Introduction
The current waves of COVID-19 spread have been a public health emergency and global threat that compelled the governments to implement extended periods of lockdown now and then by ordering their citizens to stay at home as an early and effective way for preventing this pandemic.1 Under such situations, the physical emotional and mental health problems of children and their parents are of significant concerns.2 Particularly, children routine, such as play, physical activity, studies, socialization, recreation, may have been drastically impacted due to the prolonged school closures and home confinement during the COVID-19 pandemic.3 Children and their families may be particularly vulnerable to disease severity and inadvertent arms of public health measures during pandemics and have been previously defined as a high-risk population for negative impacts during an outbreak.4, 5 The Lockdown period started from 19th March 2020 in both the states of Telengana and Andhra Pradesh led to phase wise closed down of childcare centres, schools, junior colleges, play grounds, recreational centres, workplaces and other public places making the whole family to confine themselves to their homes creating critical periods in their interactive relationships with parents or significant others. In India, majority of the families live in moderate to poor housing conditions, which makes provision for online classes, social distancing and home isolation/ quarantine at times difficult. Especially controlling children in early childhood age group (3 to 9 years) by parents is a daunting task because self-control only begins to form in them and so is the ability to relate moral principles and amid these two poles where fear of getting infected by COVID-19 clearly varied in their perception and actions, should a major stress happens, egocentrism may occur wherein it is difficult for children to take up another’s point of view and their normal stage of development or temperamental process leaves them vulnerable. There is evidence that children not only shape their environment but also elicit different responses from the external environment which affects their brain and mind development in such critical periods. Onset of all these unforeseen problems may cause distress among the parents and may affect the family equilibrium and influence the parenting practices further causing higher likelihood of mental health problems among these children. Many of the disturbances in early childhood are either ignored for considering immature responses or commonly thought to be transient, with this background an attempt was made to assess the impact of COVID-19 lockdown period on seven domains of mental health from temperament to psychiatric disorders of 3 to 8 years of children from the State of Telengana and Andhra Pradesh in India.
Materials and Methods
The study was a qualitative explorative research conducted in collaboration with 2 medical institutes (KIMS Narkatpalle and GMC, Hyderabad) from State of Telangana and a Women’s University (SPMVV, Tirupati, AP) from October to December 2020 after receiving the IEC approval. Since it was difficult to reach out children or their families personally, a snow ball method of sampling was used through online (Google form) questionnaire and posted on “Whatsapp” of parents of children with the help of school teachers by contacting the schools in the vicinity of Nalgonda, Tirupati and Hyderabad in Telengana and Andhra Pradesh states. We received the contacts of parents from the school administrations, who in turn posted the questionnaire link to other parents or friends known to them. Oral consent of the parents (preferably mother) was included in the questionnaire as a first statement and their response as ‘yes’ was considered as their consent. The questionnaire was constructed to assess the mental health and wellbeing of children as perceived by their parents. The number of items and the seven domains of mental health included were; Temperament (5items from Temperament Measurement Scale, 6 Behavioural Disturbance (7 items from CBCL / Childhood behavioural checklist7, Positive Strength (6 items from Strengths and difficulties questionnaire,7 Attachment (3 items from Parent Interview Schedule),8 Socialization (2 items), Coping Mechanism (5 items),9 Psychiatric Disorders (8 items7). The online questionnaire on mental health and wellbeing of early child hood age group (3 to 9 years) during COVID 19 lockdown, thus consisted of total 35 items presented under these seven mental health dimensions in English language. Thus, only those parents who were well versed in English could attempt and complete the questionnaire which usually took 10 to 12 minutes of time. The null hypotheses and its alternate were formulated for Temperament, Behavioral Disturbance, Positive Strength, Attachment, Socialization, Coping Mechanism, Psychiatric Disorders assumed that distribution and patterns of these dimensions were in normative phase in the children aged between 3 to 9 years. The research data was analyzed using SPSS (21.01 version), appropriate descriptive and inferential statistics were computed for qualitative and quantitative data. For example, results on continuous measurements were presented on Mean ± SD (Min-Max) and results on categorical measurements were presented in frequency and percentage. These null hypotheses for each subdomain were tested using Kruskal -Wallis H test since it is a non-parametric test which can be used as generalized form of Mann Whitney U test. It assesses the differences against the average rank or group in order to determine whether or not they are likely to have come from samples drawn from same or identical population considering the snowball sampling. A p value less than 0.05 was considered to be significant.
Results
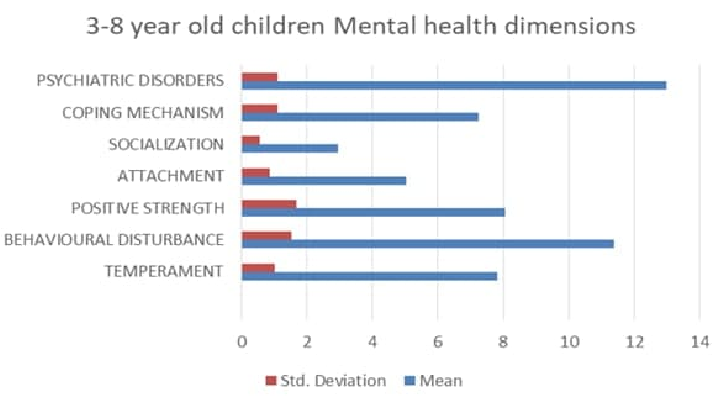
The results of this qualitative explorative study by broadly contextualizing some of the mental health impacts and challenges for children and young people and planning and implementing appropriate mental health and wellbeing interventions to support children and young people to resume to normal life, or the ‘new normal’. The responses received were 173 of which 17 were invalid and the total sample comprised of 156 parents of children (3-8 years). The data was subjected to statistical analysis using SPSS to examine the association between the age and mental health in seven domains and also the gender and mental health. In addition, the Kruskal -Wallis H test was used alternative to the one way ANOVA as the data is non parametric for testing the Null hypotheses formulated. The Table 1, shows the means, standard deviations, mode, median, minimum and maximum score for each mental health dimension indicating the distribution of values of the sample. Furthermore the Percentile ranks are also given to clarify the interpretation of scores; the 25th percentile is the value at which 25 percent of the answers lie below that value, and 75 percent of the answers lie above that value. 50th Percentile is also known as the Median and the 75th Percentile is referred as the third, or upper quartile. The percentage is a mathematical value presented out of 100 and percentile is the per cent of values below a specific value.10 The lower the percentile rank for a dimension, the more positive response it has received compared to items in the same domain in that quarter. In table 1, the values under temperament dimension at the corresponding percentile quarter indicates that the scores is among that percentage of responses; 7% at 25th, 8% at 50th, 8% at 75th and other percentage of scores; 93%,92%,92% respectively had less impact. The mean value of all the seven mental health dimensions reveal that they are closer to their respective median values indicating that they are at fifty percent of the scores. Moreover, the SDs of the seven dimensions; temperament- 1.019, Behavioural Disturbance-1.700, Positive Strength -1.598, Attachment-0.940, Socialization-0.627, Coping Mechanism-1.133, Psychiatric Disorders -1.094, of mental health reflect that the sample did not vary much in their perception of mental health problems among their children (3-8 years) as the SD values were less than two as shown in Figure 1.
The relationship between the age of the children and mental health dimensions was examined using chi-square test as presented in Table 2. The findings reveal that significant association was found between the age and; temperament (<0.001), behavioural disturbance (<0.001), attachment (<0.05), socialization (<0.001), coping mechanism (<0.05) and there was no significant association found between age of the child and; Positive Strength and Psychiatric Disorders at0.05 level. Similarly, the relationship between the gender of the children and mental health dimensions was studied using chi-square test as presented in table 3. The results indicate that there was no significant association found between the gender and all the seven mental health dimensions at 0.05 level of significance.
The null hypotheses formulated were tested using Kruskal –Wallis H test and the outcome was presented in Table 4, the findings reflect that four out of seven hypotheses were rejected as there was good evidence against the null hypotheses at 0.05 level of significance and three out of seven null hypotheses were retained as there was weak evidence against null hypotheses at 0.05 level.
Table 1
The mean scores and SD of children (3-8 years) in seven mental health dimensions
Table 2
Association between age and mental health dimensions of children (3-8years)
Table 3
Relationship between gender and mental health dimensions 3-8 years
Table 4
Null hypotheses test summary
Discussion
The study aimed at assessing the mental health and wellbeing of children in their early childhood during COVID 19 lockdown. The findings of the study indicated that parents perceived mental health problems in their children in seven dimensions. In table 1and figure1, the mean scores of these dimensions; temperament- 7.76, Behavioural Disturbance-11.09, Positive Strength -8.05, Attachment-5.01, Socialization-2.85, Coping Mechanism-7.02, Psychiatric Disorders -12.91 reveal that a notable percent of children had mental health and problems as the mean scores were almost nearer to the median values. Their parents did not vary much in their perception of problems in seven dimensions of mental health as the Standard Deviation values were less than 2. The young children need to be supervised in the areas of; self-care, personal hygiene, and sanitation and safety in this new situation to protect them from infection.
Due to lockdown the parents and primary care givers were the people responsible for attending to physical, social, emotional and health needs of children. These results compare well with the results of a survey conducted in UK ‘Nearly 1000 young carers in the UK found that over half of young carers have felt overwhelmed and stressed and have, as a result, suffered worsened mental health during the lockdown period and are one group whose mental health has been negatively impacted by the lockdown restrictions’.6 It was identified that those children and young people living in families where the experience of lockdown may have been particularly difficult and challenging may require additional support to deal with the mental health and wellbeing impacts of lockdown. 11
The relationship between the age of the child and mental health dimensions was studied using chi square test and presented in Table 2. The findings revealed that significant association was found between the age and; temperament (p=0.000), behavioural disturbance (p=0.000), attachment (p=0.20), socialization (p=0.06), coping mechanism (p=0.11). In contrary, no significant association found between age of the child and; Positive Strength (p=0.141) and Psychiatric Disorders (p=0.170) at 0.05 level. These results reflect that there was strong relationship between the age of the children and five mental health dimensions studied, indicating the need for equipping the parents with necessary skills to help children cope with the mental health problems.
The pandemics, like COVID-19, poses potential risks to development of children due to the chances of illness, protective confinement, social isolation, and the increased stress level of parents and caregivers.7 This situation becomes an adverse childhood experience (ACEs) and may give rise to noxious stress, with concomitant potential losses for brain development, personal and collective health, and the long-term impairment of cognition, mental and physical health, and productivity of future adults. 8
A study conducted on epidemics, highlighted that those working with vulnerable population should follow a trauma informed approach to understanding the impacts of lockdown on such groups during health-related crises.9 It has been indicated that compared to adults, this pandemic may continue to have increased long term negative consequences on children and adolescents. 11
The association between gender (boys and girls) with regard to mental health dimensions was examined by computing chi square test as shown in Table 3, which indicates that no significant relationship was found between the gender and all the seven mental health dimensions at 0.05 level of significance. Which elucidates that the boys and girls under the study did not differ in exhibiting their problems related to seven mental health dimensions. Regarding gender, the results point in the opposite direction as the ones found by Zhou et al., that female gender was the higher risk factor for depressive and anxiety symptoms during COVID 19 confinement.12 Younger children can experience panic of the virus, frustration, boredom, loneliness, and lack of space at home, leading to repercussions that may go beyond the quarantine period. 13 Countries which are less restrictive in their COVID-19 containment measures, such as Germany, appear to have received less impact on the mental health of minors. 14 The psychological impacts are particularly important to consider in cases where parents are front-line workers with much evidence showing that those working in health care in particular, experience negative psychological consequences during health emergencies. 3
The Table 4 presents the summary of null hypotheses tested using Kruskal –Wallis H test to examine the significant difference between groups. In the present study seven null hypotheses were formulated to know the distribution of each mental health dimension is same across the age group of children (3-8 years).
It was found that null hypotheses formulated on; Behavioural Disturbance, Attachment, socialization, coping Mechanism were rejected at 0.05 level of significance as there was evidence against these null hypotheses. Which reveals that the children varied across the age group in these four mental health dimensions. In contrary, the null hypotheses; Temperament, Positive Strength and Psychiatric Disorders, tested were retained owing to lack evidence against these null hypotheses. Which explains that there was no variation among the age groups of children with regard to these three mental health dimensions. The study results compares well with another study, which showed that the strict confinement situation of children and teenagers revealed significant consequences on the mental health of both of them. It appears that the consequences of confinement on children are mostly in the affective area, this also being reflected at the behavioural level.15 In terms of the delivery of education during lockdown, there has been concern over the exclusion of children without digital access, physical space, and other resources to support their learning.
Emerging evidence from England suggests that there has been a substantial gaps in curriculum coverage across schools, that just over half of parents were engaged with their children’s home learning, and the disadvantaged students were deprived of academic engagement 16 and those receiving free school meals may have experienced ;increasing food insecurity, deprivation of nutritional and educational needs. Moreover, in many cases where a single parent or both the parents were infected and quarantined, the children were separated from the parents.17 A review by Nearchou et al.18 found only 12 researches on child and adolescent mental health during the COVID-19 pandemic, all had quantitative cross-sectional designs. Two of these 12 studies used parents as informants, four investigations used adults in their samples and the sample of minors did not exceed n = 3435 and only two studies conducted in China valuated children. 19, 20, 21
Studies showed that the nature and extent of this impact depend on several vulnerability factors such as the developmental age, educational status, pre-existing mental health condition, being economically underprivileged or being quarantined due to infection /fear of infection. There is a need to ameliorate children and adolescent's access to mental health services by using both face to face as well as digital platforms. 22
Conclusion
The study results allows to conclude that the parents of children in their early childhood perceived problems in seven mental health dimensions during this COVID 19 lockdown period. The children varied across their age group in four out of seven mental health dimensions; Behavioural Disturbance, Attachment, socialization, coping Mechanisms indicating differences in problems displayed. The findings elucidate that the boys and girls under the study did not differ in exhibiting their problems related to seven mental health dimensions indicating no association between gender and mental health dimensions of children in this age group. However, there is a great need to prepare the children and their families to overcome the present mental health problems and learn the ways to face the post COVID19 challenges through appropriate multi sectoral intervention programmes.