- Visibility 264 Views
- Downloads 40 Downloads
- Permissions
- DOI 10.18231/j.ijn.2022.041
-
CrossMark
- Citation
A rare presentation of neurosarcoidosis as the superior orbital fissure syndrome
Abstract
We are reporting a rare case of neurosarcoidosis that presented with superior orbital fissure syndrome. A 51-year-old Indian woman who suffered from 2 weeks duration, insidious onset gradually progressive left sided headache limited to forehead, left periorbital pain, diplopia on looking toward left, and numbness on the left forehead was referred to our hospital. Ophthalmic findings included left oculomotor nerve, trochlear nerve and abducens nerve palsies, absent corneal reflex, and loss of touch, pain and temperature sensation in V1 distribution. Brain and orbit magnetic resonance imaging (MRI) showed contrast enhancing area at the left orbital apex with normal optic nerve. Normal CSF analysis. High ESR, and chest x-ray showing non-homogenous patchy opacities in bilateral lung fields leaded us for neoplastic screening. Chest computed tomography (CT) revealed multiple ill-defined irregular lung parenchymal nodular opacities of varying sizes involving bilateral lungs with enlarged mediastinal and bilateral axillary lymph nodes. Elevated angiotensin converting enzyme level was found. Biopsy of the axillary lymph node showed non-caseating granulomatous lymphadenitis with giant cells containing schaumann bodies and asteroid bodies in the cytoplasm. These findings indicating an inflammatory response induced by sarcoidosis. After the initiation of steroid treatment, the patient experienced complete remission without any recurrence. When examining a case presenting with superior orbital fissure syndrome with contrast enhancing MRI lesion at the orbital apex, the additional chest CT to exclude neoplastic lesions can detect pulmonary sarcoidosis and extraneural lesions. These may avoid delays in the diagnosis and management of neurosarcoidosis.
Introduction
Sarcoidosis is a chronic granulomatous disease affecting multiple organ systems like, the lungs, heart, nerves, and eyes. Neurosarcoidosis occurs in 5% of patients with sarcoidosis and may impair both the central and the peripheral nervous system.[1], [2] Although the facial nerve is the nerve most commonly involved in neurosarcoidosis, the cranial nerves related to eye movement, including the oculomotor, trochlear, and abducent nerves, are involved in only 2%–7% of cases.[3], [4] The term superior orbital fissure syndrome (SOFS) or Rochon– Duvigneaud syndrome is applied to lesions located immediately anterior to the orbital apex, including the structures exiting the annulus of Zinn and often those external to the annulus. [5] Multiple cranial nerve palsies may be seen including oculomotor nerve (III), trochlear nerve (IV), abducens nerve (VI) and ophthalmic branch of the trigeminal nerve (V1) in the absence of optic nerve pathology. [5], [6] The following is a case clinically and radiologically consistent with superior orbital fissure syndrome that, after comprehensive medical evaluation, was the initial presentation of sarcoidosis.
Case Report
A 51-year-old woman, working in coir factory, with a history of hypertension presented with insidious onset gradually progressive left sided headache limited to V1- trigeminal distribution, moderate to severe intensity and persistent, of 2 weeks duration. Six days later she experienced left periorbital pain which was moderate to severe in intensity and persistent. Along with this she also noticed drooping of left upper eyelid and diplopia more on looking toward left side which progressed later to have diplopia in up and down gaze. She also noticed numbness of the forehead in the ophthalmic division of the trigeminal nerve (V1) distribution.
Upon initial examinations there was no decrease in visual acuity (20/200). Left eye was dilated and fixed with absent direct and consensual pupillary reflex, and normal pupil on the right eye. The patient exhibited near complete ptosis of the left upper lid and restricted extra-ocular movements in all directions. Corneal reflex was absent in left eye. Slit-lamp bio-microscopy showed no inflammatory changes in the anterior chambers, and fundus examinations found no vitreous or retinal abnormalities. There was loss of fine as well as crude touch and, pain and temperature sensation over left ophthalmic division (V1) of the trigeminal nerve. Rest of the central and peripheral nervous system examination was unremarkable. On general examination there was significant enlargement of left axillary lymph nodes which were around 2x1 cm in size, non-tender, firm and non-mobile. Other systemic examination was unremarkable.
The routine hemogram showed low haemoglobin (9.5 gm%), normal total count and platelets and high ESR (110 mm). Peripheral smear showed microcytic, hypochromic RBCs, with normal WBCs and adequate platelet with no atypical cells with in smear. Her electrocardiogram was normal and chest x-ray showed non-homogenous patchy opacities in bilateral lung fields. Renal and liver function tests were normal. As the patient clinically had superior orbital fissure syndrome, and MRI (magnetic resonance imaging) of the brain and orbit with contrast revealed contrast enhancing area measuring 8.5 x 7.2 mm at the left orbital apex with normal optic nerve ([Figure 1]). No other significant MRI finding in the orbit and brain. So as the patient had clinically and radiologically tolosa hunt syndrome (THS) like presentation6 (unilateral painful ophthalmoplegia with preservation of optic nerve), we extended our laboratory work up for neoplastic, infective, inflammatory, vasculitic, and endocrine etiology.

Her further laboratory data showed normal vasculitic, collagen disease, and autoimmune workup. IgG4 level were normal (1.61 U/L, normal range: 0.3-2 U/L). Tumour markers (AFP, CEA, CA 19-9, CA-125) were negative for metastatic diseases. Serum protein electrophoresis was unremarkable with no abnormal M band was seen. Thyroid function test was done to look for thyroid ophthalmopathy which was normal. Cerebrospinal fluid analysis showed no atypical cells, no elevation of pressure, no evidence of CNS tuberculosis, or no other infectious changes. Serum calcium was 8.9 mg/dl. Mantoux test was positive. Serum angiotensin converting enzyme (ACE) levels were high (86 U/L, normal range: 8-52 U/L). Also to screen for primary malignancy in abdomen ultrasonography was done which was unremarkable. Similarly CT scan of the thorax with the contrast was done to look for primary malignancy of the lung which showed multiple ill-defined irregular lung parenchymal nodular opacities of varying sizes involving bilateral lungs with enlarged mediastinal and bilateral axillary lymph nodes ([Figure 2]).

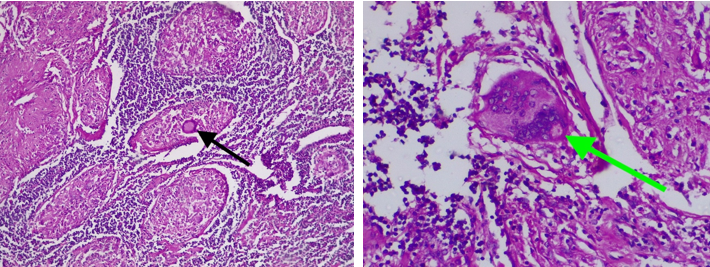
At this point, as the patient had enlarged axillary lymph node, high ACE level and contrast enhanced CT scan of chest showing mediastinal, axillary lymph nodes and lung parenchymal nodular opacities suggestive of sarcoidosis, we decided to do excision biopsy from left axillary lymph nodes which were relatively large and also more accessible for surgical excision. Histopathological findings showed non-caseating granulomatous lymphadenitis with giant cells showing schaumann bodies and asteroid bodies in the cytoplasm, indicating an inflammation response induced by sarcoidosis ([Figure 3]a,b). The patient was diagnosed with probable neurosarcoidosis according to the diagnostic criteria for this condition. [7]
Patient was given parenteral steroid [methyl prednisolone (1 gm/day)] during hospital stay when there was deterioration of ophthalmoplegia and she had good response to that in the form of improvement of ptosis and also diplopia. Then she was started on oral prednisolone 1 mg/kg/day with plan to taper minimum effective dose to reduce side effects. Two months after the initiation of this steroid therapy, the patient’s painful ophthalmoplegia and sensory disturbance in forehead had completely disappeared. There had been no recurrence by 4 months after the initiation of the steroid therapy.
Discussion
Five percentages of patients with sarcoidosis have features suggestive of neurosarcoidosis and may impair both the central and the peripheral nervous system. [1], [2] The facial nerve palsy is the most common cranial nerve palsy caused by neurosarcoidosis. [3], [4], [8], [9], [10], [11], [12] The optic nerve appears to be the second most commonly involved cranial nerve by neurosarcoidosis. [8], [9], [10] Other cranial nerves are very rarely involved in neurosarcoidosis.
A case report by Rose et al., 32-year-old woman with facial and vestibulocochlear nerve palsies. She was definitely diagnosed with neurosarcoidosis based on pathological findings of the biopsy of supraclavicular lymph node. Consistent with our case, imaging findings of the chest X-ray and CT were valuable markers for its diagnosis. [10] Miyajlovic et al. reported a case of 70-year-old woman with multiple cranial neuropathies. This case had an eye movement disturbance associated with oculomotor and trochlear nerve palsies partially like that in our case. [11] Consequently, elevations of ACE level in the serum and CSF were conclusive findings without undergoing biopsy. Erer-Ozbek et al. documented a 36-year-old woman with oculomotor, facial, glossopharyngeal, and accessory cranial nerve palsies. [12] In this case, a biopsy of hilar lymph nodes revealed a non-caseating granuloma even without increased serum ACE level. All these cases were treated with prednisolone, which improved their symptoms. [10], [11], [12] Almost similar to our case, Brandy et al. presented a 55-year-old women with oculomotor, abducent and ophthalmic division of the trigeminal nerve (V1) involvement. MRI showed involvement of extraocular muscles with intracranial extension and cavernous sinus. She was definitely diagnosed by endonasal cavernous sinus endoscopic biopsy showing non-necrotising granuloma suggestive of sarcoidosis after CT thorax showed evidence of bilateral hilar and well defined lung lymph nodes. [13]
In our patient, clinical history and the orbital MRI findings suggested THS. After systemic examination, laboratory findings, CT scan thorax, and biopsy, we considered an unusual initial presentation of systemic sarcoidosis with major neurological symptoms. Isolated neurosarcoidosis is rare, since over 90% of patients also have sarcoidosis in other organs, especially the lungs and mediastinal lymph nodes. [14] Cranial neuropathy is the most common manifestation of neurosarcoidosis. [6] Diagnosing neurosarcoidosis is often difficult, because the clinical manifestations and findings of imaging studies can be mimicked by several other diseases. Brain MRI is the most sensitive diagnostic imaging test. [14] This case highlights that sarcoidosis can present in unusual ways, masking neurological disorders.
As per the aforementioned previous case reports, multiple cranial nerve palsies involving eye movements is a rare clinical manifestation in the case of neurosarcoidosis, and the present case is extremely rare as it presents with superior orbital fissure syndrome which is reported in only one case report according to best of our knowledge. Moreover, the only critical finding that motivated us to make a diagnosis of neurosarcoidosis was the incidentally discovered right hilar lymphadenopathy on chest CT, which was originally performed to examine tumorous lesions. In consideration of such atypical ophthalmic manifestation and difficulty of diagnosis, the present case is considered to be worth as a novel case report of atypical neurosarcoidosis.
In conclusion, when examining a case presenting with superior orbital fissure syndrome/ tolosa hunt syndrome with contrast enhancing MRI lesion in the orbit, the additional chest CT to exclude neoplastic lesions can detect pulmonary sarcoidosis and extraneural lesions. These may avoid delays in the diagnosis and management of neurosarcoidosis.
Patient Consent
The patient’s legal guardian orally consented to the publication of this case report.
Source of Funding
No funding or grant support.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
References
- Lacomis D. Neurosarcoidosis. Curr Neuropharmacol. 2011;9(3):429-36. [Google Scholar] [Crossref]
- Tana C, Wegener S, Borys E, Pambuccian S, Tchernev G, Tana M. Challenges in the diagnosis and treatment of neurosarcoidosis. Ann Med. 2015;47(7):576-91. [Google Scholar] [Crossref]
- Fritz D, Beek DVD, Brouwer M. Clinical features, treatment and outcome in neurosarcoidosis: systematic review and meta-analysis. BMC Neurol. 2016;16(1). [Google Scholar] [Crossref]
- Ohno T, Ishihara M, Shibuya E, NM. Sarcoid uveitis in a patient with multiple neurological lesions: a case report and review of the literature. J Med Case Rep. 2018;12(1). [Google Scholar] [Crossref]
- Kline L. The Tolosa-Hunt syndrome. Surv Ophthalmol. 1982;27(2):79-95. [Google Scholar] [Crossref]
- Prete B, Sowka J. Painful ophthalmoplegia as aninitial presentation of sarcoidosis. Clin Exp Optom. 2017;100(3):291-4. [Google Scholar] [Crossref]
- Jain R, Yadav D, Puranik N, RG, Jin J. Sarcoidosis: causes, diagnosis, clinical features, and treatments. J Clin Med. 2020;9(4). [Google Scholar] [Crossref]
- Tana C, Wegener S, Borys E, SP, Tchernev G, Tana M. Challenges in the diagnosis and treatment of neurosarcoidosis. Ann Med. 2015;47(7):576-91. [Google Scholar] [Crossref]
- Hussam AY, ZA, Nizar S. Cranial neuropathies in sarcoidosis. World J Ophthalmol. 2015;5(1):16-22. [Google Scholar]
- Oliver R, Zahoor A, Barry S. Multiple cranial nerve palsies as the first presentation of sarcoidosis. Case Rep Otolaryngol. 2014. [Google Scholar] [Crossref]
- Mijajlovic M, Mirkovic M, Mihailovic-Vucinic V, Aleksic V, Covickovic-Sternic N. Neurosarcoidosis: two case reports with multiple cranial nerve involvement and review of the literature. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2014;158(4):662-7. [Google Scholar] [Crossref]
- Erer-Ozbek S, Bora I, Yurtogullar S. Acute multiple cranial neuropathy in a patient with neurosarcoidosis. Neurol Sci. 2010;31(6):865-6. [Google Scholar] [Crossref]
- Brandy-García A, Suárez-Cuervo C, Caminal-Montero L. Tolosa-Hunt Syndrome as an Initial Presentation of Sarcoidosis. Reumatol Clin (Engl Ed). 2020;17(3):178-9. [Google Scholar] [Crossref]
- Ungpraset P, Matteson E. Neurosarcoidosis. Rheum Dis Clin North Am. 2017;43(4):593-606. [Google Scholar] [Crossref]
How to Cite This Article
Vancouver
Zadafiya HB, CV S, KA K, SR P. A rare presentation of neurosarcoidosis as the superior orbital fissure syndrome [Internet]. IP Indian J Neurosci. 2022 [cited 2025 Sep 23];8(3):204-207. Available from: https://doi.org/10.18231/j.ijn.2022.041
APA
Zadafiya, H. B., CV, S., KA, K., SR, P. (2022). A rare presentation of neurosarcoidosis as the superior orbital fissure syndrome. IP Indian J Neurosci, 8(3), 204-207. https://doi.org/10.18231/j.ijn.2022.041
MLA
Zadafiya, Hirankumar Babubhai, CV, Shaji, KA, Kabeer, SR, Prasanth. "A rare presentation of neurosarcoidosis as the superior orbital fissure syndrome." IP Indian J Neurosci, vol. 8, no. 3, 2022, pp. 204-207. https://doi.org/10.18231/j.ijn.2022.041
Chicago
Zadafiya, H. B., CV, S., KA, K., SR, P.. "A rare presentation of neurosarcoidosis as the superior orbital fissure syndrome." IP Indian J Neurosci 8, no. 3 (2022): 204-207. https://doi.org/10.18231/j.ijn.2022.041
