Introduction
Numerous case reports, series, and prospective studies of neurological involvement associated with COVID 19 are emerging, from all across the world. Various syndromes; including stroke, encephalopathy, encephalitis, and Guillain-Barré Syndrome (GBS) have been described with SARS-CoV infection.1, 2 Stroke is a multi-factorial condition, with varied risk factors and manifestations. It is of paramount importance to understand the clinical profile and natural history of stroke with COVID19 infection. There is still no consensus statement whether it is a causative effect of the virus or mere co-existence. Mark Ellul and colleagues have discussed this conundrum, based on Hill's criteria.3 Although strength and consistency of association are low; biological plausibility and analogy with other SARS infections suggest an etiological relationship.
Data collection
In Gujarat state (India), COVID19 infection had peaked up from March 2020. Our SVP hospital is a dedicated COVID19 hospital, under government regulation. In all patients, nasopharyngeal swab for RT-PCR was used to confirm COVID19 status.
In a retrospective analysis of hospital records, out of 3908 patients with SARS-CoV infection admitted to our SVP hospital during the last 4 months(Mar to Jun 2020), we identified 7 patients of acute ischemic stroke(AIS). Details from hospital case papers were collected in systemic manner, with focus to: age, gender, clinical deficit, associated co-morbidities, imaging findings, CBC, LFT, RFT, Lipid profile, COVID bio markers (CRP, IL6, D Dimer, Ferrittin levels),and follow up status on discharge. Out of 11 patients we screened, 4 patients were excluded in view of inadequate data or incomplete work up.
Observations
The majority of severe COVID19 infected patients required ventilator support and so sedation, for a prolonged time. It was difficult to detect focal neurological findings in these critically ill patients; hence the precise number of stroke patients and incidence rate was not possible to measure.
Our key observations are: (Table 1)
All patients were more than 50 yrs of age. The mean age was 68.14 years+/- 23. Five patients (71.4%) were male.
All patients of AIS were in the moderate to severe COVID19 category. The government of Gujarat state had defined categories of COVID19 patients, as per ICMR guidelines, based on clinical and radiological findings. 4
Four out of 7 patients developed stroke 7-10 days after onset of COVID19 symptoms (range 2-17 days). Rest of patients had 8-17days interval between onset of COVID-19 symptoms and onset of neurological deficit.
Co-morbidities or preexisting stroke risk factors were found in all of our patients. Diabetes and Hypertension were the most common disorders.
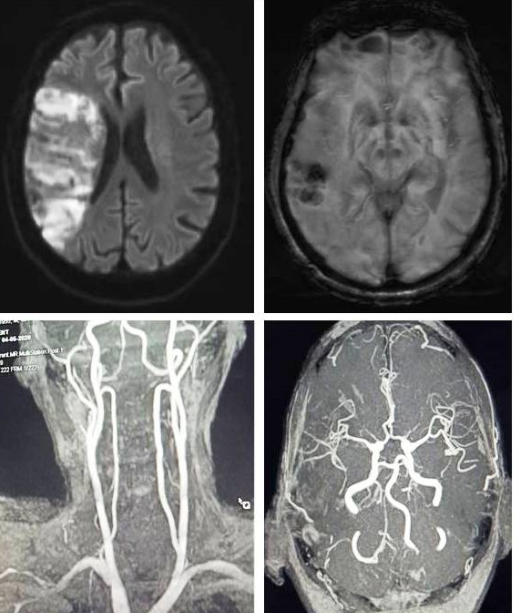
In our case series, 71.4 % (5/7) have large artery ischemic stroke. Out of them, two have more than one arterial territory involvement and two developed hemorrhagic transformations.(Figure 1)
5 out of 7 patients had elevated levels of commonly used biomarkers of prothrombotic state, i.e.; D-Dimer. In our cohort, one or more marker (CRP, IL6, D Dimer, Ferritin) was found elevated in all of the patients.
Prognosis of stroke patients with COVID19 was poor; 3 out of our 7 pt died within the hospitalization period and the rest had a severe residual disability on discharge. Patients were given antiplatelet and statin therapy; with standard stroke protocol care. None of the patients was thrombolysed and heparin (unfractionated or low molecular weight) was given as per COVID19 protocol.4
Table 1
Profile of ischemic stroke in COVID19 patients
Discussion
Though many case series and prospective research during the pandemic has shown high number of association with Ischemic stroke, in the hospitalized patients, the exact number is difficult to define; hence incidence and prevalence rates may not be calculated. Out of 3908 patients screened, only 7 were documented to have acute Ischemic stroke, giving incidence of <0.01%. Many of the severe COVID-19 patients had respiratory insufficiency and was put on mechanical ventilation support, with or without sedation. Minor neurological deficit or cognitive dysfunction might have gone unrecognized in those patients. This findings was in contrast to other studies, stating high incidence (0.9% to 2.7%) of AIS in COVID-19 hospitalized patients.5 In the early phase of pandemic, all patients including minor symptoms were admitted to our centre; so we presume our data is close to actual population incidence rather than incidence in severely affected patients only.
An elderly male of Asian origin was considered to be a traditionally high-risk population for ischemic stroke. Mean age is around 70 years and 5 out of 7 were male in our cohort. In a recent meta-analysis of 135 patients of covid19 related AIS, mean age was 63.4+/- 13.1 years and the majority were male patients.4 Data from Wuhan also noted the same; out of that cohort youngest patient of stroke was 55 years of age.2 Disease severity of COVID-19 may play an important role in pathogenesis of AIS. All of our patients had moderate to severe COVID disease category. In the Newyork study by Yaghi et al, 81.3% (26/32) of patients with stroke have met the criteria for severe COIVD19 disease.6 Variation in the incidence rate also can be attributed to different stages of COVID19 severity; showing increased prevalence in severe category.7, 8
Onset of stroke symptoms during the first week of illness may suggest a linear correlation with the inflammatory and cytokine storm stage. Studies have shown elevated levels of various biomarkers of prothrombotic state during 7-14 days of initial symptoms.9, 10
Atherosclerosis related risk factors have been noted in almost all patients.Tan et al also found hypertension and diabetes in 64.5 % and 42.5% respectively, out of 121 AIS patients.5 These findings may point to the "trigger" theory, where the virus may only act as a provocative factor for plaque destabilization in susceptible individuals with compromised vasculature. Large areas of parenchyma involvement has been co-confirmed in other case series.6 Small vessel ischemic stroke is not common, even in the diabetic and hypertensive individuals. Hemorrhagic transformation was also commonly encountered in AIS in COVID19 patients.11 In a binary regression analysis model by Yaghi et al, AIS in COVID19 patients have higher peak D –Dimer levels, as compared to contemporary controls.6 Elevated inflammatory markers, such as ESR, CRP, Ferritin, and IL6 were also found in various case series. It may help to understand the pathophysiology and judicious use of anti-inflammatory and antithrombotic therapy at a proper time window.
Severe COVID19 and associated large or multiple territory infarcts put these patients at high risk. In a pooled analysis by Aggrawal et al, cerebrovascular disease was found to be associated with a statistically significant increased risk of a severe form of COVID-19 (OR: 2.55 (95% CI: 1.18 to 5.51), I2¼29%, Cochran's Q, p¼0.24).[12] Similar results of more severe stroke, higher NIHSS, large vessel occlusion, and higher in-hospital mortality were also reported by Yaghi et al.6
Stroke mechanism in COVID19 may be multifaceted, varying from large vessel thrombosis, embolism, prothrombotic state, coagulopathy, and/or vasculopathy (endothelial dysfunction). Cytokine storm may have an important causative role in the pathogenesis of vascular events, by affecting the thrombotic process, coagulation cascade, or direct injury to endothelial surface of the vessel wall, leading to thrombosis and resultant stroke. Usually, more than one mechanism may operate in an individual patient. Thrombolysis with alteplase and Mechanical thrombectomy has also been used with variable success. The use of anticoagulation medication in therapeutic doses is now standard recommendation. But the prophylactic role in susceptible individuals, particularly elderly males, with severe COVID19 disease and high D-Dimer or inflammatory markers should be a norm.
Limitation
Our study has many obvious limitations. We have gathered data of a very small size population in a retrospective manner. Detailed investigations regarding vascular anatomy and other risk factors of stroke could not be completed in all subjects.
Summary
The number of "identified" stroke patients in COVID19 cohort at our center was relatively less. Hypertensive and diabetic elderly male, who developed moderate to severe COVID19 disease were more common in the ischemic stroke cohort. D-Dimer and inflammatory markers may help to identify a high-risk individual and start therapy at the earliest. Large vessel occlusion is a common finding and mortality is high in AIS patients, during this COVID19 pandemic.
Analogous observation studies in different heterogeneous populations will guide us to understand the disease process better and its therapeutic strategies. The identification of different subsets of patients with known factors may help to individualize treatment plans.