Introduction
The SARS-CoV-2 virus, which has led to the Covid -19 Pandemic, is responsible for severe respiratory illnesses like pneumonia and even multiorgan failure. Several organs have been affected by COVID-19, but neuro-ophthalmologic manifestations due to Optic Neuritis, Cranial nerve palsies, Miller Fischer variant of Guillain-Barre syndrome, Intracranial hypertension, Posterior circulatory stroke, Posterior reversible encephalopathy syndrome (PRES), etc. have seldom been reported. 1 Optic neuritis, unilateral or bilateral, is an unusual complication following Covid-19 Infection. Optic neuritis is characterized by the visual loss that begins suddenly and reaches its maximum severity in a week. It is often associated with periorbital pain, which increases eye movements. 2
Clinical Vignette
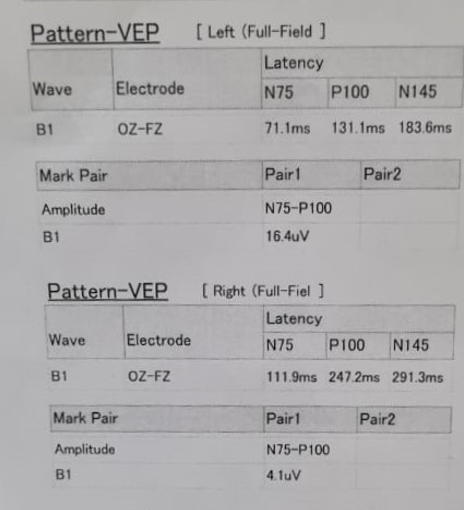
A 16-year-old was diagnosed with mild covid illness based on his clinical symptoms and positive Covid-19 Nasopharyngeal RT- PCR result and was home quarantined for that. On the last day of the quarantine, he noticed reduced vision and periorbital pain in the Right eye, which progressed over three days. On examination of the Right eye, he had Relative Afferent Pupillary Defect, Best Corrected Visual acuity of 6/60, and defective colour vision. Fundus examination shows disc oedema in Rt eye, and the rest of the eye examination in both eyes was within normal limits. VER shows prolonged P100 latency in the Right eye. MRI Brain showed hyperintensities of Rt optic nerve on T2 axial and coronal fat-suppressed images, which were enhancing on T1 axial contrast images. The rest of the MRI Brain and Spine was unremarkable. CSF examination, ADA, cytology, all stains, pan neurotropic virus panel, Oligoclonal bands, etc., were all within normal limits. The patient's Covid antibodies came out to be positive, and RT PCR for Covid -19 virus in the Nasopharyngeal swab was negative. The rest of the Blood investigations, like aquaporin-4 and anti-MOG antibodies, ANA, ACE levels, C- ANCA, p- ANCA, HIV, VDRL, etc., were negative. The patient was diagnosed with Probable Covid -19 induced optic neuritis and started on i/v Methyl Prednisolone 1gm once a day for three days, followed by tapering dosages of oral steroids with which he recovered completely.
Figure 2
Visual Evoked Response – Shows Prolonged P100 latency and reduced amplitude in Right Eye and normal P100 latency and amplitude in Left eye.
Discussion
Since the onset of the coronavirus pandemic, numerous cases highlighting the neurological complications of the infection have been reported.3 Furthermore, neuro-ophthalmological manifestations have emerged as separate entities with multiple proposed underlying mechanisms.4
We report a rare case of Post covid-19 Right eye Optic neuritis in a 16-year-old boy. We are labelling it as a case of Probable Post Covid -19 Right Eye optic neuritis based on temporal association with Covid -19 infection, after ruling out other aetiologies and finally as per the provisional case definitions for the association of COVID-19 with neurological disease suggested by Mark Ellul et al. panel.3
Optic neuritis is an inflammation of the optic nerve diagnosed based on history, ocular examination including fundus, Visual Evoked Responses, and Contrast MRI Brain with optic nerve cuts.2, 5 The aetiology of optic neuritis includes infections, toxins, drugs, connective tissue, paraneoplastic, inflammatory and demyelinating disorders, etc.5 Fundus examination is normal in Retrobulbar Optic Neuritis, and it shows disc oedema in optic papillitis as in our patient. Similar to our case, several authors have published cases of Covid -19 related to Optic Neuritis in literature. Azab, Mohammed A et al. reported a post-COVID-19 case of optic neuritis and the first meta-analysis of published case reports in July 2021.6 Covid -19 related optic neuritis can be unilateral or bilateral. Optic Neuritis may be the only complication of Covid-19 infection 6 or sometimes associated with pan uveitis and retinitis. 7 In some patients, Optic Neuritis was a part of multifocal involvement of the Central Nervous System, i.e., Acute Disseminated Encephalomyelitis. 8 Furthermore, it developed as a part of a syndrome called anti-MOG syndrome in others. 9 It should also be noted that in some patients, optic neuritis may be the initial presentation of Multiple sclerosis, whose onset is triggered by COVID-19 infection. 10
Optic Neuritis can occur para-infectiously or post-infectiously. Although several hypotheses have been proposed so far, there has been no definite proof of the mechanism by which COVID-19 induces or triggers the onset of optic neuritis. One possibility is direct viral invasion as COVID-19 is known to enter the cells using ACE2 receptors, which are found on the neurons and the choroidal cells in the eyes and can lead to uveitis and optic neuritis. 4 Cytokine storm is another mechanism that is debated as the cause of neuro-ophthalmological complications of COVID-19. The intense release of cytokines including Interleukin 6 can overstimulate the human body's immune system 1 and can potentiate the development of demyelinating injury to the optic nerve. In cases where optic neuritis occurs as a part of the anti-MOG syndrome, or Neuromyelitis Optica spectrum disorders or ADEM or after recovery from COVID-19 molecular mimicry is the most plausible mechanism whereby viral antigens initiate a robust immune response against endogenous central nervous system proteins, including MOG and the myelin of the optic nerve. 4
Conclusion
Optic Neuritis is an uncommon complication seen during and after Covid -19 infection. Physicians should always suspect this entity after encountering patients presenting with rapid onset vision loss following Covid-19 infection, as delay in the diagnosis and treatment might affect the outcome. Early treatment with steroids may give gratifying results, as in our case. Furthermore, these patients should be periodically monitored to rule out the development of other demyelinating disorders in the future.






