Case Report
A 32-year old man presented to emergency with complaints of intermittent headache for 6 days and following an episode of generalised tonic clonic seizures an hour prior to admission and with post ictal state.
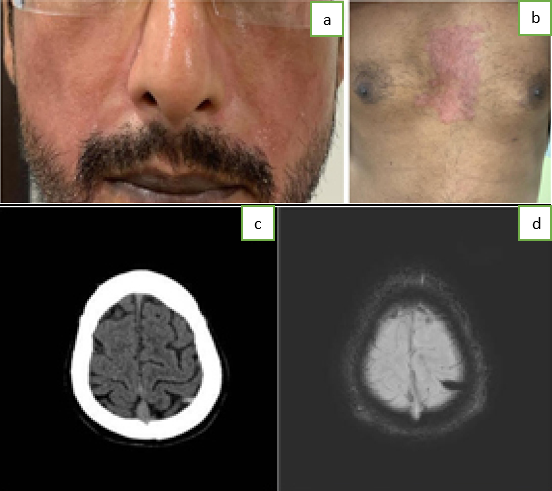
On examination, he had a blood pressure of 110/70, regular pulse of 70/min but was in an altered mental state. Pupils werebilaterally equal and reactive to light and margins of fundus were clear. Malar rash on the face (Figure 1A), erythematous rash on chest (Figure 1B) and thickening of skin on palms were noted.
He was started on intravenousantiepileptics and intubated for airway protection. CT, MRI with MRV Brain revealed ICVT (Figure 1C,D). Coagulation screen, procoagulant work up, autoimmune profile, serum ACE levels, cerebrospinal fluid (CSF) analysis along with the routine blood investigations. CSF was non-contributory. ACE and Coagulation profile was within normal limits. Procoagulants like antithrombin III, protein C, S were normal and Anticardiolipin antibodies, lupus anticoagulant titres were not raised. Anti-Centromere antibodies were positive. He was commenced on anticoagulants and hydroxychloroquine.
Follow up after three months, revealed an asymptomatic patient. He was on hydroxychloroquine, anti-epileptics and lifelong anticoagulants.
Discussion
Isolated cortical vein thrombosis (ICVT) without concomitant cerebral venous sinus thrombosis (CVST) is an infrequent and serious variant of cerebral venous thrombosis(CVT). 1, 2, 3 It is the thrombosis of 1 or more cerebral cortical veins without affection of Dural sinuses or deep cerebral veins.1, 2 Considerable aetiology is unknown (20-35%),1 with connective tissue disease often being the underlying cause.1 Systemic Sclerosis (SSc) revealed on our aetiological workup is uncommon.4
SSc has an annual incidence of 10 per million with a female preponderance.4 Inflammatory, vascular and fibrotic changes leading to excessive collagen deposition are prevalent. Hallmarks include fibrosis of skin (scleroderma) and/or internal organs, production of auto-antibodies and vasculopathy. Anti-Scl-70 and anti-RNP antibodies increase risk of neurological complications which are relatively uncommon.4 CNS manifestations are even rare and supposedly due to cerebral vasculopathy. Arterial involvement including arteritis, aneurysm, ischaemia, haemorrhage predominates. Venous involvement seldom occurs.4
CVT comprises three main syndromes - isolated intracranial hypertension, focal, and encephalopathy. Seizures manifest in focal syndrome. ICVT may potentiate permanent parenchymal damage, resulting in cerebral infarction. Predominant in young (<40 years) females, a wide clinical spectrum exists. Headaches and seizures are the commonest, followed by focal neurological deficit and altered mental status. Unlike CVST, papilledema does not prevail. 50% cases may be subacute (2d - 1mo of onset), having inflammatory aetiology.1, 2, 3
Non-contrast CT Brain is the first investigation to rule out CVT mimickers and demonstrate the “cord sign” - a linear hyperdensity arising due to changes in blood density within thrombosis vein. MRI and MRV are recommended once suspicion is raised. Susceptibility Weighted Imaging is more sensitive than Gradient Echo in detecting blood and its breakdown products. It is evolving into a gold standard diagnostic modality despite background of high anatomic variability of small occluded veins.
Heparin anticoagulation is the cornerstone of management.1, 3 It prevents thrombus propagation and allows recanalization, reducing risk of focal neurological deficit. LMWH has lower risk of inter cerebral haemorrhage, heparin induced thrombocytopenia and longer half-life as compared to UFH. Switchover to warfarin targetting INR 2-3 is considered after neurological improvement. Simultaneously, anticonvulsants for seizures and treatment of underlying cause as in our case is warranted.1
Cerebral veins are valve less and lack muscular coat, hence vulnerable. Virchow’s triad of hypercoagulability, endothelial injury and stasis must operate for thrombosis. In SSc, inflammation upsets the coagulation pathways resulting in a prothrombotic state. Inflammatory mediators create an oxidative stress, which superimposed with vascular changes result in endothelial injury.2, 3, 5 This injury invites initial vasoconstriction and platelet aggregation. Endothelial injury, platelet aggregation with fibrotic changes of the cerebral veins may be a possible mechanism of vascular stasis. The triad being complete, we hypothesise how ICVT can occur in SSc. However, further evidence may be necessary.