Introduction
Sturge-Weber syndrome (SWS), also known as encephalofacial angiomatosis or cephalotrigeminal angiomatosis, is a form of neuro-cutaneous disorder. It is seen in 1 in 50,000 people. It does not exhibit a racial bias and equally affects both sexes. 1, 2, 3
SWS typically shows up as a facial Port Wine Stain (PWS), although there are specific instances of SWS where PWS is evident in the trunk or extremities or when there is no visible PWS. PWS is present since birth. Due to the lesions' initial flat pink look, PWS might be mistaken for a bruise.4 The lesion darkens with age from reddish to purple colour.5 SWS can cause brain epilepsy, neurological impairment and eye glaucoma.4 Port-wine stains on the face are typically isolated observations, but when they coexist with vascular abnormalities of the brain and eyes, they constitute the classic triad of Sturge-Weber syndrome (SWS). 6
The prevalence of PWS is estimated at three to five children per 1000 live births; there are ~26 million people worldwide with PWS birthmarks.7, 8, 9 The majority of facial PWS (~90%) are unilateral in a trigeminal dermatomal distribution.10 The management options for SWS are limited. The primary goal is to minimize the seizure activity with anticonvulsant medications11 but when medical management fails, surgical treatment is considered.4, 11 Eye glaucoma is treated to reduce the intraocular fluid pressure. 4, 11
Case History
Here, we report a case of 39 years old female with SWS who presented with classical triad of SWS i.e., bilateral port-wine stain, epilepsy and severe glaucoma.
Port Wine Stain (PWS) was present on both sides of the face. (Figure 1) The lesion was present since birth and gradual enlargement was noticed. The bluish red lesion was not seen in other parts of the body. Family history did not reveal any similar complaint from her immediate or distant relatives. The patient had a history of right focal seizures 30 years ago which were predominantly motor in origin. The last episode took place 10 years ago. The patient also presented with right upper limb parasthesias associated with tingling which are episodic, usually lasting for a few minutes. They might possibly be a sensory seizure or secondary to ischemia. Intraoral examination did not show any gingival bleeding or overgrowth. Patient also has history of glaucoma in both eyes since 20 years with significant vision loss.
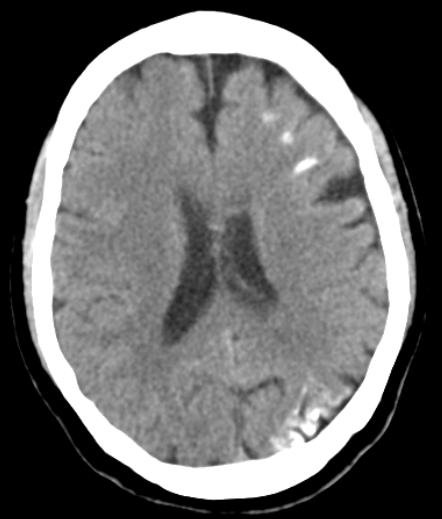
An electroencephalogram (EEG) was done which was suggestive of asymmetrical background with lower amplitude on left side without any interictal epileptiform discharges. CT Brain (P) was done which revealed gyral calcification and atrophy in left fronto parietal lobes. (Figure 2) Treatment was given with anticonvulsants.
In a nutshell, flat pinkish-purple facial birthmark (portwine stain), right focal seizures, radiographic findings of white matter calcifications and glaucoma were suggestive of Sturge–Weber syndrome type I.
Discussion
Sturge-Weber syndrome (SWS) is a rare neuro-cutaneous disorder characterized by the association of a facial birthmark called a port-wine birthmark, abnormal blood vessels in the brain, and eye abnormalities such as glaucoma. It can be viewed as a spectrum of diseases in which patients may experience abnormalities in all three of these systems (the brain, skin, and eyes), simply two of them, or just one. The illness is not inherited and does not run in families, despite the fact that symptoms are typically evident at birth (congenital).12 The disease gets its name from the William Allen Sturge and Frederick Parkes Weber. Sturge described the cutaneous, ocular and neural features of the disease in 1869 and Weber documented the radiological changes observed in these patients in 1929. 1, 2
Some publications break down SWS into three main subtypes. Type 1 consists of skin and neurological symptoms with or without glaucoma. Type 2 consists of skin symptoms and possibly glaucoma, but there is no evidence of neurological involvement. Type 3 consists of neurological involvement, but without skin abnormalities and glaucoma.12 Our patient represents Type 1 SWS.
A congenital facial birthmark known as port-wine stain or nevus flammeus is often the most notable initial symptom. This birthmark can range from light pink to reddish to dark purple in color and its size can vary. Usually, at least one eyelid, temple area, and/or the forehead of one side of the face are affected; both sides of the face have been affected less often. 12 The majority of facial PWS (~90%) are unilateral in a trigeminal dermatomal distribution.10 But our patient presented with PWS on both sides of the face i.e., bilateral PWS which is quite uncommon. (Figure 1) Bishnu Deep Pathak et al. reported a case of a young girl, who also had port-wine stain bilaterally i.e., both right and left parts of the forehead were affected. In a case report by Mukhopadhyay.S, additional port wine lesions were found elsewhere in the patient’s body i.e., hands, chest, abdomen, back, ear, leg, and even skin of the head were also involved.13 According to a case report by Kundan Mittal et al. bilateral dark-pigmented port wine stain over face, trunk, back, and arms.14, 15 Our patient did not involve PWS on any other parts of the body except her face.
Individuals with SWS may also experience a variety of neurological abnormalities. A head computed tomography (CT) scan can show intracranial calcification in certain areas of the brain. CT Brain (P) of the patient revealed mild to moderate atrophy of left fronto-parieto-occipital lobes with areas of gyral calcification in fronto-parietal lobes which can be seen Figure 2. The extent of neurological involvement can vary dramatically from one person to another. Seizures, which often begin in infancy or childhood, are a common finding. The reported patient has history of right focal seizures since 30 years which was well controlled with anticonvulsants. She did not have any fresh episodes of seizures since the last 10 years. There is no history of secondary generalized tonic clonic seizures. Seizures usually affect the opposite side of the body as the brain involvement (and the port-wine birthmark), but sometimes affect both sides of the body.12 Our patient had right focal seizures which is opposite to the brain involvement (Figure 2). Affected individuals may also experience muscle weakness or paralysis on one side of the body (hemiparesis), usually on the side opposite the brain involvement and the port-wine birthmark. But the patient did not present with any such weakness.
Some patients are born with, or develop, glaucoma which usually affects the eye on the same side of the face as the port-wine birthmark.12 Our patient presented with history of glaucoma on both eyes since 20 years. Headaches, including migraines, and visual field defects such as the loss of vision in half the visual field in one or both eyes (hemaniopsia) may also occur.12 The patient experienced frequent unilateral migrainous headaches (10 times/ month) which persisted for 1-2 days. Intraoral involvement is common, resulting in hypervascular changes to the ipsilateral mucosa which causes gingival overgrowth, gingival bleeding and asymmetric jaw growth. But our patient's intraoral examination was completely normal. There was no evidence of any bleeding gums.
The location and extent of the lesion determine the port wine stain's course of treatment. The options include surgical resection, sclerotherapy, laser photocoagulation, and a combination of these. Some lesions might not be treatable; thus, treatment should focus on symptom management. Particularly if magnetic resonance imaging (MRI) reveals that the lesion has a distinct border and is accessible, surgery should be taken into consideration.