- Visibility 43 Views
- Downloads 6 Downloads
- DOI 10.18231/j.ijn.2021.044
-
CrossMark
- Citation
A rare variant of chronic inflammatory demyelinating polyneuropathy with autonomic dysfunction
- Author Details:
-
Jayaraj K *
-
Shaji C V
-
Kabeer K A
-
Prashanth S R
Introduction
The spectrum of CIDP (chronic inflammatory demyelinating polyneuropathy) is generally known to present as progressive symmetric proximal and distal weakness, large fiber sensory loss, and areflexia, with a peaking of symptoms more than 8 weeks after symptom onset. The type of nerve fibers affected and pattern of deficits differ depending on the variant in the continuum.[1] In comparison with GBS, in which autonomic dysfunction is a common and a well-recognized complication, infrequent and mild autonomic complaints have been described in patients with CIDP.[2] Here we report a rare variant of CIDP in the background of a connective tissue disease presenting with prominent bladder dysfunction along with other neurological symptoms.
Case Report
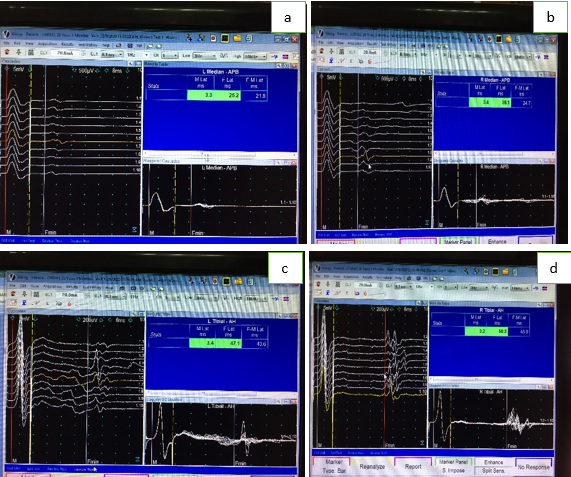
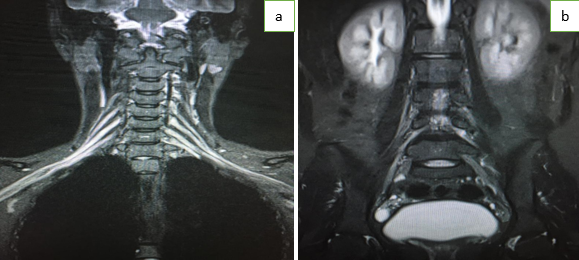
A 26 year old hypothyroid female working at Pune presented with complaints of parasthesias of upper extremities since 8 weeks. She gives history of insidious onset slowly progressive disabling cramping pain felt initially, on both calves which ascended above the knees. She had associated dull aching pain on both shoulders, upto the elbows which subsided spontaneously after a week. 3 days after the onset of cramping pain, she had electric shock like sensations radiating up from the fingers to the shoulder. 2 days after the onset of upper limb symptoms, she felt pins and needles sensations confined to soles of both feet which progressed up to the perineal region over 2 weeks. At that point of time, she had transient bladder symptoms lasting few days with difficulty in emptying the bladder completely and had to void again with her bladder sensations and bowel functions remaining intact. Weakness of right upper limb was noticed 3 weeks after the onset of pain, in the form of difficulty in holding pen, buttoning, and writing which progressed over next 1 week. She also noticed proximal muscle weakness in the form of difficulty in washing face, combing her hair which progressed over 1 week. 2 weeks after the onset upper limb weakness, she felt insidious onset gradually progressive weakness of lower limbs in the form of difficulty in getting up from squatting position with a tendency to buckle. Subsequently she had distal muscle weakness in the form of unsteadiness of ankle and difficulty in gripping her sandals. There was no history of trunk or neck muscle weakness, facial, bulbar or other cranial nerve symptoms or limb incoordination or swaying while walking. There was no history of fever, rashes, systemic symptoms or exposure to drugs or toxins. There was history of puffy fingers and small joint inflammatory pain one month prior to the symptoms. No prior history of diarrhoeal illness or animal or insect bite, recent vaccinations, diabetes, malignancies, tuberculosis or jaundice. General Examination and vitals did not reveal any signs of autonomic dysfunction. Cranial nerve examination was normal. Neurological examination showed symmetrical proximal and distal weakness of upper and lower limbs (MRC grade 4-) with absent deep reflexes and retained anal reflex and flexor plantars. Vibration sense was impaired till metatarsophalangeal joints bilaterally. Joint position sense was impaired in the 4th and 5th digits on upper and lower limbs bilaterally. Rhombergs was negative. Perineal and perianal sensations were perceived but diminished. Peripheral nerves appeared thickened. Rest of the systems were within normal limits. Laboratory evaluation showed normal haemogram with raised ESR (100mm), normal blood sugars, renal and hepatic functions. Electrolytes were normal and viral markers including HIV were negative. Antinuclear antibody was positive with profile showing nRNP/Sm positivity marker suggestive of Mixed Connective Tissue Disease, which needs repetition at an interval during follow up. Anti neutrophil cytoplasmic antibody was negative. Serum electrophoresis was negative. Urine electrophoresis, immunofixation and free light chain assay was not done. Anti Thyroid peroxidase antibody titre was high - 277.70 IU/ml (<45) suggesting thyroid autoimmunity. Chest X ray and sonography of abdomen and pelvis was normal. Initial Nerve conduction studies showed normal Compound Muscle Action Potential, Sensory Nerve Action Potential and conduction velocities and distal latencies in both upper and lower limbs (1[Figure 1]). Initial F wave latency was normal which was found to be prolonged on a repeat study after 2 weeks .Cererebrospinal study showed albuminocytological dissociation (protein – 84 mg/dl, No cells). Serum Anti ganglioside antibody panel was negative. Magnetic resonance T2 Short Tau Inversion Recovery sequence showed hyperintense signals of cervical and lumbar nerve roots on both sides extending to the trunks and plexus s/o hypertrophy and thickening of nerve of nerves.([Figure 2]). Patient was treated with intravenous immunoglobulin for 5 days and was started on oral steroids (prednisolone) on slow tapering doses to which she responded well.
Discussion
CIDP is differentiated from Guillain-Barré syndrome by a protracted time course, absence of significant life threatening autonomic dysfunction, and absence of respiratory impairment in most patients. The atypical CIDP variants do not conform to the common pattern of symmetric generalized weakness with length-dependent sensory deficits as in case a typical CIDP. These polyneuropathies broadly differ in clinical syndromes as sensory predominance (eg, sensory CIDP), motor predominance (eg, motor CIDP or multifocal motor neuropathy [MMN]), asymmetry (eg, multifocal acquired demyelinating sensory and motor neuropathy [MADSAM]), or distal predominance (eg, distal acquired demyelinating symmetric [DADS] neuropathy.[1], [3] Immune mediated demyelinating radiculopathies restricted to proximal sensory or motor root involvement are uncommon with the sensory variant called as chronic immune sensory polyradiculopathy (CISP) and motor variant as chronic immune motor polyradiculopathy(CIMP).[4], [5] The term chronic immune sensory motor polyradiculopathy (CISMP) comprises the core features of the mixed form of immune radiculopathy, which affects motor as well as sensory roots. Our patient satisfies the diagnostic criteria[4] of CISMP clinically and electrophysiologically. Nerve conduction study of distal nerve segments are usually normal, which distinguishes CISP from the sensory variant of chronic immune demyelinating polyneuropathy (CIDP). CISMP is similar to CIDP, but it lacks typical electrodiagnostic findings of peripheral nerve demyelination as the affection is predominantly in the roots.[4] This explains the normal conduction studies in the peripheral nerves in our case who later started showing proximal conduction disturbances evidenced by prolonged F wave latencies. Cases of CIDP associated with MCTD have been reported sparsely in literature from India.[6] Subclinical autonomic dysfunctions have been described in association with connective tissue diseases including mixed connective-tissue diseases. Also mild autonomic dysfunction has been reported by Lyu et al. in 25% of their CIDP patients, involving both parasympathetic and sympathetic components.[7] A case series by Sakakibara et al. reported micturitional disturbances in 8 of 32 patients with CIDP (25%) and among those subjects, voiding difficulty or urinary urgency were the main micturitional symptoms.[8] Their findings show that detrusor overactivity may occur in peripheral nerve lesions, with probable pelvic nerve irritation or ephaptic transmission as the cause of bladder dysfunction. CIDP can also produce hypertrophic nerve roots in some patients and present as spinal cord compression syndromes caused by nerve root enlargement or nerve root compression within neural foramina or both, which can account for the bladder symptoms but was ruled out by imaging here.[9], [10], [11] This case assumes a special recognition due to the rare variant of CIDP known as CISMP developing in the background of a connective tissue disease (probable MCTD) along with prominent bladder dysfunction.
Conflict of Interest
The authors declare that there are no conflicts of interest in this paper.
Source of Funding
None.
References
- K Gwathmey. Chronic Inflammatory Demyelinating Polyradiculoneuropathy and Its Variants. Continuum (Minneap Minn) 2020. [Google Scholar] [Crossref]
- R J Barohn, J T Kissel, J R Warmolts, J R Mendell. Chronic inflammatory demyelinating polyradiculoneuropathy. Clinical characteristics, course, and recommendations for diagnostic criteria. Arch Neurol 1989. [Google Scholar]
- F T Rotta, A T Sussman, W G Bradley. The spectrum of chronic inflammatory demyelinating polyneuropathy. J Neurol Sci 2000. [Google Scholar] [Crossref]
- S Khadilkar, B Patel, K A Mansukhani, S Jaggi. Two cases of chronic immune sensorimotor polyradiculopathy: Expanding the spectrum of chronic immune polyradiculopathies. Muscle Nerve 2016. [Google Scholar] [Crossref]
- M Sinnreich, C J Klein, J R Daube, J Engelstad, R J Spinner, P J Dyck. Chronic immune sensory polyradiculopathy: a possibly treatable sensory ataxia. Neurology 2004. [Google Scholar]
- P P Sethi, A Sudan, S Kumari. Case of rare association of peripheral neuropathy with mixed connective tissue disorder. BMJ Case Rep 2021. [Google Scholar] [Crossref]
- R K Lyu, L M Tang, Y R Wu, S T Chen. Cardiovascular autonomic function and sympathetic skin response in chronic inflammatory demyelinating polyradiculoneuropathy. Muscle Nerve 2002. [Google Scholar]
- R Sakakibara, T Hattori, S Kuwabara, T Yamanishi, K Yasuda. Micturitional disturbance in patients with chronic inflammatory demyelinating polyneuropathy. Neurology 1998. [Google Scholar] [Crossref]
- K Ishii, A Tamaoka, Y Fujita, S Shoji. Bladder and bowel dysfunction in chronic inflammatory demyelinating polyradiculoneuropathy. Eur J Intern Med 2005. [Google Scholar]
- A J Duggins, J G Mcleod, J D Pollard, L Davies, F Yang, E O Thompson. Spinal root and plexus hypertrophy in chronic inflammatory demyelinating polyneuropathy. Brain 1999. [Google Scholar]
- E K O'ferrall, D Gendron, M C Guiot, J Hall, M Sinnreich. Lower motor neuron syndrome due to cauda equina hypertrophy with onion bulbs. Muscle Nerve 2013. [Google Scholar]
