to road traffic accidents, falls and assaults is increasing and is a major public health problem; often affecting young productive males with tremendous social, economic costs. CT imaging has become the mainstay for the initial investigation for patients with TBI as it readily diagnoses most traumatic conditions with minimal risk and time. With the regular use of CT imaging, finding of air in the intracranial cavity, called pneumocephalus is common and seen in about 3.9-9.7% of patients undergoing CT imaging for suspected TBI. 1, 2
Post-traumatic pneumocephalus (PTP) occurs due to fracture in the cranial vault or skull base causing abnormal communication between the cranial cavity and the paranasal sinuses, mastoid air cells or the external environment. Associated damage to dura, arachnoid and pia can lead to accumulation of air in different compartments of the cranial cavity. The PTP is generally absorbed over time but occasionally lead to meningitis, CSF rhinorrhea and tension pneumocephalus which may be life threatening and require specific emergency management.
The extent of PTP is variable from patient to patient and most have a good outcome. But, there is no published prospective study regarding the risk factors for the aforementioned complications and the clinical and radiological features associated with them. Hence this prospective study was conducted to assess the risk of development of complications associated with PTP depending on the pattern of skull fractures and the CT findings.
Material and Methods
This prospective observational study was conducted over a period of 14 months from 15 Nov. 2017 to 15 Jan. 2019 in Goa Medical College, a tertiary care center for the management of all kind of trauma patients including TBI. The study included all cases of TBI with CT head showing PTP along with there radiological findings, clinical course, complications and its management outcome. All patients were treated as per latest standard brain trauma foundation guidelines. The Institution ethical committee’s approval was obtained prior to commencement of the study.
Protocol followed for patients with PTP included in the study
Nursing in flat position.
Oxygen administration by mask, 5L/ min till radiological resolution.
Observation for features of raised ICP, CSF leak, neurological deterioration or meningitis.
Administration of Paracetamol for analgesia.
Administration of prophylactic anticonvulsants: phenytoin or levetiracetam; loading dose at admission followed by maintenance dose.
Protocol for management for CSF leak
Surgical management for PTP and CSF leak
Supra-orbital twist drill was done in one patient with TP.
Anterior cranial fossa repair and duroplasty with fascia lata graft and fibrin glue was done in 2 patients with delayed TP, rhinorrhea and meningitis. Both had comminuted bilateral depressed fracture of frontal bone extending to both frontal sinuses.
Endoscopic evaluation for active leak followed by repair of sphenoid defect with graft and fibrin glue as the location of defect was not clear on CT- cisternography in one patient.
Results
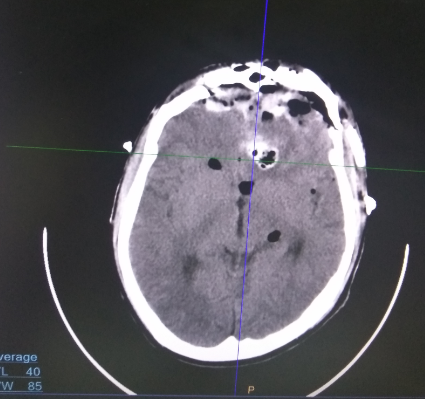
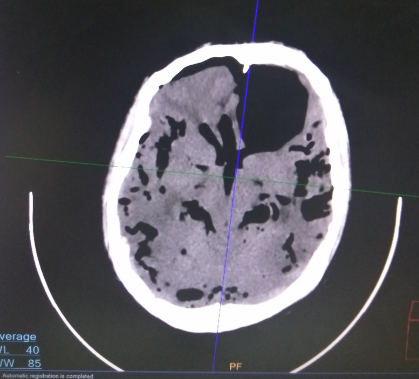
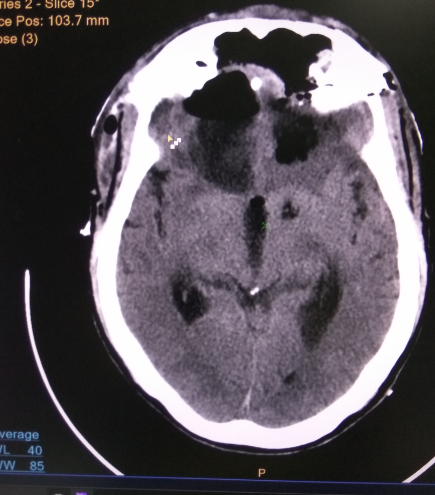
A total of 102 cases of post-traumatic pneumocephalus were included in the study. The mean age of the patients was 35.09 year (Range 1yr - 76yr; SD=16.14yr). Patients aged between 20-40years accounted for the majority (47.06%). Male: female ratio was 8.27: 1. The average length of stay during the first admission was 6.68 days (Range 1-56 days; Standard Deviation – 8.63 days). Motor vehicle accident was found to be major cause of PTP (79.41%). The Severity of TBI in patients with PTP in this study was: Mild TBI in 65%, Moderate TBI in 25% and Severe TBI in 10%. The most common site of post traumatic PTP was subdural (45.1%). Majority of the patients with PTP had focal PTP underlying the fracture segment (63.73%). Massive PTP was seen in 37 (36.27%) patients (28- multiple air bubbles; 2- isolated Mount Fuji sign; 7 -Mount Fuji sign with patchy distribution of air). In 44.12% cases of post traumatic PTP patients, CT scan showed multiple findings (combination of EDH, SDH, SAH, contusion or DAI). But in 25(24.51%) patients, only basal skull fracture and PTP were seen.
But only 4 patients developed features of tension pneumocephalus. Majority of the patients (30) had either isolated fracture frontal sinus (18) or multiple basal (12). The repeat CT scan showed a decrease in PTP in the majority of patients: 55.10% on 1st, and 70.53% on 2nd repeat scan respectively as shown in Table-3b. PTP remained the same in the first repeat CT in 35.71% of patients. Only 9.18% showed increment in PTP in the 1st repeat CT but remained clinically stable. One patient however had massive PTP with pressure effect on the adjoining brain and hence twist drill craniostomy and evacuation of PTP was done after initial CT prophylactically. Although the 1st elective repeat CT showed an increase in PTP in 9 patients, none of them had raised ICP features and were managed medically. One patient left the hospital against advice. The second repeat CT in the remaining 8 patients showed a decrease (6/8) or disappearance (1/8). In one patient it remained the same. Follow up CT imaging was not done in 5 patients who died and 2 who left the hospital against advice. 3 patients had delayed deterioration, with CSFR, signs of raised ICP and meningitis after several days; following which they underwent CT imaging and all had increase of PTP.
CSFR was seen in 13 patients: 11 had early CSFR within 72 hours after admission; 2 had delayed CSFR several days after admission and one had early and delayed CSFR which had stopped after first admission. 12 out of the 13 patients who developed CSFR had associated unilateral or bilateral comminuted depressed fracture of frontal sinus sometimes extending to the roof of orbit. In one patient, no fracture was evident in any of the CT images and diagnostic endoscopy showed a breach in the sphenoid sinus which was the site of CSF leak. The cranio-dural defect could be repaired in the same sitting. Majority (74.51%) of patients were treated conservatively. Most of operative interventions were done for associated EDH, SDH, Contusion or diffuse brain injuries. Overall 3 patients were operated for CSFR and TP, one patient was operated for TP and 22 patients were operated for associated cranial hematomass. 95 patients out of 102 were discharged; 5 patients died and 2 patients left against medical advice. All 5 patients who died suffered severe head injury with associated multiple CT findings.
Table 1
Demographic profile of Post-traumatic pneumocephalus patients.
Table 2
Anatomic and size based distribution of post-traumatic pneumocephalus.
Table 3
Associated cranio-cerebral injuries seen in patients with PTP
Table 4
Complications in patients with PTP.
Table 5
Management and outcome in patients with PTP
Discussion
PTP is fairly common and seen in 3.9-9.7% of patients undergoing investigations for TBI. 1, 2 Most of the patients have spontaneous absorption of the trapped air without serious sequelae. In some patients, there are serious complications like persistent CSFR, meningitis and TP. It would be important to know the clinical profile of those patients with PTP who are likely to develop such complications so that management can be specifically directed towards preventing them. However, the published literature on PTP comprises of only isolated case reports or retrospective studies and it is difficult to draw any inference from them. From our prospective single Centre cohort we attempted to study the general outcome of PTP and the identifiable risk factors for the occurrence of serious complications following it.
In our study of 102 consecutive patients diagnosed to have PTP over a period of 14 months from 15 November 2017 to 15 January 2019, 79.41% were following road traffic accidents and 89.2% were males. The severity of TBI in our patients was found to be: Mild in 62.8%; Moderate in 25.5% and Severe in 11.8%.
A study conducted earlier in our institute over a period of 13 months from January 2013 to January 2014, comprising 1862 TBI patients; showed the distribution of the severity to be Mild in 78.8%; moderate in 13.05% and Severe in 8.16%. 3 The patients with PTP as a subgroup appear to have significantly more severe TBI (Table 6 : p < 0.005). Though the two groups are separated by 4 years, they both are from the same community where the accident profile has remained the same and hence it is possible to extrapolate the comparison to the present cohort.
Comparison of the TBI severity pattern in the sub-group of patients with
PTP with a group comprising all patients with cranio-cerebral trauma.
Table 6
Comparison of the TBI severity pattern in thesub-group of patients with PTP with a group comprising all patients withcranio-cerebral trauma.
|
Severity |
Mild |
Moderate |
Severe |
chi square=15.6 Degree of freedom=2 Probability=0.000 |
|
Study1 (n=1862) |
1467 |
243 |
152 |
|
|
Study2 (n=102) |
64 |
26 |
12 |
PTP occurs in patients with skull fractures often involving the frontal areas or skull base. The consistent presence of fractures in all these patients indicates a higher impact force and the consequent increase in the severity of TBI. Further as the frontal bone requires a stronger impact force to sustain a fracture, those with frontal bone fractures may be expected to sustain more severe acceleration-deceleration forces with attendant damage to neuroparenchyma. 4
CT imaging is the preferred investigation for the diagnosis of TBI as it readily shows bone fractures and intracranial hematomas in the least possible time. PTP is readily diagnosed due to the intrinsic contrast difference that air has in comparison to the brain, bone and CSF. As the CT imaging is done at the initial presentation of the patient in the casualty, the presence of PTP can be identified early and the complications associated with it can be monitored for.
In our cohort, only patients with PTP on first CT, were included. Few graphical signs on imaging like Mount Fuji sign, peaking sign and multiple air bubble sign are indicators of significant PTP and due to their propensity to cause pressure effect on brain displacement or raised ICP, we have referred to such presence as massive PTP. 5. In this study, 37 patients had massive PTP, and unilateral or bilateral fracture of frontal sinus was noted in 57 (57/ 102). We found that fracture frontal sinus was a significant risk factor for massive PTP (Table 7 : p = 0.027) and CSF rhinorrhea (Table 8: p = 0.005).
Table 7
Assessment of frontal sinus fractures as risk factor for massive PTP
|
Patients |
With massive PTP |
Without massive PTP |
Chi-square=4.88 Degree of freedom=1 Probability=0.027 |
|
With frontal sinus fracture |
26 |
31 |
|
|
Without frontal sinus fracture |
11 |
34 |
Table 8
Assessment of frontal sinus fractures as risk factor for CSF leak in patients with PTP.
|
Patients |
With CSF leak |
Without CSF leak |
Chi square=8.02 Degree of freedom=1 Probability=0.005 |
|
With frontal sinus fracture |
12 |
45 |
|
|
Without frontal sinus fracture |
1 |
44 |
Table 9
Assessment of massive PTP as risk factor for CSF leak
|
Patients |
With CSF leak |
Without CSF leak |
Chi square= 15.1 Degree of freedom = 1 Probability = 0.000 |
|
With massive PTP |
11 |
26 |
|
|
Without massive PTP |
2 |
63 |
Hence, these patients are in particular need for specific observation for development of complications like TP, CSF leak, meningitis etc. Pillai et al. stated that fractures of frontal sinus followed by ethmoid sinus fracture are most common in cases of TP. 6
In our patients with PTP, CT imaging also showed associated craniocerebral injuries and 22 patients underwent craniotomy for cranial hematomas like EDH, SDH, Contusion etc. The repeat CT between 6-24 hours after trauma showed increase in PTP in 9.18% but in the subsequent CT showed a decrease or disappearance of the PTP and none went on to develop complications associated with PTP. Hence the presence of PTP alone is not an indication for repeat CT images unless there are other compelling clinical circumstances.
When the volume of PTP is minimal or is not causing any brain displacement or raised ICP, it can be managed conservatively. With medical management including Oxygen administration by mask at 5L/min till clinical and radiological improvement, 76 patients (76/102; 74.5%) improved and were discharged without any untoward sequelae. Administration of 100% Oxygen through a non-breather mask is said to increase absorption rate of post craniotomy pneumocephalus as compared to breathing room air. Oxygen inhalation may help in the reabsorption of nitrogen into the blood stream and a reduction in the volume of the intracranial air.
Administration of hyperbaric Oxygen has been reported to increase in the rate of absorption of PTP. In a study (Pankaj et al) 7 of 13 patients with post-operative pneumocephalus > 30 ml, where the patients were alternately assigned to a treatment group receiving 100% Oxygen for 24 hours and a control group breathing room air for 24 hours; volume of pneumocephalus significantly decreased by 65% in treatment group as compared to 31% in control group (p=0.009). However, hyperbaric Oxygen administration is not readily available in most centers and further it has been reported to cause TP. 8
Meningitis may occur in 20% (8.6-41) of craniobasal fractures and may increase upto 57% in presence of active CSF leak. 9, 10, 11, 12, 13 The role of prophylactic antibiotic therapy is not proven. Eftekhar et al. 14 found that indradural pneumocephalus increases the risk of meningitis and so must be treated like CSF leak. In our study, the antibiotics were only used in the presence of contaminated wounds or when features of aspiration pneumonia were present. Brodie suggested that there is 8-10 fold increased risk of developing meningitis in patients who had persistent CSF leak for 7-10 days. 15 Prompt identification of CSF fistulae and successful surgical treatment are critical for avoiding life threatening complication. 16, 17 Some authors advocate an immediate surgical repair and other believe that surgery should be done only after conservative treatment for one week. 18, 19, 20, 21, 22, 23, 24 Patients with high velocity motor vehicular accidents with skull base fractures and brain contusion and oedema, active CSF leak possess a higher operative complication in first week. Among such patients operative mortality is 25%. 25 In our study 11 patients had early CSF rhinorrhea and none received prophylactic antibiotics and all were managed without surgery. One patient developed meningitis and was treated successfully with combination of antibiotics.
Choi et al., 26 who studied 293 cases of traumatic CSF leak, found that the incidence of meningitis was significantly higher in patients who received prophylactic antibiotic therapy than in those who did not receive it. In contrast, Brodie 15 investigated 324 cases of posttraumatic CSF fistula, and found a lower incidence of meningitis in those who received prophylactic antibiotic therapy than in those who did not receive preventive antibiotics. CSFR and pneumocephalus had occurred even years after the injury and possess risk of meningitis. 11, 26 In our cohort 4 patients developed meningitis during first admission: 3 patients were post craniotomy for cranial hematomas and one patient had active CSF leak. All four patients improved on CSF analysis and culture based administration of antibiotics.
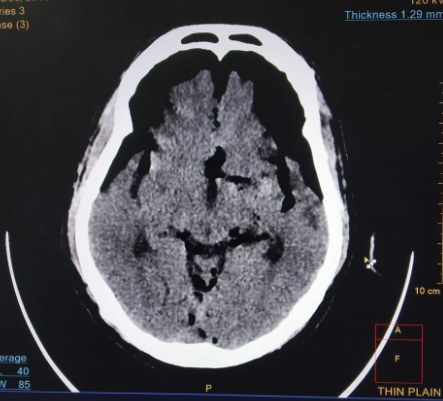
CSF leak remained the major concern in patients with PTP and cranial base fracture. In patients with progressive PTP with features of raised ICP, persistent or increasing CSFR, meningitis and pneumatocoele, investigations are required to plan further surgical obliteration of craniodural defect. Particular attention should be given to sphenoid sinus fractures that may be site of CSF leak and associated optic nerve injury. 27, 28 High resolution thin 1mm slice CT imaging of head and paranasal sinuses with 3D reconstruction, gives better idea about location and type of fracture associated. Further CT/MR cisternography is required to assess the craniodural defect with overlying bony defect for operative planning. Goal of surgical procedure is to close the craniodural defect with pericranium, fascia lata, and temporalis fascia with or without fibrin glue. 29, 30
In our study 11 patients developed early (<72 hours) CSFR and all stopped on medical management. However one patient who had early CSFR developed CSF leak again and two patients developed active CSFR with meningitis and features of raised ICP; several days after trauma. All three patients were operated and improved: 2 underwent bifrontal craniotomy and anterior cranial fossa repair and the third patient had endoscopic repair of a leak from the sphenoid sinus. In our study there was no death due to meningitis, TP or surgery for TP.
The first surgical repair of traumatic CSFR was done by Dandy in 1926 through frontal craniotomy. 31 This approach remained the mainstay of treatments for decades till 1980 when Dohlman, Calcterra and others reported extracranial nasal endoscopic repair of craniodural defect. 32 However Locatelli et al. advocated the key for endoscopic transnasal surgical repair of leak is accurate preoperative localization of fistula, adequate operative field and clear demarcation of size and anatomical location of the defect. 33 So endoscopic approaches are limited for specific indications. Presence of intracranial hematomas, comminuted fractures of the cranial base, fractures of the posterior wall of the frontal sinus and lateral extensions of frontal sinus fractures are contraindications for endoscopic approach and bifrontal craniotomy and transcranial repair of dural defect is appropriate procedure of choice. 34, 35 Bi-frontal craniotomy and cranialisation of frontal sinus, packing of frontonasal duct and repair of dural defect with graft and fibrin glue is the optimal surgical intervention. Open surgery has several advantages like access to both intradural and extradural space in anterior cranial fossa, repair of dural defect and evacuation of underlying craniocerebral hematomas. Another advantage of the intracranial approach is the possibility of treating cranial and facial fractures and deformations in a single procedure via a combined approach with maxillofacial surgeon. 36 None of our patients showed recurrence of CSF leak after surgical intervention and repair of craniodural defect.
In keeping with the fact that PTP occurs in patients with frontal fractures or skull base fractures, many patients had cranial nerve injuries involving the olfactory (4/92), optic (9/92), facial (9/92) and vestibuo-cochlear (7/92) nerves. Injury to cranial nerves can occur early due to basal skull fractures, shearing forces or rapid acceleration-decelerations injuries. Sometimes the manifestation may be late if it occurs due to ischemia, edema or hematomas. 37 Optic nerve injuries were seen in 9.8% of our patients. It appears to be more common in the subgroup of patients with PTP as its reported incidence is 2.78%. 38 As patients with PTP are more likely to have frontal bone fractures often involving the anterior skull base, the same injury may also cause optic nerve injury. As a corollary, patients with PTP should have thorough cranial nerve examination once they are stable.
Early post-traumatic seizures (PTS) were seen in 3 patients (3/102) in our study. However all patients were on prophylactic anticonvulsants due to risks for seizures due to the associated injuries. In a prospective study of 520 patients with TBI, the incidence of PTC was: 2.1% -Early PTS; 6.5%- Immediate PTS and 2.7% Late PTS. Pneumocephalus was not found to be a significant risk factor for PTS in that study. 39
There are some drawbacks in our study. The period of follow-up is only few months after trauma. It is known that CSFR and meningitis can occur many years after injury. There were no cases of CSF otorrhea during the study period. However, otorrhea is less common and is known to subside spontaneously generally.