- Visibility 327 Views
- Downloads 51 Downloads
- Permissions
- DOI 10.18231/j.ijn.2022.010
-
CrossMark
- Citation
A study of compliance and insight in patients with schizophrenia
Abstract
Introduction: Schizophrenia is a major psychiatric disorder with prevalence of 1%. The long course of illness warrants strict compliance to antipsychotic medications which is a common challenge faced by the treating psychiatrist and it affects the quality of life of the patient and the caregiver. This study aims to understand the complex relationship between insight of having the illness and compliance to medications.
Aim: To study the relationship between insight and medication compliance in schizophrenia.
Materials and Methods: This cross-sectional study included 50 patients diagnosed with schizophrenia, attending the psychiatry OPD or admitted in psychiatry ward who fulfilled the inclusion criteria. After taking the informed consent, the compliance and patients’ attitude towards illness and medication was assessed using Adherence to medication regimen. Insight was assessed using Scale to Assess Unawareness of Mental Disorder.
Results: A total of 21 patients (42%) were fully compliant to their treatment, whereas more than half of patients had full insight into their illness (n=30, 60%). Lack of insight correlated with poor compliance. Patients with poor compliance were also less aware of the beneficial effects of the treatment. There was also a statistically significant relationship between insight, compliance and patients’ belief that medications help in keeping them in good mental health.
Conclusion: Patients with better understanding of nature of illness and symptoms were more compliant with medications. This reinforces the role of insight facilitation along with psychoeducation of family members regarding compliance in the treatment of schizophrenia. Further exploration of patients’ and relatives' concept of illness and the treatment are needed to develop interventions to improve compliance.
Introduction
Every aspect of a patient’s life is affected by schizophrenia. Non-compliance is the biggest challenge faced during the long-term pharmacotherapy in schizophrenia.Compliance refers to the extent to which a person’s behaviour coincides with medical or health advice. It includes errors of omission, mistakes in dosage and timing, and taking medications that are not prescribed.[1] While non-compliance is common in many medical conditions, poor treatment adherence can have disastrous consequences in the life of a patient with schizophrenia and also the family members. 25% to 70% of all schizophrenic patients are noncompliant, despite estimated rates of noncompliance differing because of inconsistent definitions and heterogeneous samples.[2] This maybe because majority of schizophrenics believe they are not ill or they attribute illness to external factors. This has an important effect on compliance. Rapport between the doctor and patient and the subjective well-being of the patients on treatment are the two agreed-upon major determinants for medication compliance.[3]
One of the most intriguing aspects of dealing with patients of schizophrenia is phenomenon of insight. Traditionally, insight has been used to differentiate between two broad groups of disorders, the psychoses and the neuroses. However, current views are slightly different and insight may be seen in psychotic disorders.
Grades of insight ranging from complete denial to true emotional insight have been suggested. These grades include
Complete denial of illness
Slight awareness of being sick and needing help but denying it at the same time.
Awareness of being sick but blaming it on others, external factors, or medical or unknown organic factors.
Intellectual insight: Admission of illness and recognition that symptoms or failures in social adjustment are due to irrational feelings or disturbances, without applying that knowledge to future experiences.
True emotional insight: Emotional awareness of the motives and feelings within and of the underlying meaning of symptoms, whether the awareness leads to changes in personality, and future behavior; openness to new ideas and concepts about self and important people in the person’s life. [4]
Patient not believing that they are ill or accept that they experience clinical symptoms can lead to therapeutic noncompliance. Result of studies of insight in patients with schizophrenia suggests that decreased insight is associated with greater risk of relapse, impaired social functioning and non-compliance with medication and treatment. [2] In schizophrenia, positive symptoms may distort insight, negative symptoms reduce the will and drive, cognitive deficits affect attention and memory.
The patient's perspective has been a neglected area of research over a long period. Recently, the development of second-generation anti psychotics, with their improved side-effect profile, has enabled the focus of treatment to be broadened to include the patient's overall well-being and quality of life. Moreover, in the past, clinicians did not trust the patient’s report on their subjective well being. On the contrary, a growing number of studies have demonstrated that self-rating scales can be completed in a consistent and reliable manner by most schizophrenic patients, if not acutely psychotic or having severe cognitive impairment.[5], [6], [7], [8] The relationship between insight and treatment compliance is very important because patients will accept treatment on their own if they believe that they are ill. Thus, this relation has great implications from the view of prognosis, outcome of schizophrenia and rehabilitation of patients. Most of the studies on insight and its correlates have been done in the West and Indian studies on this topic are very few. The relationship between insight and compliance need to be studied in Indian population and present study is an attempt to do so.
Materials and Methods
This cross-sectional study was conducted in a tertiary care teaching hospital over a period of 18 months. The clearance from the ethical committee was sought before initiating this time bound study. During this time period and after taking informed consent from the patient, a total of 50 participants who fulfilled the inclusion criteria and exclusion criteria, were selected for the study.
Patients attending the Psychiatry OPD / admitted in psychiatry ward, diagnosed as Schizophrenia (ICD -10 Diagnostic Criteria for Research).
Patients between 18 and 60 years of age.
Patients who were on treatment for at least 3 months.
Exclusion criteria
Presence of any comorbid psychiatric disorder including substance abuse.
Presence of any comorbid physical illness in patient.
Violent and noncooperative patients.
Study tools used
Detailed semi- structured Proforma was prepared to gather information regarding the demographic details of the patients attending Psychiatry OPD which includes name, age, sex, marital status, type of family and residential address.
To assess compliance itself and several factors influencing compliance, a self-reporting compliance interview “Adherence to medication regimen” was used that covers the following issues: patients’ personal and clinical data, type and dose of medication, patients’ attitudes toward their illness in comparison with other serious diseases, and questions regarding who asks the patient about taking medication and about the reasons for failure to take drugs. It includes questions on attitude towards illness, medications and also reaction of relatives and other caregivers on non-compliance. Most questions can be answered by either “yes,” “no,” or “don’t know,” or “more,” “equally,” “less serious,” or “don’t know.” Three questions require a narrative answering. The above scale is being used after taking due permission from the original author Dr. Maria Anna Rettenbacher. [9]
To assess insight, the “Scale to assess Unawareness of Mental Disorder” (SUMD) was used. This scale was developed by Amador and Strauss in 1993. It samples discrete and global aspects of insight across a variety of manifestations of illness. The SUMD is a standardized scale on which ratings are made on the basis of direct patient interview. All scores range from 1 to 5, with higher scores indicating poorer awareness or attribution. [10]
Data was entered in to Microsoft Excel 2007 and analysed using Epi Info 3.4.3. Appropriate descriptive statistical methods were used and Chi-square was used for correlation analysis.
Results
eveals age distribution of the patients included in the study. Majority of the patients (28%) were between the age group of 21-30 years and 41-50 years. The least number of patients (2) were between the ages of 18-20 years.
hows the sex distribution of patients included in the study. 29 out of 50 (58%) patients were females.
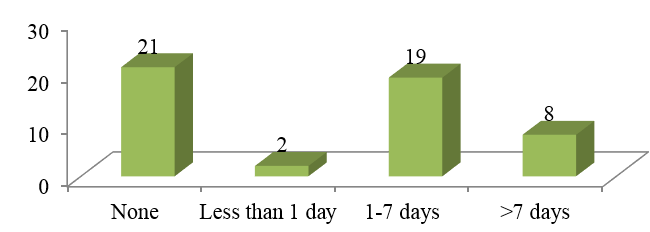
The [Figure 1] and [Table 3] shows compliance rates of the patients. Original author of the questionnaire used to assess compliance (Adherence to medication regimen) classified patients as (1) fully compliant = medication never missed, (2) partially compliant = missed medication for a maximum of 7 consecutive days, and (3) noncompliant = missed medication for more than 7 consecutive days during the last 3 months.21 (42%) of total patients were fully compliant, 21(42%) were partially compliant whereas only 8(16%) were noncompliant.
[Table 4] Shows the no. of patients who believed that there are problems taking medicines for treatment.
There was a highly significant relationship (p=0.0001) between insight and belief that medicines help in keeping patients in good mental health as shown in following [Table 5]. 28 out of 30 patients having full insight believed that medicines keep them in good mental health. Only 2 out of 9 patients with no insight believed the same.
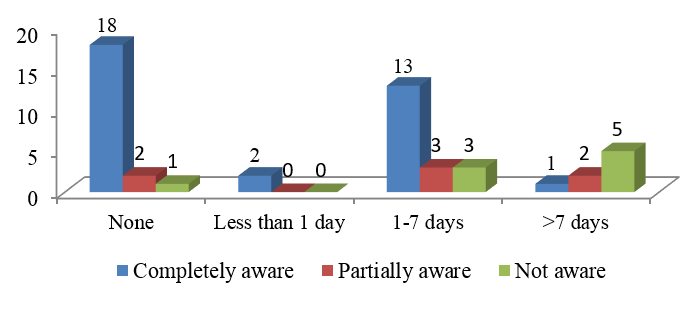
[Table 6] and [Figure 2] shows the relationship between compliance and patients’ belief regarding the beneficial effects of medicines. Similar to above relationship 18 out of 21 fully compliant patients were completely aware of beneficial effects of medicines, and only 1 out of 8 non-compliant patients were aware of the beneficial effects of medicine. Relationship was found to be significant according to chi square analysis (p=0.007).
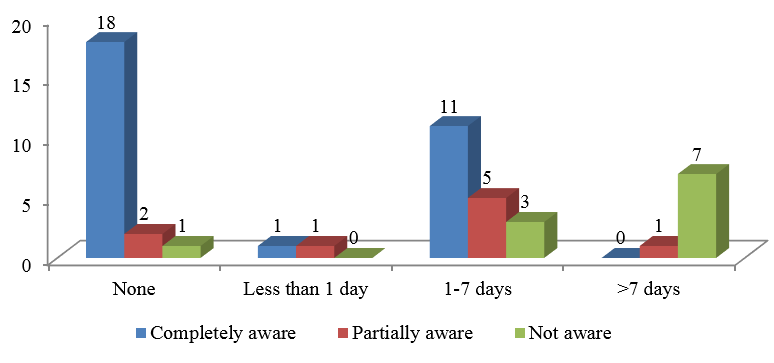
[Table 7] and [Figure 3] shows the relationship between insight and compliance. Relationship between the two was highly significant with p=0.001 according to Chi square test. 18 out of 21 fully compliant patients had complete awareness of their illness. Out of 8 patients who were non-compliant, none of them were completely aware of their illness.
|
Age (In years) |
No. of patients (%) |
|
18-20 |
2(4) |
|
21-30 |
14(28) |
|
31-40 |
11(22) |
|
41-50 |
14(28) |
|
51-60 |
9(18) |
|
Total |
50(100) |
|
Sex |
No. of patients (%) |
|
Male |
21(42) |
|
Female |
29(58) |
|
Total |
50(100) |
|
Days Off Rx in last 3 months |
No. of patients (Percent) |
|
None |
21(42) |
|
Less than 1 day |
2(4) |
|
1-7 days |
19(38) |
|
>7 days |
8(16) |
|
Total |
50(100) |
|
Problems taking medicines |
Frequency (%) |
|
Yes |
35(70) |
|
No |
15(30) |
|
Total |
50(100) |
|
Insight |
Medicines help in keeping you in good mental health |
Total |
||
|
Yes |
No |
Don't know |
||
|
Completely aware |
28 |
1 |
1 |
30 |
|
Partially aware |
7 |
2 |
0 |
9 |
|
Not aware |
2 |
9 |
0 |
11 |
|
Total |
37 |
12 |
1 |
50 |
|
Days off Rx |
Achieved effects of Rx |
Total |
||
|
Completely aware |
Partially aware |
Not aware |
||
|
None |
18 |
2 |
1 |
21 |
|
Less than 1 day |
2 |
0 |
0 |
2 |
|
1-7 days |
13 |
3 |
3 |
19 |
|
>7 days |
1 |
2 |
5 |
8 |
|
Total |
34 |
7 |
9 |
50 |
|
Days Off Rx |
Insight |
Total |
||
|
Completely aware |
Partially aware |
Not aware |
||
|
None |
18 |
2 |
1 |
21 |
|
Less than 1 day |
1 |
1 |
0 |
2 |
|
1-7 days |
11 |
5 |
3 |
19 |
|
>7 days |
0 |
1 |
7 |
8 |
|
Total |
30 |
9 |
11 |
50 |
Discussion
It is believed that antipsychotic maintenance treatment may reduce the severity of symptoms or prevent relapse, so medication compliance has become a focus of increasing concern. The intent of this study was to study compliance, insight and relationship between the two. The cyclical nature of non-compliance in schizophrenia is thought to reflect the patient’s state of mind.
Age
In the study sample, subjects were predominantly between the age group of 21-50 years (78%, n=39) (table 1). This in keeping with other western studies [11] and a large epidemiological Indian study done by Padmavathi [12] in urban Madras that reported that prevalence of schizophrenia was highest in the age range of 15-45 years. Maximum amount of insight and compliance was seen in patients of age group 51-60years (six out of nine, 66.6%).
Gender
Of the fifty patients constituting our study sample, 42% were males (n=21) and 58% were females (n=29) (table 2). This reflected the pattern of patient population coming to the institute. This also could reflect the fact that more females sought treatment or were brought for treatment as compared to males. Most of the studies in western countries [13], [14], [15] and India [16] had more male patients in their study except few. [13] out of 21 (61.9%) males were fully aware of their illness whereas 17 out of 29 (58.6%) females had full insight. More males (52.3%) than females (34.4%) were fully compliant to treatment.
Compliance
In our study, 42% of patients were fully compliant, 42% partially & 16% were non-compliant (table 3). Partially compliant were defined as patients who missed medications for 1 day or more but less than 7 days in last 3 months, whereas non-compliant were defined as those who missed medications for more than 7 days in past 3 months. These findings were similar to the study done by Adams J [17] in which 49% were fully adherent and 38% were partially adherent to the treatment, whereas study done by Maria A. Rettenbacher [9] who used similar scale and definition to assess compliance as used by us showed 52.5% of the 61 investigated patients were fully compliant, 39.3% were partially compliant, and only 8.2% were noncompliant. Rates of compliance were better in our study as it has been reported in past that noncompliance may occur in up to 50 percent of patients with schizophrenia who are prescribed neuroleptics. Study done by Olfson et al had higher number of compliant patient (80.8%) than complaint patients (19.2%).[18] In a study done by Srinivasan and Thara [19] at SCARF, Chennai revealed that up to 58% schizophrenic patients had a history of non-compliance during the course of treatment.
Thirty-five patients in our study group believed that there are problems taking medications for schizophrenia (table 4). Medicines having side effects was found to be the most common reason in sample size of 50 patients (32 – yes, 18 – No). 26 patients experienced medicines to be expensive, whereas 24 found to be non-expensive. Majority of the patients in our study group (78%, n=39) believed that compliance can be improved if they are praised when they take medicines on time. Other methods which could improve compliance according to our patients were “warning about the consequences” if medicines are not taken on time and “showing course of their illness during relapse as described in their hospital medical notes”. Other factors which made them more compliant to treatment was their belief that medicines prevent relapses and made them feel better (n=38, 76%). We also studied relationship between compliance and patient’s belief that medicines keep them in good mental health. There was a significant positive correlation between two (p=0.005). 20 of 21 fully compliant patients believed that medicines are helpful in keeping them in good mental health. 6 out of 8 non-compliant patients believed otherwise.
Insight
In our study group of 50 patients, 30 patients (60%) believed they had a mental illness, 9 (18%) were somewhat sure (unsure whether he/she had mental illness but could entertain the idea that he/she might) and 11 patients (22%) were unaware that they had a mental illness. The level of insight was higher in our study as compared to few of the previous studies as they estimate that between majority of patients with schizophrenia do not believe they have a disorder. [20] The study done by Pyne came out with similar results compared to our study in which he found that 63% of patients believed they had mental illness, whereas 37% were not aware of their illness. [21]
We also studied relationship between insight and belief that medicines help in keeping patients in good mental health. The relationship was found to be highly significant (p=0.0001). 28 out of 30 patients having full insight believed that medicines keep them in good mental health. Only 2 out of 9 patients with no insight believed the same (table 5). When patients were asked to relate schizophrenia to other diseases or disorders, more patients judged (n=26,52%) schizophrenia to be less severe than cancer. This is similar to study done Rettenbacher in which 72% of the patients judged schizophrenia to be less severe too. [22]
Achieved effects of medication
Patients awareness of achieved effects of medication was also assessed which showed that 34 patients were aware that medicines have lessened the intensity or frequency of their symptoms, whereas 7 were partially aware and 9 were unaware. This had a statistically significant relationship with compliance as 18 out of 21 compliant patients were aware that medicines have been beneficial and only 1 out of 8 non-compliant patients believed the same(table 6). This finding is similar to the findings of study done by Lin & Spiga who found that 36% of patients were compliant to treatment in perceived benefits group as contrast with only 15% of the group that had not perceived benefits from medication. [23]
Relationship between insight and compliance
The relationship between insight and compliance in our study was found to be statistically highly significant (p=0.001). 18 out of 21 compliant patients had full insight into their illness whereas none of the 8 non-compliant patients were aware of their illness. Also, 12 of 21 partially compliant patients had insight into their illness. This positive relationship between insight and compliance has been consistently found in previous studies in which it has been seen that poor insight is associated with noncompliance ([Table 7]).
Few studies have reported that patients with better medication compliance had better insight into mental illness. [24], [25] Other studies have reported an association between a lack of insight at hospital admission, discharge, or post discharge assessment and poor outpatient compliance. [26], [27] Whereas in a study done by Cuffel et al the relationship between awareness of illness and adherence was not found to be significantly positive. [28]
Conclusion
The present study attempted to assess insight and compliance, and to find out relationship between these two in patients with schizophrenia. The study was conducted on 50 patients attending Psychiatry outpatient department or admitted in psychiatric ward of a tertiary care hospital. The patients were assessed after applying inclusion and exclusion criteria. The compliance was assessed using Adherence to medication regimen and insight was assessed using SUMD.
We found a statistically significant relationship between insight and compliance in our study group (p=0.001). It was seen that patients having good compliance had better awareness about their illness. Patients with good compliance were also more aware of the beneficial effects of the treatment (p=0.007). There was also a statistically significant relationship between insight, compliance and patient’s belief that medications help in keeping them in good mental health (p=0.0001).
This study emphasizes the importance of insight facilitation for the patient and psychoeducating the caregivers regarding the nature of illness, for better compliance towards medications.
Limitations of the study
The sample size was relatively small as it was a hospital-based study
It was a cross-sectional study and patients were not followed up, so we cannot draw conclusions about the direction of observed relationships.
For assessing compliance, ideally drug assays should be used, but drug assays for anti-psychotics are not available in our setting. In this study measuring instruments were used. The instruments are based on patients’ report and can overestimate the compliance.
Conflict of Interest
The authors declare that there is no conflict of interest.
Source of Funding
None.
References
- Blackwell B. Drug therapy: patient compliance. N Engl J Med. 1976;289(5):249-52. [Google Scholar] [Crossref]
- Fenton WS, Blyler CR, Heinssen RK. Determinants of medication compliance in schizophrenia: empirical and clinical findings. Schizophr Bull. 1998;23(4):637-51. [Google Scholar] [Crossref]
- Millas WD, Lambert M, Naber D. The impact of subjective wellbeing under neuroleptic treatment on compliance and remission. Dialogues Clin Neurosci. 2006;8(1):131-6. [Google Scholar] [Crossref]
- Sadock BJ, BS, VS, PR. Psychiatric report, medical record and medical error. Kaplan and Sadock’s comprehensive textbook of psychiatry. 9th Edn.. 2009;1:907-18. [Google Scholar]
- Hogan TP, Awad AG. Subjective response to neuroleptics and outcome in schizophrenia: a re-examination comparing two measures. Psychol Med. 1992;22(2):347-52. [Google Scholar]
- Naber D. A self-rating to measure subjective effects of neuroleptic drugs, relationships to objective psychopathology, quality of life, compliance and other clinical variables. Int Clin Psychopharmacol. 1995;10(3):133-8. [Google Scholar]
- Voruganti K, Heslegrave RJ, Awad AG, Seeman M. Quality of life measurement in schizophrenia: reconciling the quest for subjectivity with the question of reliability. Psychol Med. 1998;28(1):165-72. [Google Scholar]
- Lambert M, Schimmelmann BG, Karow A, Naber D. Subjective well-being and initial disphoric reaction under antipsychotic drugs-concepts, measurement and clinical relevance. Pharmacopsychiatry. 2003;36(3):S181-90. [Google Scholar] [Crossref]
- Rettenbacher MA, Hofer A, Eder-Ischia U, Hummer M, Kemmler G, Weiss E. Compliance in schizophrenia: psychopathology, side effects, and patients' attitudes toward the illness and medication. J Clin Psychiatr. 2004;65(9):1211-8. [Google Scholar] [Crossref]
- Amador XF, Strauss DH, Yale SA, Flaum MM, Endicott J, Gorman JM. Assessment of insight in psychosis. Am J Psychiatry. 1993;150(6):873-9. [Google Scholar] [Crossref]
- Kao YC, Liu YP. Compliance In Schizophrenia: the predictive potential of insight into illness, symptoms and side effects. Compr Psychiatry. 2010;51(6):557-65. [Google Scholar] [Crossref]
- Padmavathi R, Rajkumar S, Srinivasan TN. Schizophrenic patients who were never treated-a study in an Indian urban community. Psychol Med. 1998;28(5):1113-7. [Google Scholar] [Crossref]
- Rocca P, Crivelli B, Marino F, Mongini T, Portaleone F, Bogetto F. Correltaions of attitude toward antipsychotic drugs with insight and objective psychopathology in Schizophrenia. Compr Psychiatry. 2008;49(2):170-6. [Google Scholar] [Crossref]
- Staring BP, Gaag MVD, Koopmans GT, Selten JP, Beveren JMV, Hengeveld MW. Treatment adherence therapy in people with psychotic disorders: randomised control trial. Br J Psychiatry. 2010;197(6):448-55. [Google Scholar] [Crossref]
- Fleischhacker WW, Meise U, Giinther V, Kurz M. Compliance with antipsychotic drug treatment: influence of side effects. Acta Psychiatr Scand. 1994;328:11-5. [Google Scholar]
- Sarvanan B, Jacob KS, Johnson S, Prince M, Bhugra D, David AS. Assessing insight in schizophrenia: East meets West. Br J Psychiatry. 2007;190:243-7. [Google Scholar] [Crossref]
- Adams J, Scott J. Predicting medication adherence in severe mental disorders. Acta Psychiatr Scand. 2000;101(2):119-24. [Google Scholar] [Crossref]
- Olfson M, Mechanic D, Hansell S, Boyer CA, Walkup J, Weiden PJ. Predicting medication noncompliance after hospital discharge among patients with schizophrenia. Psychiatr Serv. 2000;51(2):216-22. [Google Scholar] [Crossref]
- Srinivasan TN, Thara R. Management of medication noncompliance in schizophrenia by families in India. Schizophr Bull. 2002;28(3):531-5. [Google Scholar]
- Trauer T, Sacks T. The relationship between insight and medication adherence in severely mentally ill clients treated in the community. Acta Psychiatr Scand. 2000;102(3):211-6. [Google Scholar] [Crossref]
- Pyne JM, Bean D, Sullivan G. Characteristics of patients with schizophrenia who do not believe they are mentally ill. J Nerv Ment Dis. 2001;189(3):146-53. [Google Scholar] [Crossref]
- Rettenbacher MA, Burns T, Kemmler G, Fleischhacker W. Schizophrenia: Attitudes of patients and professional carers towards the illness and antipsychotic medication. Pharmacopsychiatry. 2004;37(3):103-9. [Google Scholar] [Crossref]
- Lin IF, Spiga R, Fortsch W. Insight and adherence to medication in chronic schizophrenics. J Clin Psychiatry. 1979;40(10):430-2. [Google Scholar]
- Marder SR, Mebane A, Chien C. a comparison of patients who refuse and consent to neuroleptic treatment. Am J Psychiatry. 1983;140(4):470-2. [Google Scholar] [Crossref]
- Mcevoy JP, Apperson U, Appelbaum PS, Ortlip P, Brecosky J, Hammill K. Insight in schizophrenia: its relationship to acute psychopathology. J Nerv Ment Dis. 1989;177(1):43-7. [Google Scholar] [Crossref]
- Bartko G, Herczeg I, Zador G. Clinical symptomatology and drug compliance in schizophrenic patients. Acta Psychiatr Scand. 1988;77(1):74-6. [Google Scholar] [Crossref]
- Putten TV, Crumpton E, Yale C. Drug refusal in schizophrenia and the wish to be crazy. Arch Gen Psychiatry. 1976;33(12):1443-6. [Google Scholar] [Crossref]
- Cuffel BJ, Alford J, Fischer EP, Owen RR. Awareness of illness in schizophrenia and outpatient treatment adherence. J Nerv Ment Dis. 1996;184(11):653-9. [Google Scholar] [Crossref]
How to Cite This Article
Vancouver
Hyder S, Monga A, Paisari P, Kunjumoidee RR. A study of compliance and insight in patients with schizophrenia [Internet]. IP Indian J Neurosci. 2022 [cited 2025 Sep 27];8(1):50-56. Available from: https://doi.org/10.18231/j.ijn.2022.010
APA
Hyder, S., Monga, A., Paisari, P., Kunjumoidee, R. R. (2022). A study of compliance and insight in patients with schizophrenia. IP Indian J Neurosci, 8(1), 50-56. https://doi.org/10.18231/j.ijn.2022.010
MLA
Hyder, Shafeen, Monga, Abhinav, Paisari, Pradeep, Kunjumoidee, Raihana Rasheed. "A study of compliance and insight in patients with schizophrenia." IP Indian J Neurosci, vol. 8, no. 1, 2022, pp. 50-56. https://doi.org/10.18231/j.ijn.2022.010
Chicago
Hyder, S., Monga, A., Paisari, P., Kunjumoidee, R. R.. "A study of compliance and insight in patients with schizophrenia." IP Indian J Neurosci 8, no. 1 (2022): 50-56. https://doi.org/10.18231/j.ijn.2022.010
