- Visibility 199 Views
- Downloads 39 Downloads
- DOI 10.18231/j.ijn.2022.044
-
CrossMark
- Citation
Surgery for Lumbar disc prolapse in pregnancy: Case series
- Author Details:
-
Rajesh Kumar Bharti *
Case Report 1
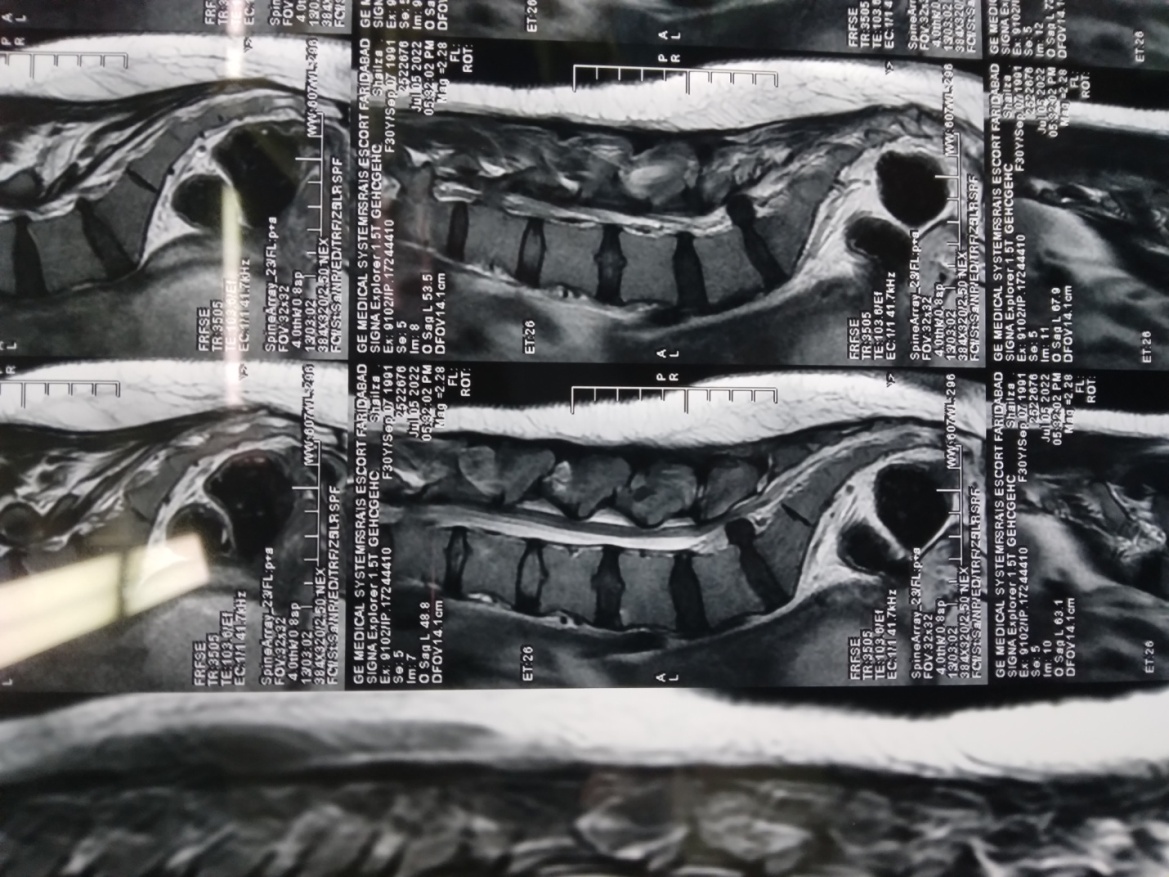
A young lady of 32 years, known case of Hypothyroidism with 16 weeks pregnancy of gestation presented with complaints of severe low back pain, radiating pain to Lt. Lower limb associated with weakness of lower limb. Examination revealed restricted SLR (Lt.) of 300, Lt. Plantar flexor of 3/5, with hypo-aesthesia in Lt. S1 dermatome, VAS (visual analogue score for pain) of 9/10. MRI Lumbo-sacral spine ([Figure 1], [Figure 2]) revealed extruded & superior migration of L5-S1 intervertebral disc, predominantly in the left paracentral location. Her obstetrical history G2P1L0, POG 16+5weeks, per abdomen uterus of 14-16 weeks size, fetal heart sound was regular. USG Doppler of both lower limbs was normal. TSH 16.25 micro IU/ml, FT3 2.01 pg/ml, FT4 1.40 ng/dl. Physician consulted for hypothyroidism, Thyroxine dosage increased to 200 mcg.
Patient put in prone position with careful placement of padded rolls under the chest & pelvis to avoid compression on the gravid uterus and care was taken for all pressure points. Clinically, L5-S1 disc space localized, using anatomic landmarks. The L4/5 disc inter-space is commonly believed to be represented by a line drawn between the two highest points of the iliac crests. This line is frequently used as a pre-operative guide for incision placement, in patients undergoing spinal surgery. Usually, we use intraoperative fluoroscopy to confirm the disc space but here, Intraoperative localization done using clinical judgement. L5 laminotomy on Lt. side done, ligamentum flavum excised, Lt. S1 nerve root along with thecal sac were gently retracted, and found extruded, desiccated disc fragment causing compression of Lt. S1 nerve root. Traversing nerve root was swollen & hyperemic, and it became lax after diskectomy. There were no dilated epidural vessels, hemostasis was perfect.
Post-operatively VAS 1/10, no fresh neuro-deficit.
It was a precious pregnancy, lady was under regular antenatal checkup, developed gestational hypertension and at 31 weeks + 4 days POG had preterm labor pains with abruptio-placenta. She went into spontaneous labor and had preterm vaginal delivery, alive baby boy of 1.58 kg born. She had no neurodeficit.
Case Report 2
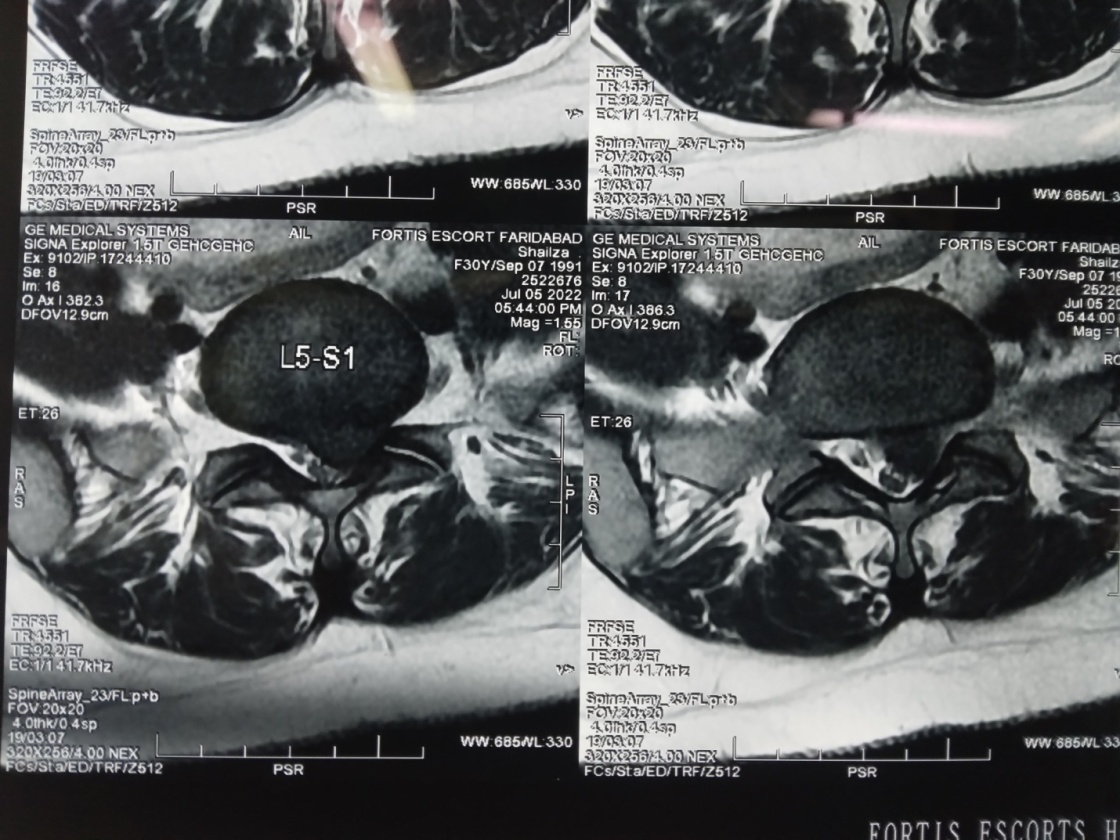
A 30 years lady, 16 weeks pregnant, presented with complaints of acute onset low back pain, radiating pain to left lower limb, weakness and numbness in lower limb for the last 2 days. She had difficulty in walking. Examination revealed Lt. SLR 300, Lt. EHL/DF - 4/5, AF - 3/5, Hypoaesthesia Lt. S1 dermatome by 30%, compensatory scoliosis to left. MRI LS spine ([Figure 3], [Figure 4]) revealed Lt. L5-S1centrolateral disc prolapse. Patient was advised surgery and risks of anaesthesia, positioning & surgery; regarding fetal miscarriage had been explained to the patient and relatives. After informed consent, she was taken up for microdiskectomy surgery in Lateral decubitus position with Lt. side up. Laminotomy of left side L5 performed. S1 nerve root was found swollen and hyperemic, stretched by underlying large disc fragments, microdiskectomy done. Traversing nerve became lax after microdiskectomy. Patient withstood procedure well and became pain free postoperatively. Gynaecologist consulted, Fetal heart sound were regular.



Case Report 3
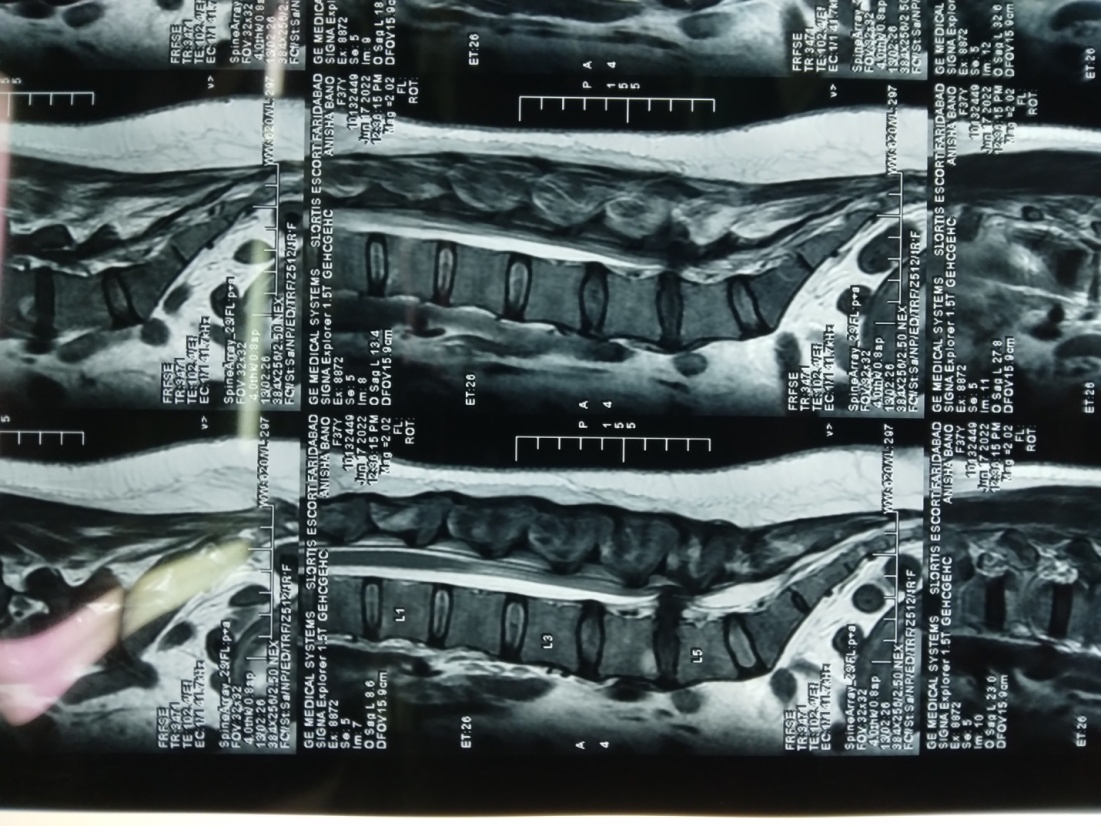
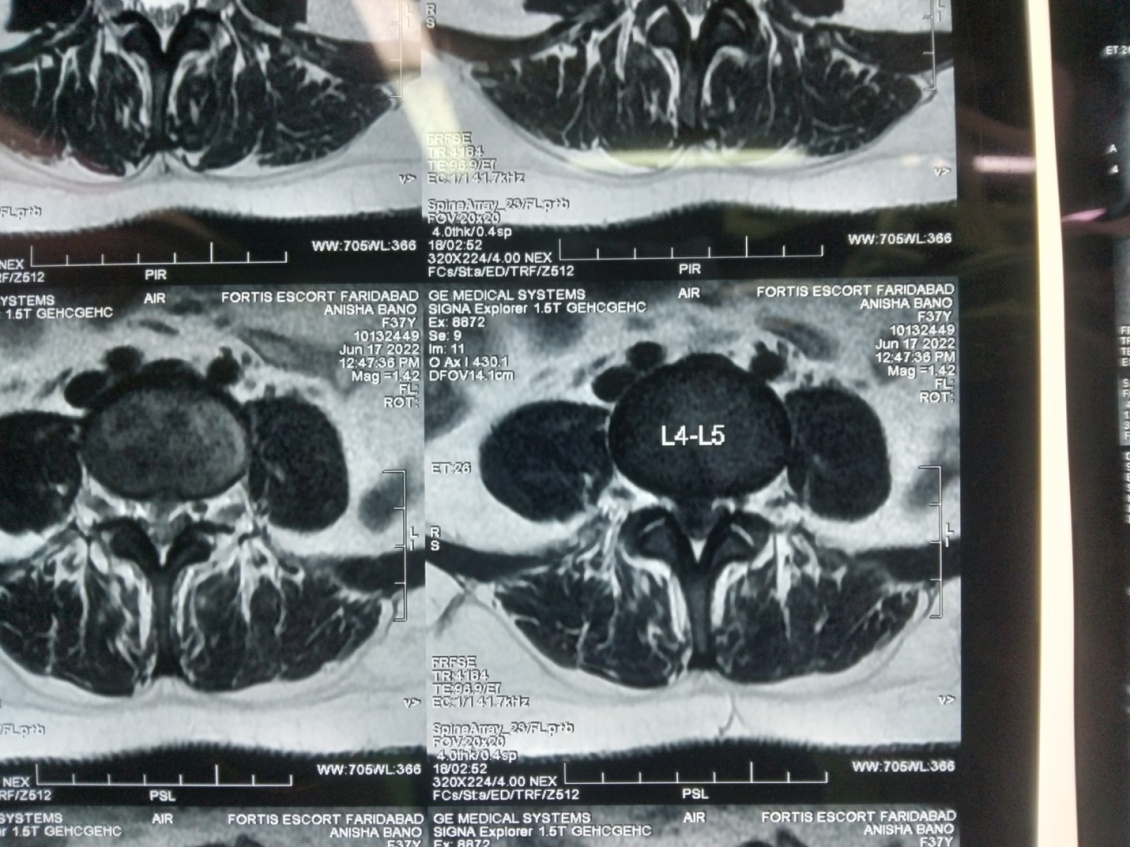
A 37 years lady, with 5 weeks pregnancy of gestation, by IVF and it was a precious pregnancy; came with complaints of low back pain, radiating pain Lt. lower limb, urinary and bowel incontinence, Examination revealed perianal anaesthesia, anal reflex was absent.
MRI LS pine ([Figure 5], [Figure 6]) revealed L4-L5 large central disc prolapse. She had cauda equina syndrome due to large central disc prolapse, so advised emergent surgery; but patient and her husband were not willing for surgery and left the hospital against medical advice. 2 days later, she came in emergency as her complaints were not relieved and now she became willing for surgery. It was informed to the patient and her husband that her cauda equina symptoms were not relieved/came to normal,due to so much delay & also, about the high risk of miscarriage. L4/5 microdiscectomy was performed in prone position, no intraoperative fluoroscopy was used. A large central extruded disc retrieved ([Figure 7]). Her Low back pain and radicular pain was relieved but she remained urinary and bowel incontinent. She had miscarriage on 2nd post-operative day.
Discussion
MRI is considered the gold standard diagnostic investigation, in patients suffering from spinal pathology. American College of Radiology recommends to avoid MRI during the first trimester and to never use of intravenous Gadolinium contrast agent. When MRI is necessary in the first trimester, the risks and benefits should be judged and discussed with the expectant mother and family, to make an informed choice.[1], [2], [3]
According to the American Congress of Obstetricians and Gynecologists (ACOG) guidelines, MRI is not associated with adverse fetal effects, and the use of paramagnetic contrast agents (gadolinium) during MRI has not been studied in pregnant women but animal studies have demonstrated increased rates of spontaneous abortion, skeletal, and visceral abnormalities when given at two to seven times the recommended human dose. [4] Exposure to X-rays can result into teratogenic effects, carcinogenesis, genetic alteration or mutations in germ cells.
Absolute indications of diskectomy during pregnancy are cauda equina syndrome, progressive neurologic deficit, as postponement to perform the surgical procedure may result into permanent deficits. Elective surgery should not be performed during pregnancy. Surgery should be avoided in the first trimester, which is the period of organogenesis. The risk of preterm labor is considered lowest in second trimester, so that period is optimal to perform surgery. [5] Mazze and Kallen studied 5,045 patients who underwent a non-obstetric surgical procedure during pregnancy; their results revealed similar rates of congenital anomalies and stillbirth to those of pregnant patients not underwent to any surgical procedure. [6]
In the case of surgery on pregnant women, there is uncertainty as to how often and to what extent intraoperative fluoroscopy is possible. In cases when extensive fluoroscopy is unavoidable, such as polytrauma patients, the indication for induced abortion should be discussed with the patient. Operative positioning should be chosen according to the gestational age and location of the lesion. For spine surgery, various studies recommend the prone position in the first and early second trimester, because there is only minimal aortocaval compression by the gravid uterus. [7] After 12 weeks of gestation, left lateral position is recommended, so as to avoid aortocaval compression. [8] Tilting the operating table may be helpful, in case of limited or restricted operative field.
Acetaminophen and some opiates are suitable medications for pain relief during pregnancy, although recent reports of adverse fetal side effects after prolonged long-term maternal use have been reported. [9], [10]
General anesthesia poses risk to both the mother and the fetus, like aspiration, preterm labor. For these reasons, many anesthesiologists try to avoid general anesthesia if at all possible and instead use regional anesthetics. However, Brown and Brookfield reported in a case report that in case of root compression by disc herniation with neurologic compromise, regional anesthesia may worsen the preexisting neurologic deficit. [11] The goals of anesthetic management in pregnant women are maternal safety and avoidance of fetal hypoxia and early labor. Benzodiazepines have been correlated to fetal malformation and should be avoided during anesthesia. [12]
In our case, patient had VAS 9/10 and developed neurologic deficits, for which we offered her L5-S1 microdiskectomy surgery. It was a precious pregnancy due to increased age, hypothyroidism, so all pros & cons of general anesthesia, surgery were discussed with the patient and her family, with informed consent, we performed microdiskectomy in prone position with careful placement of padded rolls under the chest & pelvis to avoid compression on the gravid uterus. No fluoroscopy was used,disc space localized using clinical judgement. During surgery there were no epidural venous engorgement or excessive bleeding, Surgery was uneventful, Post-operatively her VAS 1/10, with no fresh neuro-deficit. She was under regular antenatal checkup, developed gestational hypertension and at 31 weeks + 4 days POG had preterm labor pains with abruptio-placenta. She went into spontaneous labor and had preterm vaginal delivery, alive baby boy of 1.58 kg born. She had no neurodeficit.
In our 2nd case we placed the patient in lateral decubitus position and fluoroscopy was not used. Surgery went smoothly and she made good recovery post-operatively. Fetal heart rate was also normal.
3rd case was conceived by IVF, a precious pregnancy, came in first trimester with cauda equina syndrome, her neurological deficit (Urinary and fecal incontinence) didn’t improve and had miscarriage on 2nd post-operative day.
Katz et al proposed that until 20 weeks of gestation, there is no need for monitoring the fetal heart sound during surgery; from 20 to 23 weeks, monitoring is debatable and is mandatory from the 23rd week onwards. [13] An endoscopic diskectomy, has also been described as a safe and effective approach in a pregnant patient. [14]
Conclusion
Surgery in pregnancy is a relatively compromised state, in terms of radiologic investigation, medication, surgical timing, positioning on operating table, anesthesia; in respect for maintaining well being of fetus and the mother and progression of safe gestation. Surgery in first trimester, carry high risk of miscarriage.
If due care is taken, then neurosurgical procedures of short duration can also be done safely in second trimester of pregnancy, in justifiable neurosurgical pathologies. Lateral decubitus position is relatively safe in terms of positioning gravid uterus and also for the anaesthetist.
Source of Funding
None
Conflict of Interest
Author declare no conflict of interest.
References
- MM Laban, NS Rapp, P Von Oeyen, JR Meerschaert. The lumbar herniated disk of pregnancy: a report of six cases identified by magnetic resonance imaging. Arch Phys Med Rehabil 1995. [Google Scholar] [Crossref]
- PI Wang, ST Chong, AZ Kielar, AM Kelly, UD Knoepp, MB Mazza. Imaging of pregnant and lactating patients: part 1, evidence-based review and recommendations. AJR Am J Roentgenol 2012. [Google Scholar] [Crossref]
- FG Shellock, J Crues. MR procedures: biologic effects, safety, and patient care. Radiology 2004. [Google Scholar] [Crossref]
- . ACOG Committee Opinion. Number 299, September 2004 (replaces No. 158, September 1995). Guidelines for diagnostic imaging during pregnancy. Obstet Gynecol 2004. [Google Scholar] [Crossref]
- K Hayakawa, J Mizutani, N Suzuki, C Haas, A Kondo, S Otsuka. Surgical management of the pregnant patient with lumbar disc herniation in the latter stage of the second trimester. Spine (Phila Pa 1976) 1976. [Google Scholar] [Crossref]
- R I Mazze, B Kallen. Reproductive outcome after anesthesia and operation during pregnancy: a registry study of 5405 cases. Am J Obstet Gynecol 1989. [Google Scholar] [Crossref]
- A Kathirgamanathan, A D Jardine, D M Levy, M P Grevitt. Lumbar disc surgery in the third trimester-with the fetus in utero. Int J Obstet Anesth 2006. [Google Scholar] [Crossref]
- VI Vougioukas, G Kyroussis, S Glasker, M Tatagiba, KM Scheufler. Neurosurgical interventions during pregnancy and the puerperium: clinical considerations and management. Acta Neurochir (Wien) 2004. [Google Scholar] [Crossref]
- R E Brandlistuen, E Ystrom, I Nulman, G Koren, H Nordeng. Prenatal paracetamol exposure and child neurodevelopment: a sibling-controlled cohort study. Int J Epidemiol 2013. [Google Scholar] [Crossref]
- B Kallen, M Reis. Use of tramadol in early pregnancy and congenital malformation risk. Reprod Toxicol 2015. [Google Scholar] [Crossref]
- MD Brown, KF Brookfield. Lumbar disc excision and cesarean delivery during the same anesthesia. A case report. J Bone Joint Surg Am 2004. [Google Scholar]
- L Iyilikçi, S Erbayraktar, A N Tural, M Celik, S Sannav. Anesthetic management of lumbar discectomy in a pregnant patient. J Anesth 2004. [Google Scholar] [Crossref]
- J D Katz, R Hook, P Barash. Fetal heart rate monitoring in pregnant patients undergoing surgery. Am J Obstet Gynecol 1976. [Google Scholar] [Crossref]
- H S Kim, S W Kim, S M Lee, H Shin. Endoscopic discectomy for the cauda equina syndrome during third trimester of pregnancy. J Korean Neurosurg Soc 2007. [Google Scholar] [Crossref]
How to Cite This Article
Vancouver
Bharti RK. Surgery for Lumbar disc prolapse in pregnancy: Case series [Internet]. IP Indian J Neurosci. 2022 [cited 2025 Sep 13];8(3):217-221. Available from: https://doi.org/10.18231/j.ijn.2022.044
APA
Bharti, R. K. (2022). Surgery for Lumbar disc prolapse in pregnancy: Case series. IP Indian J Neurosci, 8(3), 217-221. https://doi.org/10.18231/j.ijn.2022.044
MLA
Bharti, Rajesh Kumar. "Surgery for Lumbar disc prolapse in pregnancy: Case series." IP Indian J Neurosci, vol. 8, no. 3, 2022, pp. 217-221. https://doi.org/10.18231/j.ijn.2022.044
Chicago
Bharti, R. K.. "Surgery for Lumbar disc prolapse in pregnancy: Case series." IP Indian J Neurosci 8, no. 3 (2022): 217-221. https://doi.org/10.18231/j.ijn.2022.044
