Introduction
Moyamoya disease is a uncommon condition characterized by progressive stenosis of internal carotid artery and major arteries of circle of willis and multiple random collaterals at base of brain. The incidence of intracranial aneurysm in MMD is approximately 3.4-18% which is higher than in general population and associated with poor prognosis. The hemorrhagic complications are frequently due to rupture of aneurysm. The pathogenesis of aneurysm is due to multiple interconnected factors like hemodynamic stress, pathological vessel architecture, and the site at which they occur.
Case Report
A twenty-one years old female, presented to emergency room with history of sudden onset of severe headache, 1 episode of seizure and loss of consciousness. She had no previous similar complains in past or any significant comorbidities. On Examination vitals were stable. She was irritable with neck stiffness, bilateral pupils were reactive to light. She could follow simple verbal commands and move all 4 limbs. Her routine investigations were normal, coagulation profile was normal, peripheral smear showed no evidence of sickle cell disease, serum TSH and blood glucose levels were normal. Serum ANA with immunofloresence test was negative.
Figure 5
Diffusion weighted imageshowing multiple infract in bilateral temporal region, right occipital region and cortical infarcts.
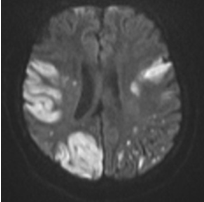
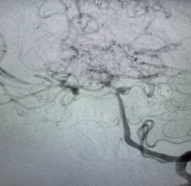
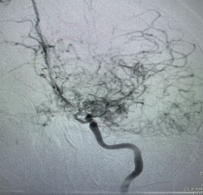
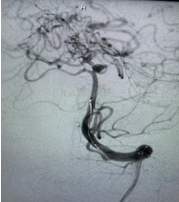
CT scan of brain was done which showed subarachnoid hemorrhage in basal cistern, cerebral Angiography was suggestive of aneurysm of approximately (2*1.5cm) at basilar artery and left Superior cerebellar artery junction. She underwent Digital subtraction angiography of cerebral vessels which was suggestive of basilar artery and left Superior cerebellar artery junction, stenosis of internal carotids artery and multiple collaterals in posterior circulation suggestive of Moyamoya disease(MMD). She underwent endovascular coiling of aneurysm. She was treated with medical management of aneurysm with enteral nimodipine 60mg, adequate hydration and anti epileptic drug; she was also started on Aspirin 150mg once daily to prevent ischemic complication secondary to MMD. On third post operative day she has worsening sensorium with dysarthria, dysphagia, emotional lability and upper limb weakness. MRI brain was done which was suggestive of bilateral insular cortex, right occipital cortex and multiple high parietal cortical infarcts. DSA was done again which showed diffuse vasospasm which was treated with intra arterial nimodipine and milrinone. She was continued on medical management and started on warfarin after adequate discussion with relative regarding risk of hemorrhage. Following this she had uneventful recovery and was discharged with residual bulbar weakness.
Discussion
Moyamoya disease (MMD) is an idiopathic cerebrovascular disease characterized by progressive stenosis or occlusion of the terminal portion of the bilateral internal carotid artery (ICA) and the formation of abnormal collateral networks at the base of the brain.1 Aneurysm associated with Moyamoya disease is rare. Intracranial aneurysms associated with MMD are known to be one source of intracranial hemorrhage. They can occur widely in the intracranial artery, ranging from the circle of Willis at the base of the brain to moyamoya vessels, but most typically they occur within the posterior circulation.
Intracranial aneurysms associated with MMD are usually classified into major artery aneurysms and peripheral aneurysms according to the location. The major artery aneurysms are typically true saccular aneurysms, predominantly at the circle of Willis. The peripheral aneurysms occur mainly in or near the fine collateral network of moyamoya vessels; they are commonly pseudoaneurysms resulting from rupture of the pathological moyamoya vessels or distal dilated choroidal arteries. Ni et al.2
reported that 47.2% of 36 aneurysms associated with MMD were peripheral aneurysms and 52.8% were major artery aneurysms.
Zhao et al3 reported the major artery aneurysms (78.6%) were much more than the peripheral aneurysms (21.4%).The major artery aneurysms in anterior circulation are common in the Anterior communicating artery(ACoA), posterior communicating artery (PCoA) and Anterior choroidal artery (AChA), and those in posterior circulation are common in the basilar artery tip and Posterior Cerebral Artery. The peripheral aneurysms often occur in the distal AChA, PChA, lenticulostriate artery and moyamoya vessels.
Zhang et al 4 further categorized these aneurysm according to site of aneurysm.
Major artery aneurysm which can be anterior or posterior circulation.
Peripheral artery aneurysm futher classified as anterior choridalor posterior choridal artery
Moyamoya vessel aneurysm
Meningeal artery aneurysm
Aneurysm at the site of anastomosis
The basilar artery is susceptible to develop aneurysms due to increased hemodynamic stress on the vessel wall. Aneurysms are frequently found in the tip of the basilar artery, including those associated with MMD. Because basilar tip aneurysms are deeply located, direct clipping is difficult and dangerous. Endovascular embolization is the main treatment option for these aneurysms. The direct clipping is difficult and hazardous, because first, it carries a risk of disrupting important collateral vessels. Second, intraoperative brain retraction should be minimized because cerebral tolerance to ischemia is poor in these patients. Third, temporary interruption of the parent arteries may also cause irreversible cerebral infarction. Thus, endovascular coiling is preferred over surgical clipping. In addition, perioperative hypercapnia, hypocapnia, hypotension, and hypovolemia may also lead to cerebral ischemia.
Table 1
Summary of cases with basilar artery aneurysm with Moyamoya disease
|
Author |
Number of cases |
Presentation |
Treatment |
Outcome |
|
Dange et al.,2018 5 |
4 |
4-Ruptured SAH |
Endovascular treatment |
No complications |
|
Wan et al., 2015 6 |
4 |
1 each SAH, IVH, ICH+SAH, Ischaemia |
Endovascular Coiling with/without revascularisation |
No complications |
|
Jeon et al.,2014 7 |
2 |
1-ruptured, 1 unruptured aneurysm |
Y stent coiling |
Thromboembolic infarction due to acute in-stent thrombosis; postoperative Infarction in the midbrain. |
|
Kim et al.,2012 8 |
1 |
SAH |
Endocasvular embolization |
No complications |
|
Yu et al.,2010 9 |
1 |
SAH |
Endovasular embolization |
No complications |
|
Artia et al.,2003 10 |
5 |
Subarachnoid hemorrhage (3); cerebral hemorrhage (1); asymptomatic (1) |
Endocasvular embolization |
One case with transient intraoperative mydriasis; 1 case with transient oculomotor paresis; 3 cases no complications. |
|
Kagawa et al. (2001) 11 |
1 |
Left hemiparesis |
Endocasvular embolization |
No complications |
|
Irie et al. (2000) 12 |
1 |
SAH |
Endocasvular embolization |
No complications |
|
Bhattacharjee et al. (1999) 13 |
1 |
SAH |
Direct clipping |
Brain death |
MMD is a disease outcome of enhanced angiogenesis. When vessels are occluded, collateral circulation develops to stabilize cerebral blood flow, but the collateral vessels in MMD may be small, weak, and prone to hemorrhage/aneurysm and thrombosis. Collateral vessels of MMD, the moyamoya vessels, are dilated perforating arteries that have various histopathologic changes, including fibrin deposits in the wall, fragmented elastic laminae, attenuated media, and the formation of microaneurysms. Thus, aberrant collaterals could be the source of thromboembolism occluding distal branches of collateral flows. Ischemic cerebrovascular events in patients with MMD were attributed to reduced blood flow caused by obstruction of major intracranial arteries. Embolic phenomenon is also a predominant mechanism of brain infarction in MMD. Yamashita et al14 evaluated histopathologic changes of moyamoya vessels in 22 patients with MMD and showed intraluminal thrombosis in the stenotic segment and microaneurysm formation or attenuation of vessel thickness.
Kim et al15 suggested that ischemia following moyamoya disease most of the diffusion restriction patterns (83.7%) were of embolic type, and hemodynamic pattern was rarely observed in the acute symptomatic patients with MMD, microembolic signals could be observed in approximately a third of patients (31.6%) in transcranial Doppler monitoring; and most hemispheres (86%) showed good collateral status, and few patients with acute infarcts of embolic pattern showed poor collateral status. Thus ischemic stroke is more likely to be because of thromboembolism than to collateral failure. Caplan et al 16 described that hypoperfusion and embolism often coexist in the mechanism of infarction, and the interrelationship involves 2 factors: decreased perfusion limiting blood flow to regions rendered ischemic by emboli and decreased blood flow impeding washout of the emboli.
Cerebral vasospasm remains a leading cause of disability after aneurismal subarachnoid hemorrhage (SAH). Rates of cerebral infarction caused by vasospasm range between 24- 35% on computed tomography (CT) scan and may be 81% when magnetic resonance imaging (MRI). Vasospasm is most often a multivascular or diffuse process. Rabeistein et al 17 showed that 2 common patterns of cerebral infarction from delayed cerebral ischemia: single cortical infarction typically in the proximity of the ruptured aneurysm and multiple widespread lesions often involving subcortical regions and frequently distant from the site of aneurysm rupture. Hijdra et al 18 found 60% of cases to have multivascular and diffuse ischemia.
Iwama et al.,19 described three patient with bleeding type moyamoya disease who suffered ischemic complication following first episode of intracranial hemorrhage. Dehydration accelerated by administration of hyperosmotic drug was suggested as contributory factor. Shibamoto et al.,20 described a case of right unilateral Moyamoya disease with right MCA territory hypoperfusion in a postoperative case of intracranial hemorrhage in a case with Moyamoya disease. Possibility of raised intracranial pressure, dehydration, vasospasm and shrinkage of ruptured vessels was considered in pathogenesis of ischemia. Matsuoka et al.,21 suggested in their case report that diffuse segmental vasoconstriction of basilar and posterior cerebral arteries after intracranial hemorrhage in moyamoya disease.
Thus, to conclude Moyamoya Disease associated with aneurysm is rare and hemorrhagic and ischemic complications are common in Moyamoya disease. Prevention of hypotension by adequate hydration, judicious of hyerosmolar therapy and anticoagulation may help in prevention of ischemic complications.