Introduction
This report presents a comparison of non-contrast CT (NCCT) and diffusion weighted imaging (DWI) findings in a patient with anoxic brain injury following cardiac arrest. NCCT is typically the first-line of neuroimaging investigations obtained and the most widely used modality for imaging ischemia due to its widespread availability, faster acquisition times and lower cost. DWI however, despite its longer acquisition time is generally considered to be the gold standard.1 We present a case here which shows despite its widespread use, DWI may not always capture the full extent of parenchymal changes during anoxic brain injury.
Case Report
A 65 year old male patient with a history of hypertension, obesity, smoking, obstructive sleep apnea and chronic obstructive pulmonary disease presented to the hospital from home via emergency medical services (EMS). Prior to this, the patient had been experiencing 2 weeks of vague chest pain and during the morning of emergency department (ED) presentation went into sudden witnessed cardiac arrest. On arrival, the patient was found to be in pulse less electrical activity (PEA) arrest by EMS. After 15 minutes of cardio pulmonary resuscitation (CPR) the patient achieved return of spontaneous circulation (ROSC) but unfortunately went on to have a second event requiring an additional 7 minutes of CPR. After achieving ROSC for the second time, the patient’s initial electrocardiogram (ECG) showed ST elevation myocardial infarction along with troponins >30,000 ng/L. Dual antiplatelets (Aspirin and Clopidogrel) were started right away and patient received cardiac catheterization with two drug eluding stents for his proximal left anterior descending (LAD) occlusion. Patient’s hospital stay was also complicated with a pneumothorax which was managed with a pigtail drain.
The neurology team was consulted for neuroprognostication post-cardiac arrest. On exam there were no signs of myoclonus, pupils were 2 mm and equal bilaterally with very minimal reactivity to light. Patient had roving eye movements and doll’s eyes. Corneal, nasal tickle, gag, cough, knee and ankle reflexes were absent. Peripheral and central pain responses were absent and patient did not demonstrate any grimace to noxious stimuli. Patient remained intubated with an FiO2 of 40% and vitals were stable.
A non-contrast CT scan was performed which showed global loss of Gray-White matter differentiation in the cortical regions and generalized sulcal effacement (Figure 1a). Pronounced hypoattenuation was seen in the basal ganglia (Figure 1 b) as well as the medial occipital lobes bilaterally (Figure 1c).
Figure 1
Non-contrast CT head showing; a): Loss of gray-white differentiation and sulcal effacement; b): Hypoattenuated caudate and lentiform and c): Medial occipital lobe hypo-attenuation

Figure 2
MR DWI showing restriction diffusion in; a): Cortical regions; b): The caudate nuclei, lentiform nucleus and the forniceal columns; c): Hyperintensity in bilateral hippocampi and medial occipital lobes; and d): Left amygdala.
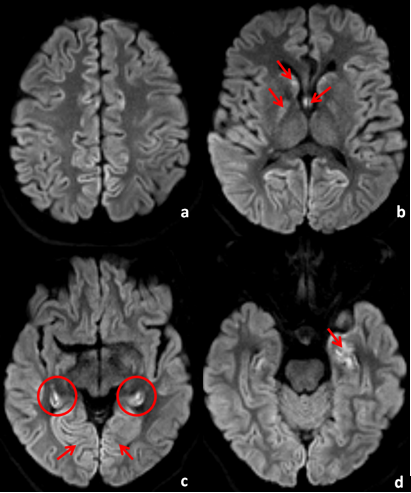
The CT scan was followed by a brain MRI 3 days later which showed restricted diffusion on DWI involving the caudate nuclei, globus pallidus and the forniceal columns (Figure 2a). There was also restricted diffusion and cortical hyperintensity seen in bilateral hippocampi (Figure 2b) as well as within the left amygdala (Figure 2c).
In consultation with the patient’s family, the decision was made to switch to comfort measures. This was done a few days later and the patient passed peacefully surrounded by his family only few minutes after withdrawing life support.
Discussion
Although it is often presumed to be the most sensitive modality for delineating the extent of parenchymal ischemia and for neuroprognostication, this report demonstrates that NCCT can sometimes outperform DWI in better characterizing the extent of parenchymal injury. Therefore, NCCT should not be discounted as an important tool during neuroprognostication.
Cardiac arrest is one of the main causes of global anoxic brain injury.2 The primary mechanism behind ischemic insult is a mismatch between arterial oxygen content and increased metabolic demand in brain hypoxia. This progresses to cytotoxic edema, then ionic edema and lastly through inflammation and programmed cell death which is typically spread and exacerbated secondary to peri-infarct depolarizations. 3 Following acute ischemia, there is an inverse relation between an increase in brain water content and CT attenuation measured in Hounsfield units (HU) with studies reporting as much as 1% increase in water content can lead to a subsequent decrease of between 1.8 – 2.5 HU.4 The pattern of imaging findings secondary to global anoxic brain injury however, has not been studied very well.
Animal models have shown that the hippocampi and basal ganglia structures including the caudate nucleus and thalamus are the most susceptible to acute ischemic injury.5 Imaging characteristics of these regions post global anoxic injury have not been very well described in literature. Moreover, diffusion restriction does not always necessitate irreversible areas of parenchymal injury which can complicate assessment and prognostication. For instance, it is known that diffusion restriction in transient global ischemia (TGA) has been described as short term with no resulting permanent infarction.6 In other conditions such as posterior reversible encephalopathy syndrome (PRES) diffusion restriction has been described to resolve in most, though not all, patients.7 DWI has been widely established to represent cytotoxic edema secondary to ischemic injury at higher thresholds of cerebral blood flow than CT thus making it the favoured imaging modality.4 Placing disproportionate emphasis on DWI however, may in occasional cases lead to underestimating the true extent of infarction in patients.
Conclusion
This case report provides valuable insight into the importance of appearances on NCCT alongside DWI in neuroprognostication as relying only on the latter may underestimate the true extent of parenchymal infarction. Although diffuse loss of Gray-White matter differentiation consistent with global anoxic brain injury was seen on CT, DWI 3 days later, only showed diffusion restriction and hyperintensity in select areas. DWI hyperintensity was seen in diverse structures including the hippocampi, globus pallidus, forniceal columns, medial occipital lobes as well as the left amygdala.
Further studies elucidating the pattern of ischemic involvement at different time points in anoxic brain injury is crucial. It is also important to study the relative advantages and disadvantages of NCCT and DWI in prognostication of anoxic brain injury. This will also aid in unveiling new knowledge concerning the pathophysiology behind anoxic brain injury.
Key Points
Global anoxic brain injury has characteristic imaging findings on CT and DWI. Recognition of these findings is instrumental for a timely diagnosis.
CT may demonstrate global loss of Gray-White matter differentiation and sometimes be a better prognostic indicator in determining the extent of parenchymal injury.
Further studies are needed to elucidate the pattern of DWI restriction secondary to anoxic brain injury.
