Introduction
Meningioma was named by Harvey Cushing which was theorized to have arisen from the arachnoid cap cells of the leptomeninges. He deducted thatlocation of meningioma was not limited to any anatomicalsite, but was distributed wherever there was leptomeninges un like acoustic tumours.1 Meningiomas are the most common primary benign intracranial neoplasm of the adults. It accounts for 13.0% -36.0 % of all primary central nervous system neoplasms. Only about 1.0 to 3.0 % of all the meningiomas are malignant, however they represent approximately 80.0% of the malignant brain tumour diagnosis.2
WHO in 2007 had divided meningiomas into 3 grades namely WHO grade I, grade II and grade III tumours. Nine histological subtypes meningothelial, fibroblastic, transitional, psammomatous, angiomatous, microcystic, secretory, lymphoplasmacytic-rich and metaplastic meningiomas were classified as Grade I in the WHO 2007 classification. Chordoid, clear cell, and atypical meningiomas were classified as Grade II, while papillary, rhabdoid and anaplastic meningiomas were designated as Grade III.3, 4 In the 2021 updates however, Meningioma has been grouped under a single type.
There are several risk factors which predisposes to the genesis of meningioma. Some of the important risk factors are obesity, alcoholism, previous exposure to ionizing radiation and hormonal replacement therapy. Some genetic conditions like neurofibromatosis type 2, von Hippel Lindau disease, multiple endocrine neoplasia type 1, Li-Fraumeni, Cowden disease, and Gorlin’s syndrome have shown a preponderance towards the development of meningiomas.5, 6 Here in we present a case series of four variable presentations of meningiomas which was received in our institution.
Case 1
A 35 year old female presented to the neurosurgery clinic with insidious onset headache but was persistent and not relieved by medications. She had a history of two live births, with last childbirth 2 years ago. She was hypertensivebut non diabetic and was on oral contraceptive pills
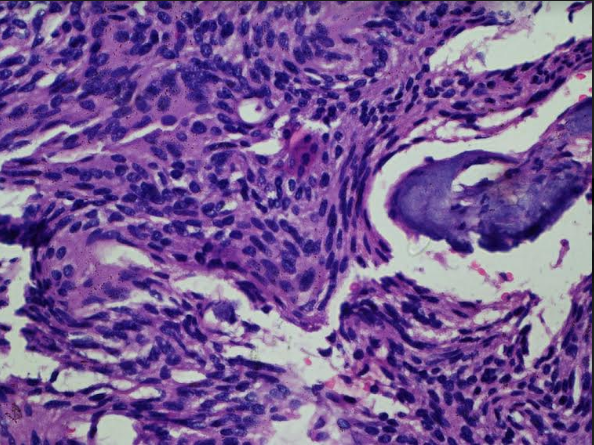
On examination, central nervous system along with other systems showed no abnormality. Routine haematological and biochemical parameters were within normal limits. X-ray chest revealed no abnormality. CT scan revealed isodense left convexity mass in left fronto-parietal region with uniform enhancement suggestive of a meningiomatous lesion (Figure 1). Subsequently craniotomy was performed.
Grossly the resected specimen was creamish, white soft in consistency measuring0.8x0.3 cm in size. Haematoxylin and eosin-stained sections showed lobulararchitecture containing meningothelial whorls formed by syncytial cells with indistinct cell membranes, eosinophilic cytoplasm and round uniform nuclei with intranuclear pseudo inclusions. A report of Meningothelial meningioma was signed out (Figure 2). On follow up after 6 months, the patient was found to be recovering well.
Case 2
A 55-year-old female presented with pain in the limbs to the orthopaedicsclinic associated with weakness. Pain was dull aching with progressive weakness. The patient was normotensive and non-diabetic.
On neurological examination bilateral power was 3/5. Tone was within normal limit. Routine haematological and biochemical tests revealed no abnormality. Routine dorso-lumbar X- ray showed no abnormality.
MRI spine revealed a round extramedullary intradural mass at T7 level which was relatively hyperintense to spinal cord on sagittal sections view with intense post- contrast enhancement, with a provisional diagnosis of midthoracic meningioma (Figure 3).
She was referred to the neurosurgery clinics for further follow up. Subsequently laminectomy with midline dural opening and dissection was performed. There was an immediate resolution of symptoms.
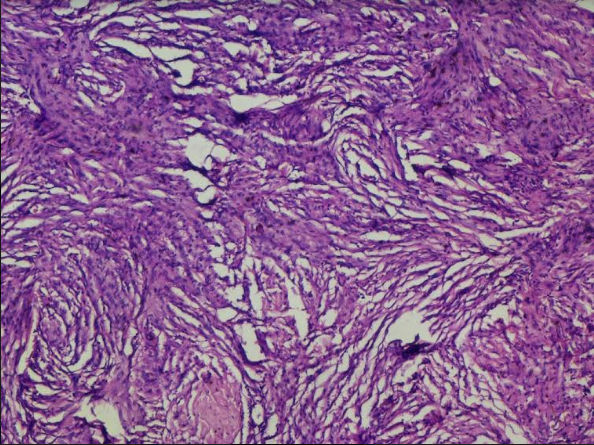
Grossly the resected specimen was multiple, whitish, glistening soft tissue pieces measuring 1.3x0.9 cmin size. Haematoxylin and eosin-stained sections showed whorls of round to oval tumor cells with numerous psammoma bodies obscuring the background with foci of calcification. Few areas of fibrocollagenous tissue with dilated and congested blood vessels and mixed inflammatory infiltrate were seen. Immunohistochemistry of Somatostatin receptor 2a showed variable intensity of cytoplasmic staining; CEA was strongly positive while GFAP was negative. A report of Psammomatous meningioma was signed out (Figure 4). The patient recovered fully with postoperative physiotherapy. On follow up after six months, the patient reported resolution of pain in the limbs and has clinically improved.
Case 3
A 32 year old female presented to the Surgery clinics with dizziness and headache, which was insidious in onset and slowly progressive and not responding to medications. No abnormality of the central nervous system was seen on examination. Patient was normotensive and non-diabetic.
Contrast enhanced MRI showed an ovoid enhancing mass involving left parieto-occipital region with adjacent dural thickening with a provisional diagnosis of meningioma. Craniotomy was performed and grossly the specimen was multiple, fragmented whitish tissue pieces measuring 0.5x0.4 cm. Haematoxylin and eosin-stained sections showed meningothelial cells forming prominent whorls, psammoma bodies and clusters of spindle cells. Few dilated and congested vessels were seen in the background. Immunohistochemistry of Somatostatin receptor 2a showed variable intensity of cytoplasmic staining, while GFAP was negative. A diagnosis of Transitional meningioma was given. There was a resolution of symptoms with patient showing no signs of recurrence on 6 months of follow up.
Case 4
A 40-year-old female presented to the ophthalmic clinic with complaints of diplopia and disturbances in gait. No other complaints were seen. There was a history of oral contraceptive pills intake. Fundus examination revealed disc oedema and mild retinal vessel narrowing. Neurological system revealed no abnormality. Haematological examination revealed mild anemia with lymphopenia. MRI revealed a large ovoid extra axial mass with flat base on dural surface with isointensity on T1WI and contrast enhancement. A provisional diagnosis of meningioma was made. A craniotomy was performed.
Grossly the resected specimen was multiple fragmented soft tissue pieces measuring 1.2x0.6 cm. Haematoxylin and eosin-stained sections showed intracellular lumina with eosinophilic, secretions with areas of meningothelial whorls. Abundant mast cells were seen in the background along with dilated and congested blood vessels.
Secretions were PAS positive and CEA positive. Immunohistochemistry of Somatostatin receptor 2a showed variable intensity of cytoplasmic staining, while GFAP and SOX 10 was negative. A diagnosis of secretory meningioma was signed out. Follow up scans at 6 months showed no residual tumour.
Figure 1
CT scan revealed isodense left convexity mass in left fronto-parietal region with uniform enhancement suggestive of a meningiomatous lesion.
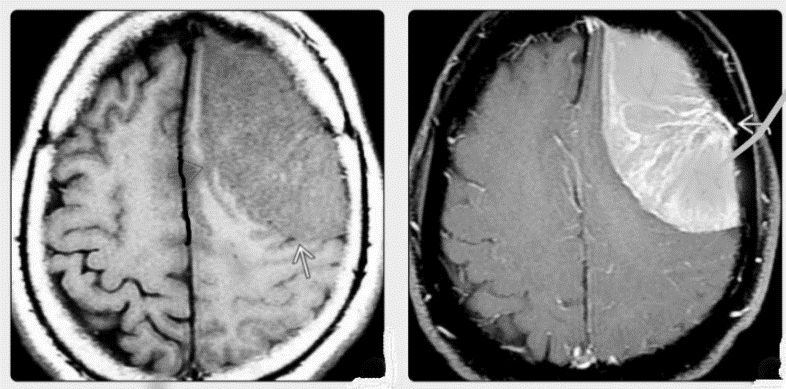
Figure 2
Meningothelial meningioma: Sections showed lobular architecture containing meningothelial whorls formed by syncytial cells with indistinct cell membranes, eosinophilic cytoplasm and round uniform nuclei with intra-nuclear pseudo inclusions. Haematoxylin and eosin x10X.
Discussion
Meningiomas are slow growing mostly benign tumours. They show a female preponderance in the benign category. However, there is male preponderance in the malignant category. 7 The most common site of meningioma is cerebral convexity followed by parasagittal, sphenoid wing, infratentorial, interventricular, tuberculum sella and other sites. 8
Clinical presentation of meningiomas, depends upon their location within the CNS and spinal cord. Symptoms of headache due to increased intracranial pressure, focal neurological deficits or generalized and partial seizures caused by focal mass effect are manifested. Gait disturbances may be seen. Personality changes are associated with parasagittal or frontal meningiomas, which may be diagnosed as dementia. In our case series, we saw varied presentations like headache, dizziness to pain in the limbs with weakness of both limbs, diplopia and gait disturbances. All the above symptoms can occur in cases of meningiomas, depending on their anatomic locations.9, 10
The diagnosis of meningiomas is based on the clinical history, physical examination, radiology and ultimately histologic findings. In CT scans meningiomas may show calcifications and hyperostosis. In contrast enhanced CTscans most meningiomas appear as homogenous dense enhanced dural based lesions with or without brain edema. 11 However, the gold standard for diagnosing meningioma is Magnetic Resonance Imaging butthe definitive diagnosis is done by histopathology. Meningiomas on MR scans appear as lobular, extra axial masses with well-circumscribed margins having a broad-based dural attachment and may displace the cortical grey matter if they are large.
The most common histological type of meningioma is the meningoepitheliomatous type. Histomorphology shows meningothelial cells with round to oval nuclei and indistinct cell borders arranged in sheets or whorls accompanied by psammoma bodies which are extra axial and dural based lesions.12 These fibroblast-like spindle cell tumours predominantly form storiform growth patterns. Variable but often prominent collagen deposition is seen in fibroblastic meningioma. A close differential may be schwanomma but for occasional whorls and psammoma bodies. Transitional meningioma consists of meningothelial and fibrous component and cells with intermediate features. Psamommatous meningiomas are manifest commonly in the spinal cord of older women, where they are usually slow growing and biologically indolent. They show marked calcifications that are readily evident on CT scans. Psammoma bodies constitute over half of the tumour mass. 13 Secretory meningiomas manifests as an advanced form of epithelial differentiation characterized by the formation of gland-like lumens with eosinophilic secretions which are PAS positive, with a female preponderance. The tumor cells associated with the gland-like spaces are usually strongly immunoreactive for cytokeratin. Carcinoembryonic antigen (CEA) is found within the pseudo-psammoma bodies and/or the tumor cells surrounding them. Psamommatous meningioma are also associated with combined KLF4 K409Q and TRAF7 gene mutations. 14, 15
Treatment options include observation for small asymptomatic meningiomas. For large symptomatic meningiomas surgery is indicated. There is a 90.0% chance of disease-free survival.Other treatment options include external beam radiotherapy and neoadjuvant chemotherapy. 16 Our cases did not receive adjuvant or neo adjuvant chemotherapy, as all were of WHO grade I. WHO Grade II and Grade III meningiomas require a multidisciplinary approach involving surgical, medical and oncologic management.17 Craniotomy remains the surgery of choice, however endoscopic approach may be planned if the sinuses are involved. 18