Introduction
Agenesis of the corpus callosum (ACC) is one of the most frequent congenital brain disorders, characterized by the total or partial loss of the corpus callosum. Callosal development disorders can arise when neurogenesis, neuronal migration and specification, telencephalic midline patterning, axon guidance, or post-guidance development are disrupted.1 This abnormality can develop singly, in conjunction with chromosomal, syndromic, or monogenic problems, and, in rare cases, as a result of ischemic, viral, or teratogenic causes;2 only 10% of the cases are related to chromosomal abnormalities.3 Different studies illustrated that the prevalence of ACC is about 1 in 4000-5000 live-births.4 The studies describe a range of cognitive and neurological characteristics related with ACC; developmental delay, linguistic difficulty, intellectual disability, motor impairments, and epilepsy are all common traits.5
ACC is detected during a second-trimester ultrasonography test when the cavum septi pellucidi (CSP) is not visible in the axial plane; However, due to the heterogeneity of presentation, prenatal diagnosis may not be attainable in all cases.2, 6 In addition, the prognosis of patients diagnosed with ACC is difficult to predict.7
There are several known syndromes, such as Aicardi, acrocallosal, Andermann, and Shapiro, in which the ACC can occur alongside other disorders.8 Acrocallosal syndrome (ACLS) is an uncommon autosomal recessive genetic disorder initially discovered in 1979 by Schinzel et al.; which is caused by mutations in the KIF7 gene.9 ACLS is characterized by corpus callosum agenesis, hallux duplication, post-axial and pre-axial polydactyly, macrocephaly, minor craniofacial anomalies, and severe psychomotor retardation. 9 Although autosomal recessive inheritance has been hypothesized, ACLS frequently seems to develop sporadicly.10 However, Genetic counseling is an essential precaution for future pregnancies.11
We present the case of a 20-day-old neonate with characteristics consistent with ACLS. The patient’s parents did not have a hereditary disorder. This case report was carried out in compliance with the World Medical Association's Helsinki Declaration. The patient’s parents have given us written informed consent for this case report to be published.
Case Presentation
The patient was a 20-day-old boy who was brought to the Pediatric Neurology Clinic due to the discovery of corpus callosum agenesis during the 32th week of the mother's pregnancy. He was first in birth order and was delivered by cesarean section at 38 weeks.The patient’s parents mentioned no history of similar disorders in their family. No consanguinity existed between the parents. They had previously undergone a genetic test that revealed no abnormalities. The patient’s mother was 29 years old and was a hairdresser. The mother possessed no prior abortions. She had no history of illness, smoking, or use of alcohol or drugs during or before the pregnancy. Only in the 28th week of pregnancy did the mother experience a sore throat, and polymerase chain reaction revealed the presence of SARS-COV-2. She had received two doses of Sinopharm vaccine at 15 and 21 weeks of gestation. Early prenatal tests revealed no abnormalities. The 12th gestational week screening ultrasonography revealed NT<3cm and CRL=60.7cm, both of which were normal. In the 17th week ultrasonograghy, the risk of placenta previa was noted since the placenta was located in the anterior wall of the uterus. At 5 months of gestation, echocardiography was also conducted for the fetus, which showed the presence of atrial septal defect (ASD) and mild tricuspid regurcitation (TR). In the 32nd week of pregnancy, an ultrasonography revealed evidence of hydrocephalus in the occipital ventricles with AP trigone maximal diameter of 16 mm. Anomalies of the corpus callosum were suggested based on the teardrop sign in the frontal horn view. The dilated ventricles resembled colpocephaly, and the third cerebral ventricle was slightly displaced. Based on the results of the sonography, it was decided to refer to the pediatric neurology clinic for additional evaluations following the child's delivery. The apgar score of the newborn was 9 out of 10. His birth weight was 2780 gr, birth height was 47 cm, and birth head circumference was 34 cm.
On arrival at the clinic, the child was in a good general condition. He had stable vital signs. His height and head circumference were normal and within the Z-score range of 0 to +1, and his weight was 3450 gr within the Z-score range of -2 to -1. Examination of the skull indicated anterior fontanelle enlargement. On the patient's face there were no apparent abnormalities. A short systolic ejection murmur was detected in the left fourth parasternal space during a cardiovascular examination. His muscle tone and infantile reflexes were normal. The right foot pre-axial polydactyly was observed during the limb assessment (Figure 1). The examination of the abdomen and genitourinary system was normal.
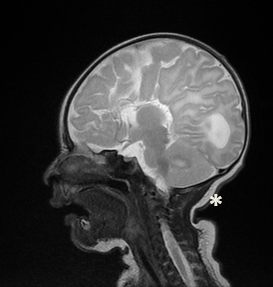
Brain MRI and electroencephalogram were performed for the patient. The electroencephalogram results were unremarkable. On the MRI of the brain, agenesis of the corpus callosum was noted in association with colpocephaly and significant enlargement of the lateral ventricles (Figure 2, Figure 3). Based on the foregoing, the pediatric neurologist decided to follow up the child's neurological development.
Figure 2
Coronal T1-weighted brain MRI showing enlargement of the occipital lateral ventricles (white stars)

Figure 3
Sagittal T2-weighted brain MRI showing agenesis of the corpus calosum (black arrow) and enlargement of lateral ventricle (white star)
Agenesis of the corpus callosum is one of the most frequently found structural brain abnormalities with several recognized syndromic correlations and genetic disorders, with an incidence between 0.03 to 0.7%.12 Polydactyly and agenesis of the corpus callosum are characteristics of acrocallosal syndrome (ACLS). Despite the high incidence of hand and foot polydactyly, preaxial polydactyly of the foot is expected to occur in only 0.4 cases per 10,000 Europeans.13 Preaxial polydactyly of the foot is related with other congenital anomalies and syndromes, such as craniosynostosis, renal malformations, and also corpus callosum agenesis in ACLS as seen in our patient. ACLS is an extremely rare developmental condition and only roughly forty cases have been reported globally to date.14
According to the criteria established by Courtens et al in 1997, the diagnosis of ACLS can be made if at least three of the following four criteria are present: 1) Minor craniofacial abnormalities 2) Moderate to severe mental retardation with hypotonia 3) Polydactyly 4) Total or partial absence of the corpus callosum.11 Polydactyly and agenesis of the corpus callosum and widening of the anterior fontanelle were observable in our patient, but despite the structural abnormalities of the brain, the patient's neurological exams were normal. Due to the child's young age, it is currently impossible to form a definitive assessment on his mental development.
The cardiac results are comparable to prior reports of congenital heart diseases found in two other cases. In the report by Casamassima et al., the child diagnosed with ACLS displayed tetralogy of Fallot on echocardiogram and Wolff-Parkinson-White Type B on electrocardiogram.15 In Singhal et al. report, the echocardiography of the patient with ACLS indicated a small secundum type ASD with moderate tricuspid regurgitation and dextro positioning of the heart.10 Considering that ASD was detected by echocardiography in the present study, it is possible that cardiac abnormalities are among the symptoms of this syndrome.
Acrocallosal syndrome, Joubert syndrome, and hydrolethalus fetal syndrome are all caused by a missense mutation in KIF7(15q26.1), a modulator of ciliary Hedgehog signaling. 16 Due to the autosomal recessive inheritance pattern of ACLS, the recurrence risk is 25%, making genetic counseling essential. In our case, the genetic test had revealed that the patient's parents were healthy. According to the studies, although autosomal recessive inheritance has been proposed, ACLS often tends to happen sporadically.17 It was also noteworthy that the patient's mother worked as a hairdresser and had been exposed to chemicals during pregnancy. In a study by Rylander et al., it was determined that a greater proportion of children born to hairdressers suffered major malformations (2.8% vs 2.1%). 18 However, in previous studies, mostly oral clefts have been linked to mother's occupation as a hairdresser. 19 On the other hand, laboratory research on mice have demonstrated that exposure to cosmetics-related chemicals including toluene, significantly raises an index of poor perinatal outcome, comprising morphological and marginal neurodevelopmental malformations and newborn mortality. 20 These studies imply that the mother's exposure to cosmetic-related substances may be a possible cause of the neonate's abnormalities.
Conclusion
The current case provides additional evidence that ACLS can be linked with pre-axial polydactyly and craniofacial symptoms such as widening of the anterior fontanelle in addition to corpus callosum agenesis. Ultrasonography during the second trimester can reveal abnormalities of the central nervous system, including ventricular enlargement and corpus callosum defects. It is recommended that echocardiography also be performed on these children in order to screen for any heart abnormalities. In addition, due to the increased likelihood of congenital abnormalities in children born to hairdresser mothers, it is essential to minimize exposure to cosmetic chemicals during pregnancy or to take the required precautions.
Authors’ Contributions
RS was the principal investigator of the study. RS and AG were included in preparing the concept and design. MV and HB revisited the manuscript and critically evaluated the intellectual contents. All authors participated in preparing the final draft of the manuscript, revised the manuscript, and critically evaluated the intellectual contents. All authors have read and approved the manuscript's content and confirmed the accuracy or integrity of any part of the work.

