Introduction
Central nervous system tuberculosis is a devastating disease if not detected and treated at an early stage. It may manifest as tuberculous meningitis, tuberculoma or tuberculous brain abscess. It has multiple varied clinical presentations like - meningitis symptoms [fever, headache, neck stiffness, vomiting], focal neurological deficits, altered sensorium [encephalopathy], lethargy with decreased concentration, seizures and multiple cranial nerve palsies. 1 Here we describe a case of a 49-year-old retroviral positive male, presenting with excessive daytime sleepiness for two weeks. He was diagnosed to have multiple central nervous system tuberculoma and showed improvement in his symptoms after starting on steroids and anti-tuberculous medication.
Case History
A 49-year old male known case of the retroviral disease for five years on antiretroviral therapy since then with good compliance, now presented with acute onset excessive daytime sleepiness with snoring and fatiguability for two weeks. No history of seizures, headache, vomiting, or fever with no associated history of weight loss and loss of appetite. No record of preceding head trauma. He was a smoker for 25 years and restrained alcohol use for 15 years.
Figure 1
Magnetic Resonance Imaging of Brain– Fluid attenuated inversion recovery images; A,B: Showing hyperintensities in the thalamus; A: Triangle head) and mid-brain; B: Triangle head). Diffusion-weighted imaging; C: showing diffusion restriction in medial thalamus (left more than right – arrows) with Apparent diffusion coefficient; D: consistent with acute infarct. T1 weighted post-contrast images; E,F: showing contrast enhancement with conglomerate ring lesions.
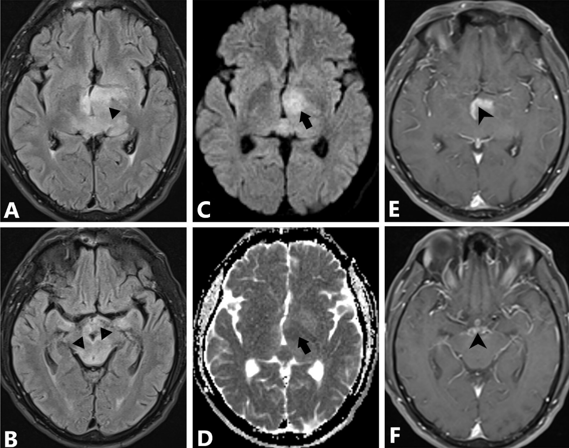
Clinically, he was conscious, alert, moderately built, and well-obeying commands—no focal neurological deficits. Fundus examination was normal, with no evidence of papilledema/ retinopathy. With a clinical scenario of acute onset sleep disturbance, he was evaluated accordingly. Blood investigations – total counts were 12200 per microlitre with normal haemoglobin and platelet counts. His erythrocyte sedimentation rate was 24 mm after two hours. Renal and liver functions were normal. Chest x-ray showed no abnormality. Magnetic resonance imaging (MRI) of the brain showed hyperintensities in the bilateral thalamus and midbrain (Figure 1A,B) with a tiny vasculitic infarct in the left thalamus (Figure 1C,D). Post-contrast imaging (Figure 1 E,F) showed multiple conglomerate ring-enhancing lesions with oedema in the bilateral thalamus, interpeduncular cisterns, pons, cerebellar vermis and the left ganglio-capsular region. Spectroscopy showed lactate peak – features were suggestive of tuberculoma. Spine screening showed no evidence of any space-occupying lesions.
The cerebrospinal fluid analysis showed five cells with elevated protein (66.2g/dl) and normal glucose levels (50.5mg/dl).
Considering his acute-onset excessive daytime sleepiness (EDS) secondary to tuberculoma, he was started on anti-tuberculous medication with steroids. His sensorium improved after starting on medication. Pulmonologist had seen him during the hospital stay for sleep apnoea - His body mass index was 24.7. Polysomnography (PSG) testing was done. It showed central and obstructive apnoea evidence with the former being predominant [Apnoea –hypopnoea index (AHI) of 58.7 with poor effort on spirometry]. He was advised on home CPAP with inhalers at discharge. After three months, his EDS improved, and his CPAP titration study showed improvement in the AHI index (value of less than 5).
Discussion
Excessive daytime sleepiness or hypersomnia as an acute and primary presentation is uncommon and less evident. In a clinical setting, hypersomnia can be pulmonary, cardiac, neurological or psychiatry related.2 Sleep-related disorders like sleep-disordered breathing and sleep-wake disturbances are known to be reported in neurological conditions like stroke. Sleep-disordered breathing like central sleep apnoea, obstructive sleep apnoea, and complex sleep apnoea occurs in neuromuscular junction disorders and degenerative disorders (multiple systemic atrophy, Parkinson's disease) and epilepsy. Sleep-wake disturbances like excessive daytime sleepiness (EDS or hypersomnia or sleep attacks), insomnia and sleep-related movement disorders like REM sleep behaviour disorder are known to occur in neurological conditions.3 All these are known to occur as subacute to chronic, except for stroke and trauma. These disorders cause decreased concentration, fatiguability, low productivity and increase the risk of injury and accidents. Apart from that, it also causes heightened psychosocial stress with family, friends and work.
Physiologically, sleep is modulated by sleep-promoting and wake-promoting thalamocortical circuits. The brainstem controls respiration. Regions like the insular cortex, supplementary motor cortex and thalamus also play a role in autonomic and voluntary breathing.4 Hypothalamus also helps in the regulation of respiration during sleep.5 Neurological conditions causing acute sleep-related disturbances include stroke. 6, 7 epilepsy, head trauma8 and metabolic encephalopathy. Vascular insults to the ventral thalamus and hypothalamus are known to cause hypersomnia.9, 10 A case report of the artery of Percheron infarct, presenting with excessive daytime sleepiness, has been reported.11 In thalamic strokes with EDS, bilateral or left side lesions have poorer recovery than right-sided lesions with less common cognitive deficits and complete recovery.7
A case presenting with excessive daytime sleepiness (EDS) was indicative of initial presentation secondary to tuberculoma in the bilateral thalamic region and had a better outcome despite bilateral involvement. We highlight this as the first case report of central nervous system tuberculoma presenting acutely as excessive daytime sleepiness.
Conclusion
Acute onset hypersomnia with sleep apnoea occurring secondary to thalamic tuberculoma has been less reported. Apart from vascular events and metabolic conditions, we should also consider infections as an etiological association with acute onset sleep-related disorders. They have a detrimental effect and may lead to mortality if there is any delay in the diagnosis. Early detection and initiation of treatment measures can improve quality of life.
