Introduction
As per the International Association for the Study of Pain (IASP), headache, is the most common, painful, and disabling conditions that affects people throughout their lives.1 Headache disorders are a worldwide problem, although there are regional variations. It affects people of all ages, geographical areas, races and socioeconomic status and is more common in women. It can be extremely debilitating at times and can have a significant impact on an individual’s quality of life, imposing huge costs to healthcare and indirectly to the economy in general.2, 3, 4
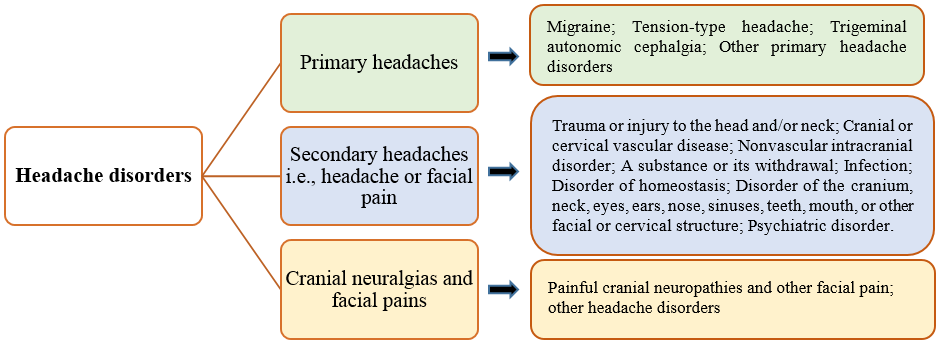
As per the International Classification of Headache Disorders (ICHD), headache is classified as primary headache that has no known underlying cause; secondary headache that is due to another condition causing traction due to inflammation of pain-sensitive structures; and the painful cranial neuropathies and other facial pains (Figure 1).4, 5 Given the associated disability and financial costs to the society, headache disorders are of public-health concern especially migraine, tension-type headache and medication-overuse headache as they are responsible for high levels of disability and ill-health.6 More than 90% of the patients presenting with headache in primary care have a primary headache disorder. 4
The most important types of headaches are:7
Acute headache i.e., subarachnoid haemorrhage, and others that presents with acute onset, severe headache with / or without neurological symptoms.
Episodic headache i.e., migraine with /or without aura that presents with pulsating headache, aggravation by physical activity with nausea, phono- and photophobia; tension-type headache that presents with pressure headache without associated symptoms; cluster headache and others that presents with unilateral headache with ipsilateral autonomic facial symptoms; trigeminal neuralgia that presents with unilateral severe headache lasting for seconds.
Chronic headache i.e., chronic tension-type headache that presents with pressure headache without associated symptoms or medication overuse headache; medication-overuse headache that is associated with use of acute pain medication more than 10–15 days per month; intracranial hypertension, inclusive of brain tumour headache that presents with frequent and increasing headache with nausea and neurological symptom.
Headache responsible for high population levels of disability and ill-health are migraine, tension-type headache and medication-overuse headache. Migraine often begins at puberty and affects those aged between 35 - 45 years, is more common in women, is recurrent, often life-long, and characterized by recurring attacks. Tension-type headache (TTH) that may be stress-related or associated with musculoskeletal problems in the neck can be episodic (<15 days/month) in more than 70% of the people and chronic (>15 days/ month) in about 1-3% of the people. Cluster headache (CH) is relatively uncommon (<1 in 1000 adults) can be episodic and chronic mostly in people ≥20 years.6
One of the very common cause of headache is also gastro-intestinal (GI) disturbances. The main causative factor of headache in GI diseases is due to disturbance of function with or without organic disease. It can be due to organic causes or functional GI diseases, IBD and CD along with H.pylori infection. 8, 9
Table 1
Triggers for different types of common headache
|
Migraine 10 |
Tension-Type Headache 11 |
Cluster Headache 12 |
|
Stress; hormonal changes during menstruation, ovulation, and pregnancy; skipped meals; weather changes; excessive or insufficient sleep; different odors like perfumes, colognes, petroleum distillates; neck pain; exposure to lights; ingestion of alcohol; smoking; late sleeping; heat; food (aspartame, tyramine and chocolate); exercise and sexual activity. |
Stress (mental or physical); irregular or inappropriate meals; high intake of coffee/ caffeine-containing drinks; dehydration; sleep disorders, too much or too little sleep; reduced or inappropriate physical activity; psychological problems; menstrual cycle and hormonal substitution in females. |
Watching television; alcohol; hot weather; stress; use of nitro-glycerine; sexual activity; and glare. |
Headache disorders are a problem worldwide and affects people of all geographical areas, ages, races, income levels. 6 About 70% of the people (7 in 10) have at least 1 headache a year. 13 and about 50% of the adults have had a headache at least once within the previous year (i.e., symptomatic at least once within the previous year). About 50-75% of those aged 18–65 years worldwide have had headache in the previous year and, ≥ 30% of those have migraine headaches. About 1.7–4% of the world’s adult population have headache on ≥15 days every month. 6
Discussion
Burden of headache
As per the Global Burden of Disease (GBD) study, headache disorders are one of the major public-health concerns globally in all countries and world regions.14 Headache disorders are among the most prevalent and disabling conditions worldwide. Globally, the current headache disorder of any type (i.e., active) was reported in about 52% of the population, 44.4% and 57.8% in males and females respectively. Migraine was reported in about 14.0% of the population, 8.6% and 17.0% in males and females respectively and tension-type headache (TTH) in 26.0% of the population, 23.4% and 27.1% in males and females respectively. Headache on ≥15 days/month was reported in 4.6% of the population, 2.9% and 6.0% in males and females respectively. 14
As per the 2017 global pain index report, about 86% of people claim to have experienced head pain (TTH or migraine) at some point in their life, with about 23% of them experiencing head pain on a weekly basis. In India it is about 31 - 40%. About 22% claimed to experience tension-type headaches weekly, which was more common among women (26% vs. 18% in men). 15 As per 2020 global pain index report, of the ten different pains experienced by an individual in a year, 84% is due to headache, which was more common among Gen Z and millennials compared to other generations (90% vs. 79%). 15
The lifelong prevalence of headache is 96%, with a female predominance. The prevalence of chronic daily headache worldwide has been consistent between 3-5% which most likely represents chronic migraine. 4
Headache is common in childhood, especially primary headache (TTH or migraine) that tends to increase in frequency during adolescence. 16 A review of 50 population-based studies reported the overall prevalence of a headache and migraine in children and adolescents (< 20years) at any point in time to be 58.4% (95% CI 58.1–58.8%) and 7.7% (95% CI 7.6–7.8) respectively. 17, 18
Primary headache disorders are among the commonest disorders that affects people in almost all countries and India is no exception. A large population-based neuro epidemiological survey from Karnataka involving different villages reported that people suffering from headache are found to be more in rural areas than in the urban areas. Prevalence in rural areas was 71.2% (68.4 - 73.8%) which was much higher than that of 57.3% (54.5-60.1%) in urban areas after adjusting for gender. Although it is not clear as to what makes the rural population more prone to headache, the probable factors could be exposure to sunlight, physical labour, financial stress, stress of family life and lack of easily accessible care and resources. 19
The 1-year crude prevalence of any headache was 63.9%, with a female: male preponderance of 4:3 in a door-to-door survey in and around areas of Bangalore. The study included 2,329 adults (urban = 1,226 and rural = 1,103) aged 18–65 years who were interviewed using a pilot-tested, validated, structured questionnaire. The age-standardised 1 year prevalence of migraine was 25.2% that was very high compared to the mean global prevalence (14.7%) and TTH was 35.1% which was higher among younger age group. Estimated prevalence of all headache on ≥15 days/month was 3.0% and probable medication overuse headache was 1.2% that was more among female and rural population. 20
In another study from Urban Kolkata, community-based 1-year prevalence of migraine in India was 14.12% which was found to be similar to that observed in other countries and the maximum burden was among females. 21
In another epidemiological study in the national capital region of Delhi which included rural and urban areas, the 1-yr prevalence of migraine was estimated to be 27.2%. Overall data showed primary headaches in India to be more than or as prevalent as in the Western countries. The correct estimation of the disease burden will need better epidemiological data. When the current estimates were applied to the population of India, the absolute number of people with migraine, tension type headache, and chronic daily headache in Indian adults was about 211.25 million; 295.75 million and 25.35 million respectively (based on the assumption of population of India to be 1300 million with 845 million of adult population). 2
Both migraine and TTH cause significant burden on individuals as well as the society with substantial rates of absenteeism and lost productivity at work, home, and school. 22 A prospective observational study (Jan 2020 – Sep 2021) of 815 patients presenting with main complaints of headache, migraine was found to be the most common primary headache followed by TTH. About 67.7% of the patients had migraine and 32.2% had TTH. The common triggers were loss of sleep, prolonged working hours, and stress. 23
Usually headache disorders are not perceived to be serious because they are generally episodic, do not cause death, and are not contagious. Headaches are not just painful, but can also be disabling. Repeated headaches and the constant fear of getting it again can affect family life, social life and employment. Also the long-term effort of coping with a chronic headache can predispose to other illnesses. 6 The myths and behavioural preferences (headache is caused by social or emotional problems, visual impairment, exposure to very bright light, or supernatural forces etc. the trust in traditional healers and distrust in modern medicine) not just results in delayed, missed/ or mistaken diagnoses, but also results in individuals failing to receive medically proven treatments. 24 About 95% of headaches seen in practice are primary headaches, yet they are not considered a serious problem warranting attention because they are not life-threatening, and do not cause permanent disability. They are often neglected with no specific diagnosis and treatment and is managed sub optimally many a times. 25 Hence appropriate treatment of headache disorders will require accurate diagnosis and recognition of the conditions, simple lifestyle modifications, patient education and appropriate treatment with cost-effective medications. 6
Stress and Hheadache
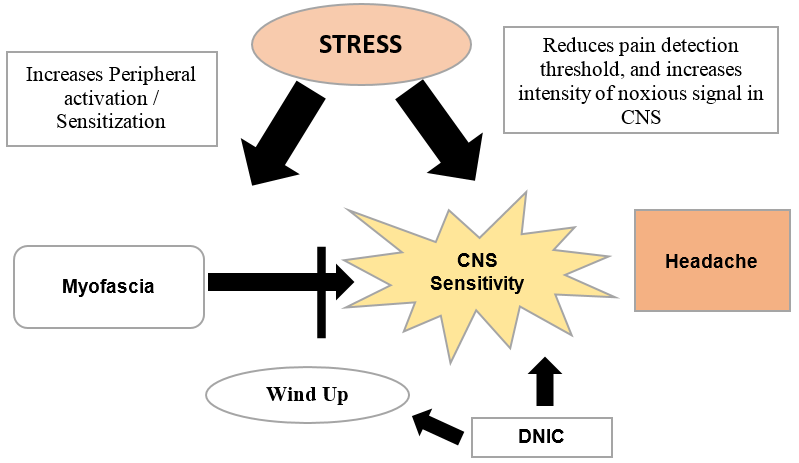
For centuries, the relationship between stress and headache has been well known (Figure 2). Often, patients with headache report stress to be one of their main activators or aggravators for their headache. 26
Figure 2
Stress and headache mechanisms 27
CNS: Central Nervous System; DNIC: Diffuse Noxious Inhibitory Control.
A stress and headache survey that included 11,203 individuals aged 22-45 years in 35 cities across 16 states (conducted in 2021 in India during the COVID-19 pandemic) reported stress to be a common phenomenon across all geographies with more than 75% of the respondents have felt stress in the previous one year. About 89% of respondents had a headache in the same time period, which was more common among women vs. men (92% vs. 86%), esp. women working full time (93% vs. 87%). Increased stress levels were found to be associated with increased headaches in about 89% of the respondents. About 42% of the respondents reported bouts of headache once a week or more frequently. Headaches were found to be the most prominent symptom of stress in about 41% of the respondents (those who felt stressed /had a headache), more so among women vs. men (45% vs. 37%); working women vs. working men (46% vs. 40%) and women working full time vs. men working full time to stress (45% vs. 37%). More than half of the sufferers claimed to have resorted to some medication when they have a headache while an alarming 38% working respondents take leave from work when they have a headache. Most respondents (48%) act on their headache within few hours, indicating the need for highly effective medication. 28
Stress is presumed to be an etiological factor in the first onset of a primary headache disorder. 26 TTH and migraine, the most common primary headache disorders affect about 80% of the general population and stress is one of the most common trigger factors for both migraine and tension-type headache. 29, 30
Stress leads to a worsening of chronic headaches. It also acts as a trigger of episodic headache attacks before they transform into chronic headaches. Those with headache may either be more exposed to stressful psychosocial stimuli, or have reduced ability to tolerate stress. Those with transformed headache may not have greater exposure to major stressful events, but they have a different way of reacting to stress. 30
There are many factors that may influence the relationship between stress and primary headache disorders. It could be age, gender, socioeconomic status, subtype, severity and frequency of headache, comorbidities (medical and psychiatric), coping style, catastrophizing,
resilience, grit, psychological and physiological reactivity to stress and also biological indices like sleep, nutrition etc. Various stress-related emotional and cognitive states could be due to anger that is suppressed, mental anxiety, repression and conversion, or resentment and dissatisfaction. 26
Stress could be a predisposing factor that could: 26, 29
Contribute to onset of headache disorders
Accelerate the progression to chronic headache
Provoke or exacerbate headache episodes.
A trigger that could increase the probability of an attack of headache or migraine
A premonitory symptom of an attack.
Most epidemiological studies report females to be more affected with primary headache disorders. This could be to hormonal factors and it could also be secondary to stress, as females have multiple roles to perform in Indian households. People who are married report more headaches than unmarried people which again suggests that stress of married life could be a precipitating factor for primary headache disorders.31
Headache itself could be a stressor and hence stress-management approaches in patients with different headache subtypes becomes important.29
Headache and its impact on quality of Life (QoL)
Headache that is chronic or recurring can have an effect on the well-being of an individual. Most patients experience a reduction in their functional capacities during headache attack and can have diminished motor performance and disturbed interpersonal relationships with a feeling of inadequacy.32
Headache is not just about pain, it could also be disabling in many individuals.1 Migraine, medication overuse headache and tension type headache are the 2nd, 6th and 12th leading causes of disability from neurological disorders globally.33
Migraine is associated substantial disability among females, those living in rural areas and individuals aged <40 years due to higher disease burden.34
About 8 out 10 individuals with pain are anxious or worried about the pain with impact on mood, especially those with headache. At least 1 in 3 workers take time off due to headache annually. About 56% (66% in India) of those with headache feel that work to be the cause their headache. About 42% say they regularly work through their headache and 12% say they regularly leave work early because of headache. 15
Headache disorders are most troublesome in the productive years of life i.e., late teens to 50s and the estimates of their financial cost to society are huge which is mainly from lost working hours and reduced productivity. 6 Lost productive time, including lost paid work time, is one of the major burdens that has huge implications not only for those affected but also for their dependents and society. The working population (18–65 years) lost 2.7% of its entire productive time to headache which is > 6 days a year which is an enormous loss and those with migraine lost 5.8 % of their productive time i.e, about 4 days a year. The lost paid work time accounts for 40 % of this which may have an impact on GDP. 35
As per the recent GBD analysis (2019), headache disorders were estimated to be responsible for 46.6 million years lived with disability (YLDs) globally (5.4% of all YLDs). The age standardized rate was 602.5 YLDs/100,000 person-years Headache disorders were ranked as the 3rd cause of disability (after back pain and depressive disorders), and the 1st cause in adults <50 years. 36
The burden of headache disorders has not been systematically studied. It is not considered to be of much public health significance given its ubiquitous nature with little or no resultant mortality or permanent disability. But headache disorders do impose a considerable burden on sufferers that could have substantial personal impact, impaired quality of life and incur cost. Repeated headaches, and the constant fear of the next one can affect family and social life and employment. Also the long-term effort of coping with a chronic headache disorder can predispose an individual to other illnesses (like anxiety and depression are more common in those with migraine). 2
Migraine is the 2nd most prevalent primary headache disorder and a major cause of disability among patients with primary headache disorder causing significant functional impairment, physical as well as psychological. 37 It is the leading cause of disability in adults <50 years of age and the 2nd leading cause of disability at all other ages worldwide. About 25% of the people with migraine have moderate to severe disability that is about 32.3% in North America, 12% in Europe, 22% in South America and 19% in Asia.38 Migraine caused 45·1 million and tension-type headache 7·2 million YLDs globally in 2016. GBD estimates from India show that migraine has jumped nine places from being ranked 24 to 15 in the disease burden for India between 1990 -2016. 2
A number of studies across multiple countries have investigated the impact of migraine on work performance. About 86 million workdays are lost to migraine each year and migraine costs 8.8 billion per year in lost productivity in the UK and about £1 billion is spent on healthcare costs associated with migraine. Whereas in the U.S, the annual migraine-related costs for every 1000 employees are estimated to be US$ 84,000, of which 33% is attributable to lost work time. In Singapore, migraine cost about $1.04 billion Singapore dollars in economic losses in 2018 that was largely attributed to lost productivity. 39
Self-Care in Managing Headache
One of the commonest conditions people take medications without professional help is headache. If the frequency of headache is low and the symptoms are not disabling, professional help may not be needed. Such headaches can be easily managed with simple analgesia. Self-care is what is needed for most people, when the symptoms have an established and familiar pattern. When the symptoms are unmanageable with these measures professional help is needed. It is also important to educate people to recognise a new symptom or a symptom that has changed significantly and seek prompt and early consultation with healthcare professional when there are associated symptoms such as fever or neurological signs. 40
Headaches can be severe and interfere with day-to-day activities without proper treatment. 41, 42 Primary headache disorders can be effectively managed in most cases by patients themselves that may help reduce attack frequency and severity and lessen impact. 5, 43 Educating people and increasing awareness of the common headache disorders and advising patients on when to consult or self-treat with over-the-counter pain medications is important. 3
The rationale for promoting self-management interventions is that people can learn ways to help themselves to manage their headaches better which can have a positive effect on physical symptoms as well as functional capacity. These interventions could be with or without conjunctive pharmacological therapy (acute and prophylactic medication) like identifying and managing controllable triggers, relaxation exercises, effective stress management, activity pacing, good sleep, talking effectively about pain with family and others. 44, 45 Self-management may be effective in improving pain intensity, headache-related disability, quality of life and medication consumption and also improve mood (anxiety and depression). Self-management interventions for migraine and TTH are more effective than usual care in reducing pain intensity, mood and headache-related disability, but have no effect on headache frequency. Cognitive behavioural therapy, mindfulness and education about interventions, which is delivered in groups may be more effective. 44
Self-management for migraine and TTH can be used either alongside pharmacological interventions or as a stand-alone therapy, mostly when other treatment options have failed or a non-pharmacological intervention is preferred. Group interventions (cognitive behavioural approach, mindfulness and educational components) may be more effective than alternative intervention. 44, 46
Self-care activities are an important part of comprehensive treatment especially in the treatment of migraine, where it could help get positive results by decreasing disability and saving treatment costs for patients.47 Self-care with simple analgesics is all that is required for most people with headache which is one of the commonest reasons for self-medication most of the time. 40
Conventional vs. Routine medications in managing headache
Analgesics, anti-emetics, specific anti-migraine medications, and prophylactic medications are the main classes of drugs to treat headache disorders.6 The pharmacological options for managing headache disorders are based on the subtypes. Acute tension-type headaches may improve with ibuprofen and high-dose acetaminophen and amitriptyline may be used as preventive measure in tension-type headaches after 3 months of treatment. NSAIDs (ibuprofen, naproxen, aspirin, and high-dose acetaminophen) and triptans are effective for acute relief of migraine. Intravenous magnesium and greater occipital nerve blocks are also effective. The effective preventive for migraine are candesartan, telmisartan, lisinopril, oral magnesium, topiramate, propranolol, erenumab, fremanezumab, and galcanezumab. The frequency of cluster headache may be reduced with galcanezumab and acute cluster headaches can be improved with triptans and oxygen. 48
More than 50% of the patients with migraine and more than 80% of the patients with TTH worldwide choose over-the-counter (OTC) medications to prescription medications to manage their condition. This could be due to wide variation in symptom severity from person-to-person and attack-to-attack that could be mild pain with little disability to severe pain with complete disability especially in those with migraine or TTH which may not be typically associated with debilitating pain or functional impairment. Also, the prescription drugs are more costly, more likely to have contraindications or undesirable side effects compared to OTC medications. Evidence-based guidelines have endorsed OTC drugs to be safe and effective treatment options for acute treatment of migraine and TTH. Many agents available OTC, including acetaminophen and also fixed combinations of analgesics with caffeine have established efficacy in managing TTH and migraine in well-controlled trials. 22
What do guidelines recommend
Paracetamol has been recommended as a 1st line drug in pain management guidelines. It is being used for the treatment of headache and migraine for a long time and is recommended by most international societies. The American Academy of Neurology and the American Headache Society considers oral paracetamol used alone or in combination to be effective in migraine. The American Academy of Family Physicians and the American College of Physicians–American Society of Internal Medicine, and the Ad Hoc Committee of the Italian Society for the Study of Headaches for the Guidelines of Primary Headaches in adults all recommend paracetamol for treatment of migraine. The European Federation of Neurological Societies supports paracetamol as 1st line treatment for tension-type headache. 49
Based on the efficacy and tolerability of paracetamol, the British Association for the Study of Headache (BASH) guidelines recommended it as a 1st line choice in evidence based guidelines for several conditions causing mild to moderate pain and TTH. 50
The German, Austrian and Swiss Headache Societies and the German Society of Neurology recommend paracetamol as a 1st line option for self-medication of migraine attacks and paracetamol and caffeine combination is recommended as 1st line therapy for TTH. 43
The American Headache Society recommends the use caffeinated analgesic combination (aspirin plus acetaminophen plus caffeine) for mild-to-moderate migraine attacks. 51
As per the Indian guidelines, NSAIDs, non-opiate analgesics and combination analgesics containing caffeine are a reasonable 1st line treatment choice for mild-to-moderate or severe migraine attacks responsive to similar NSAIDs or nonopiate analgesics in the past.52
Paracetamol and Caffeine in Managing Headache
Paracetamol (PCM)
Is used as over the counter (OTC) medication and as a prescription medication for managing pain. The clinical pharmacological profile of PCM is that of a potent analgesic and antipyretic with little/ or no anti-inflammatory activity and with very minor side effects (gastrointestinal, renal, or vascular). Although its mechanisms of analgesic activity is not fully understood, its site of action is peripheral and central nervous system. It can affect the central neurotransmission of pain in different ways. It is metabolized to N-arachidonoylaminophenol (AM404), a compound with multiple potential analgesic activities, including the blockade of neuronal uptake of anandamide and of neuronal sodium channels. It is found to decrease the tissue concentrations of prostaglandins and pro-inflammatory mediators. 49
Paracetamol, a non-opioid, centrally acting analgesic is available in a wide range of OTC preparations in different doses and in a variety of formulations and combinations 53 to treat acute primary headaches. It may be used alone or in combination with aspirin, caffeine and tramadol to treat acute primary headaches. 54
Paracetamol is effective and safe for post exodontia pain and sufficient pain control is achieved with following a dosage of 500 mg thrice a day provided surgical trauma to the investing tissues is minimal. 55 Paracetamol is still the most widely used analgesic–antipyretic agent and is the first choice drug by many for pain management and control of fever including children, pregnant women, and elderly. It is safe in OTC doses for treatment of colds and flu and there is no evidence that it prolongs the course of colds and flu by any effect on the immune system or by reducing fever. 56 Paracetamol is effective in relieving the pain of large joint OA and is considered a 1st line oral analgesic for managing OA. 57 Paracetamol, though more than a century since its first clinical use, still continues to be used as the first-line therapy for managing pain and is recommended for all including children, pregnant women and elderly, for simple headaches, osteoarthritis, and non-inflammatory musculoskeletal conditions. 58
As per the NIH, acetaminophen is used to relieve mild to moderate pain from headaches, muscle aches, menstrual periods, colds and sore throats, toothaches, backaches, and reactions to vaccinations and to reduce fever, and to relieve the pain of osteoarthritis. 51 Paracetamol is available in various formulations and dose forms -325 mg, 500 mg, 650 mg and 1g.59 The usual oral dose for adults is 0.5g to 1g every 4-6 hours up to a maximum dose of 4g daily. 53 The standard adult dose of paracetamol is 500 to 1000 mg, and the maximum recommended daily dose is 3 to 4 g for adults. 49, 60, 61
Paracetamol in a dose range of 650–1300 mg is found to be effective in relieving mild to moderate pain like headache, toothache, dysmenorrhoea, and a variety of post-surgical pain. 56
Paracetamol in therapeutic doses is a safe analgesic. It is rapidly absorbed from the gastrointestinal tract after oral administration. The rate of oral absorption is predominantly dependent on the rate of gastric emptying. Its systemic bioavailability is dose-dependent that ranges from 70 - 90%. It distributes rapidly and evenly throughout most tissues and fluids and has a volume of distribution of approximately 0.9L/kg. About 10 - 20% of the drug is bound to red blood cells. It is extensively metabolised in the liver to sulphate and glucuronide conjugates. About 85 - 95% of a therapeutic dose is excreted in the urine within 24 hours in healthy subjects. 62 Because of its good safety profile, it is recommended especially for aged and frail patients. 49 There is no need for dose reduction for older people. The risk of harm should be considered when recommending it to frail older people and those with impaired liver function. 63 There is no evidence to support a higher incidence of hepatotoxicity of paracetamol in normal dosages in elderly subjects. 64
Oral paracetamol has the potential to reduce pain in various conditions. It is the analgesic of choice for patients in whom salicylates or other NSAIDs are contraindicated (asthmatics, salicylate allergy, history of peptic ulcer and patients with CKD). 65 Stephens G and co-workers assessed the efficacy and safety of paracetamol in a review of drugs (Cochrane Database of Systematic Reviews) used for acute treatment of frequent episodic tension‐type headache (TTH) in adults and compared 500 or 650 mg of paracetamol with placebo, and paracetamol 1000 mg with other painkillers. They found no difference between any of these treatments. About 10 in 100 people benefited because of paracetamol 1000 mg, the benefit was small in terms of being pain free at 2 hours for people with frequent episodic TTH who have an acute headache of moderate or severe intensity. 66
There is a general consensus that analgesics, especially NSAIDs are to be taken with food to reduce unwanted gastrointestinal adverse effects. 67 Paracetamol is an effective and very safe analgesic that does not cause gastrointestinal mucosal injury like the NSAIDs. It is devoid of any gastrointestinal (GI) ulcerogenic potential and is suitable for patients at high risk of developing GI ulcers or bleeds. Much of the toxicity of therapeutic doses of non-selective NSAIDs is not seen with paracetamol. Paracetamol has an apparent COX-2 selectivity of action with poor anti-platelet activity and good gastrointestinal tolerance and does not cause significant gastrointestinal toxicity at therapeutic doses. 68 At high doses, it may induce upper GI symptoms such as abdominal pain/discomfort, heartburn, nausea or vomiting, but is devoid of risk for GI ulcers and ulcer complications. 69 Paracetamol lacks major GI toxicity in short-term use and has GI safety superior to that of many NSAIDs. 60 Unlike the NSAIDs, acetaminophen can be taken on an empty stomach as food may slow its absorption. 70
Paracetamol exerts its analgesic activity through a direct effect on the central nervous system at least in part mediated by the serotonergic system. Due to its scarce inhibition of peripheral cyclooxygenase it is better tolerated at gastrointestinal level than NSAIDs, it is only a weak inhibitor of platelets aggregation and does not alter the bleeding time. 71
Acetaminophen is an effective and well-tolerated treatment for episodic and moderate migraine headache which also provides a beneficial effect on associated symptoms of migraine like nausea, photophobia, phonophobia, and functional disability generally. In a randomized, placebo controlled, double-blind clinical trial (6 hours duration, OPD setting) by Prior MJ and co-workers about 52% of patients treated with acetaminophen 1000 mg reported mild to no pain after 2 hours vs. 32% with placebo. The mean pain intensity difference from baseline at 2 hours was significantly greater with acetaminophen 1000 mg (0.82) vs. placebo (0.46) [P < 0.001]. Both primary endpoints at 1 hour after treatment was maintained throughout the 6-hour study period. 72
Caffeine
Caffeine (1,3,7-trimethylxanthine), is probably the most frequently ingested pharmacologically active substance in coffee, tea, soft drinks, products containing cocoa or chocolate, and medications including headache or pain remedies available over-the-counter worldwide. It is completely absorbed from the gastrointestinal tract following ingestion, reaches a maximum concentrations within 1–1.5 hours and is readily distributed throughout the body. It is metabolized in the liver to 1- methylxanthine and 1-methyluric acid from the paraxanthine intermediate and only 1–5% of ingested caffeine is excreted unchanged in the urine. 73 The elimination half-life in healthy individuals is about 5 hours (1.5 - 9.5 hours) that can be influenced by factors such as sex, age, use of oral contraceptives, pregnancy and smoking, obesity, altitude etc. The total plasma clearance rate is 0.078 L/h/kg. 73, 74
Caffeine has been used as an analgesic drug adjuvant and has shown to have intrinsic antinociceptive action which is most likely to occur through the blockade of adenosine A2a and A2b receptors. Its effect as an adjuvant with analgesic is due to the change in the activity and synthesis of cyclooxygenase enzymes in certain sites. 75
Caffeine as an analgesic adjuvant enhances the action of PCM
Caffeine, either alone or in combination with other agents has been used worldwide for decades in both OTC and prescription analgesic combinations. 22, 76 Caffeine has shown to enhance early absorption of acetaminophen. The administration of caffeine and paracetamol is superior in reducing the subjective perception and objective (pain-related evoked potentials) measurement of pain. 77 Caffeine has shown to increase and prolong analgesic effect of paracetamol through pharmacodynamic interaction. 75 The mechanisms by which caffeine contributes to or enhances the efficacy of other analgesics is not well understood, but it could be due to: 76, 78
Improved drug absorption through lower gastric pH and increased gastric blood flow.
Reduced metabolic clearance of drugs through reduced hepatic blood flow.
Blockade of peripheral pro‐nociceptive adenosine signalling, and activation of the central nor adenosine pathway (pain‐suppressing systems).
Transcriptional down‐regulation of cyclo‐oxygenase‐2 (COX‐2), via blockade of the adenosine A2a receptor.
Relief of inhibitor adenosine actions on central cholinergic nerve terminals.
Changes in mood and emotional state contributing to changes in the perception of pain.
Caffeine is known to significantly enhance the effectiveness of analgesics and NSAIDs in the treatment of patients with migraine and TTH. In most patients who use caffeine-containing OTC combinations for occasional, acute treatment of TTH or migraine the tolerability is good with appropriate use. Available evidence indicates that combining caffeine with acetaminophen significantly improves efficacy over use of only analgesics. The tolerability is generally good for the vast majority of patients and adverse effects are predictable and are generally mild and transient. Combination of caffeine with analgesic medications like acetaminophen have shown to significantly improve efficacy in vast majority of patients in the treatment of patients with TTH or migraine. 22
In TTH, the magnitude of the adjuvant effect from caffeine for the summed pain intensity difference (SPID), %SPID, and total pain relief (TOTPAR) was between 76 - 97%; for measures of peak analgesia and duration of analgesia, the effects were 63–85% greater than the net analgesic effect of acetaminophen monotherapy. Compared to acetaminophen 1000 mg plus placebo, AAC (acetaminophen 500 mg, aspirin 500 mg, and caffeine 130 mg per 2-tablet dose) provided significantly superior total pain relief at 4-h post dose (P < .001 vs. APAP and placebo) [Table 2]. The efficacy of AAC (acetaminophen 500 mg, aspirin 500 mg, caffeine 130 mg per 2-tablet dose) in migraine is established with a significant advantages of AAC over placebo at 2- and 6-h post dose for relief of pain, associated symptoms, and disability (Table 3).22
Table 2
Pooled results from 2 TTH trials in patients over 4 h for AAC-130, APAP, and placebo 22
Table 3
Pooled results from 3 migraine trials: AAC-130 vs. placebo for migraine at 2 and 6 h post dose 22
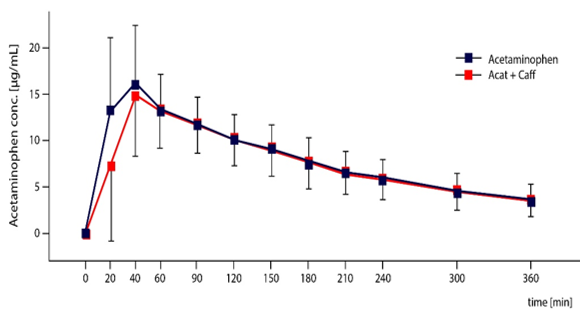
Caffeine enhances early absorption of acetaminophen and increases vigilance and arousal. In combination with acetaminophen it is significantly superior in reducing perceived tonic pain and pain-related evoked potentials compared to acetaminophen or caffeine alone. 79 Caffeine, a common additive to analgesic drugs increases the analgesic potency of paracetamol by 41%. 80 Caffeine enhances the analgesic efficacy of paracetamol in combination by pharmacodynamic interactions rather than pharmacokinetic interactions. 81 Caffeine causes sustained anti-nociception-enhancing effect when given with acetaminophen. It accelerates absorption of acetaminophen that is seen as enhanced early AUCs (Figure 3). In vitro dissolution tests revealed a faster dissolution for acetaminophen compared to formulation, including caffeine, and deconvolution of averaged in vivo plasma concentrations for both formulations indicated a higher and faster absorption rate for acetaminophen in combination with caffeine. 79
Figure 3
Increased early AUCs: Faster absorption rate after administration of the caffeine formulation 79
The combination of paracetamol (1,000 mg) and caffeine (130 mg) seems to be as efficient and safe as sumatriptan (50 mg) in treatment of patients with migraine. Pini and co-workers assessed the efficacy of the combination with the gold standard sumatriptan by the sum of pain intensity differences, the curve of mean pain intensity, the number of pain free at 2h, and the total pain relief in a multi-center randomized double-blind, double-dummy, cross-over controlled trial. Both the treatments were effective with respect to the baseline and there was no differences between the treatments. The time course of total pain relief (TOTPAR) was similar and rescue medication was needed in 38 % of those with paracetamol treatments and 45 % with sumatriptan treatment, without significant differences (Fisher exact test: p = 0.3308). 71
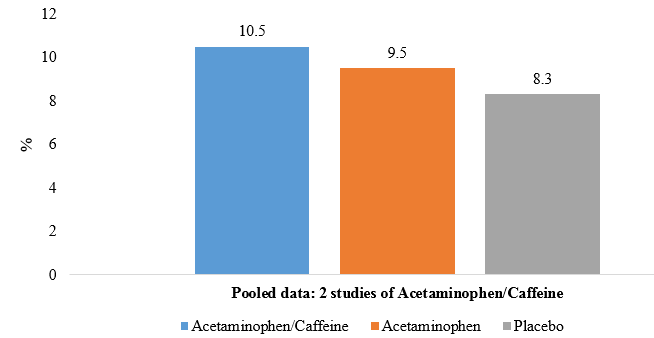
Migliardi and co-workers compared the efficacy of two analgesic combinations containing caffeine with an acetaminophen [acetaminophen (500 mg) plus aspirin (500 mg) plus caffeine (130 mg)] and acetaminophen (1,000 mg) plus caffeine (130 mg)] with a placebo, in patients with episodic TTH in randomized, double-blind, and period crossover studies conducted under similar protocols. The pain was rated by the patients using the VRS-4. Caffeine-containing analgesics were found to be superior to placebo and acetaminophen was significantly superior to placebo in all studies (Figure 4). The significant analgesic adjuvant effect of caffeine was independent of patients’ usual caffeine use or their caffeine consumption in the 4 hours before medication. 82
Figure 4
Pooled TOTPAR scores from two studies of acetaminophen/caffeine vs. acetaminophen, and placebo. 82
TOTPAR: Pooled mean total pain relief; APAP: Acetaminophen CAF: Caffeine
Combination of PCM and caffeine in pre- and post-operative pain
A double-blind, cross-over trial by Wojcicki J and co-workers evaluated the 3 analgesic preparations: paracetamol, paracetamol with caffeine (Finimal) and aspirin in the relief of postoperative pain in 72 orthopaedic inpatients and 144 ambulatory outpatients with idiopathic headache. They found combination of paracetamol and caffeine to have the greatest pain relief in both groups of patients. Paracetamol-caffeine combination was found to be superior to paracetamol alone or aspirin. 83
Combination of PCM + Caffeine in relief of dental pain
A review of 3 controlled clinical trials by Abou-Atme and co-workers showed that the combination of acetaminophen and caffeine is efficacious for the management of dental pain. It was found to be superior to acetaminophen alone, similar to ibuprofen, and slightly inferior to acetaminophen and codeine. Caffeine with analgesic medications seems to provide a synergetic analgesic effect. 84
Paracetamol (PCM) + caffeine better than PCM + Propyphenazone(PPZ) + Caffeine in dental pain
A double-blind, randomized parallel group study among adult out-patients (18 - 70 years) with dental pain following small dental surgery (e.g. extraction of an impacted wisdom-tooth or dental implant) compared the efficacy and the onset of pain relief with a formulation containing 250 mg Paracetamol + 150 mg Propyphenazone + 50 mg Caffeine vs. the combination of 500 mg Paracetamol + 50 mg Caffeine. The doses for both was 1 capsule at the onset of dental pain following the surgery and a 2nd capsule could be taken 30 minutes later and the following doses of 1 - 2 capsules, as needed, up to 6 capsules per 24h. Patients on 250 mg Paracetamol + 150 mg Propyphenazone + 50 mg Caffeine combination took more frequently a second capsule than those on Paracetamol 500 mg + Caffeine 50 mg. Patient rating for efficacy was more favourable for combination of Paracetamol 500 mg + Caffeine 50 mg vs. combination of 250 mg Paracetamol + 150 mg Propyphenazone + 50 mg Caffeine (p=0.009). 85
It was observed that a 500 mg PCM + 50 mg caffeine formulation for oral use disintegrates 3 times faster than a 300 mg PCM + 150 mg PPZ + 50 mg caffeine formulation. While a 500 mg PCM + 50 mg caffeine formulation takes around 2 minutes to disintegrate, a 300 mg PCM + 150 mg PPZ + 50 mg caffeine formulation takes around 7 minutes to disintegrate. A faster disintegration time typically contributes to a typically translates to a faster onset of action. 86 Faster disintegration and gastric emptying of paracetamol leads to its faster rate of absorption. 87
Pain care guide for managing headache for pharmacist in primary care
Pharmacists can help patients seeking guidance on the self-treatment of headaches, and also evaluate patients to ascertain if self-treatment is appropriate. When warranted patients should be encouraged to seek further medical care from their primary health care providers. 8
Patient care guide for managing headache
Pharmacist-led management for relief of headache. 40, 88, 89, 90, 91, 92, 93, 94
Assess #
Site: Where is the headache?
Onset: How quickly did it come and was it preceded by other symptoms?
Character: Ask the patient to describe the pain
Radiation: Does the pain go anywhere?
Associated features: nausea, vomiting, sensitivity to motion, sound, light, weight loss, fever, night sweats, any triggers* that contribute to headache
Timing: For how long does the headache last?
Exacerbating or relieving factors
Severity of headache: Does it interfere with daily life activities.
Recommend appropriate management
Simple analgesics if frequency of headache is low and the symptoms are not disabling. • Paracetamol plus caffeine/Other NSAIDs.
Before recommending any analgesics.• Enquire about potential allergies.
Headache is persisting and is interfering with daily life. • See a doctor.
Table 4
Features of primary headache disorders
Table 5
Basics of headache self-management 95
|
Manage triggers |
Manage stress |
Manage emotions |
Minimize intensity and impact |
Empower patients
Inform: Proper use of analgesics (duration, how to take it i.e. with/ without food; potential adverse effects)
Advice patients to consult a physician before using analgesics esp. in pregnant/ lactating women, patients on any other medications or with a pre-existing medical condition.
Recommend preventive measures: Relaxation techniques, avoiding stress, eating a balanced diet, and getting an adequate amount of sleep
Advice patients to seek medical care - If no relief of pain, chronic headaches, or increase in intensity or frequency of headache.
*Triggers: Stress, anxiety, environmental factors (noise, poor lighting conditions when reading or using a computer), change in sleep pattern (not getting enough sleep) and eating patterns (skipping meals), use of certain pharmacologic agents, fluctuations of hormone levels, and food sensitivities.
# Features of primary headache disorders (Table 4)
Self-management tips for primary headache 95, 96, 97
Make lifestyle changes i.e., stress reduction, regular eating and sleeping schedules, and regular exercise schedule to minimize the frequency of your headaches.
Keep a headache diary' to help identify what's causing your headache.
Seek care from medical professional and learn about triggers to avoid the potential triggers in future.
Try treating your headache with suitable pain-relieving medicine like the over-the-counter medications for mild headaches like Paracetamol plus caffeine/ Other NSAIDs
Take prophylactic treatment to prevent attacks of frequent and severe headache.
Try remedies like resting and relaxing or trying to sleep, taking a warm bath, applying a heat pack or taking a massage.
Do not use headache medicines for > 9 days a month to avoid overuse of analgesics and risk of chronic daily headaches.
Consult your doctor if the symptoms persist or you get frequent headaches to find out the underlying cause and avoid recurring headache.
Conclusion
Headache disorders are highly prevalent conditions that can be disabling at times. It can have a significant impact on an individual’s quality of life, resulting in huge costs to healthcare and the economy. Headache is classified as primary headache that has no known underlying cause and secondary headache that is due to another condition causing traction due to inflammation of pain-sensitive structures. Majority of the patients presenting with headache in primary care have a primary headache disorder.
Headache disorders are one of the major public-health concerns globally are amongst the most prevalent and disabling conditions. It causes substantial rates of absenteeism and lost productivity. There is a strong relationship between stress and headache and often patients with headache report stress to be the cause for their headache and headache itself could be a stressor. Headache that is chronic or recurring can have an effect on quality of like of the individual with decreased functional capacities, lost working hours and reduced productivity. Headache disorders do impose a considerable burden on the sufferers and can have substantial personal impact, impaired quality of life and also incur greater cost.
Headache is one of the commonest conditions that people treat without professional advice and can be easily managed with simple analgesics. People can learn ways to help themselves to manage their headaches better which can have a positive effect on physical symptoms as well as functional capacity. Professional help is needed when the symptoms are unmanageable with simple analgesics. Headaches can be managed with OTC drugs that are safe and effective treatment options for acute treatment of migraine and TTH. Paracetamol (acetaminophen) is one of the most popular drugs used worldwide, and is often used in combination with other drugs. The combination of acetaminophen and caffeine acts on distinct molecular targets and more signalling cascades of pain compared to single analgesics. Caffeine is known to augment the action of the analgesic in combination and the combination with paracetamol is found to be more effective than paracetamol alone in the treatment of primary head ache disorders. Combining caffeine with acetaminophen significantly improves efficacy over the use of only analgesics. Caffeine has shown to increase the analgesic potency of paracetamol and causes sustained anti-nociception enhancing effect with acetaminophen. The combination of paracetamol and caffeine are found to be more effective than paracetamol alone in the treatment of primary head ache disorders.