- Visibility 76 Views
- Downloads 31 Downloads
- DOI 10.18231/j.ijn.2021.028
-
CrossMark
- Citation
Multifocal Tuberculosis- an unusual encounter
Introduction
Worldwide, 10 million people fall ill with tuberculosis (TB) each year. India accounts for 27% of the global burden of the TB cases.[1] Tubercular osteomyelitis, a form of extra-pulmonary TB, represents less than 2% of all TB cases and about 10% of all cases of extra-pulmonary TB.[2] Multifocal involvement that occur simultaneously at two or more locations in the skeletal system, is exceptional and constitutes <5% of all skeletal TB cases.[3], [4], [5] Isolated involvement of the posterior elements of the spine is very rare, incidence being 2 to 3 % of patients with spinal TB.[6] Calvarial TB is one of the rare manifestations of TB with an estimated incidence of 1% of all skeletal TB.[5]
In this study, we present a case of atypical disseminated multifocal TB in a non-immunocompromised patient. Unusual radiological images were observed at uncommon sites, which were more compatible with a multifocal osteomyelitis, histiocytosis or metastatic disease rather than an infectious disease. Inspite of widespread involvement, the outcome of the patient was favorable following antitubercular treatment.
Case Report
A 25year old female patient presented with 4 month history of headache and neck pain. She had decreased appetite, weight loss, but no history of chronic cough or fever. The patient’s general physical examination was normal. There was slight tenderness over the right anterior 3rd rib, lower thoracic spine and right sacroiliac joint. No para-spinal swelling or spasms were observed.Neurological examination was also normal. Hematological and biochemical blood tests were within normal limit however erythrocyte sedimentation rate (ESR) was 100 mm/h. In addition, tests for autoantibodies, TB anti-bodies and tumor associated antigens were negative. Human immunodeficiency virus (HIV) and purified protein derivative (PPD) tests were also negative.
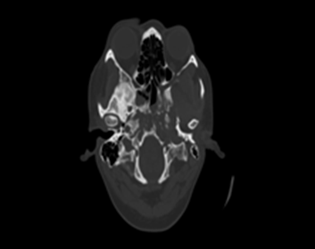
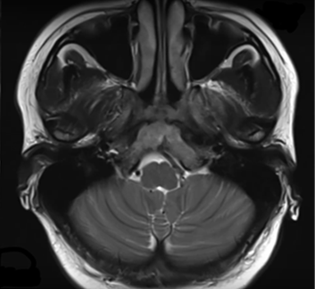
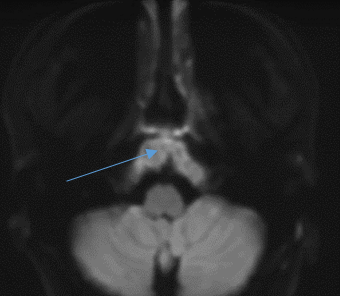
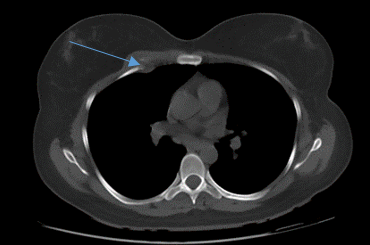
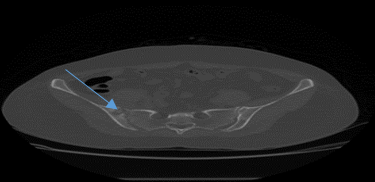
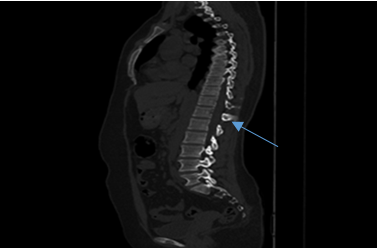
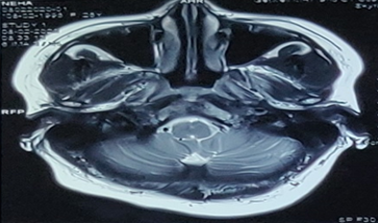
NCCT head showed permeative osteolytic lesions in basi-sphenoid including left pterygoid plates and occipital condyles with no evidence of matrix mineralization ([Figure 1]). MRI brain showed heterogenous altered signal intensity lesions in basisphenoid including left pterygoid plates and occipital condyles with associated mild soft tissue component ([Figure 2]); these also showed diffusion restriction ([Figure 3]), with heterogenous enhancement on post contrast study with multiple areas of peripheral ring enhancement and central necrosis. CT of chest and abdomen showed an expansile lytic lesion involving the right third rib ([Figure 4]) permeative lytic lesion was seen in spinous process of D 11 vertebrae ([Figure 7]), lytic lesions showed a radioluscent rim and central dense sclerotic bone in left pubic bone ([Figure 6]) and right iliac bone consisting with button sequestrum. Erosions and irregularity was seen along the articular aspects of right sacroiliac joint ([Figure 5]) consistent with sacroiliatis. Vertebral bodies and intervertebral discs at the said levels appeared unremarkable. The brain parenchyma was normal, lung fields were clear with no evidence of mediastinal or hilar lymphadenopathy, abdomen showed no obvious lesion in CT.
Based on the history, examination and radiological studies multifocal osteomyelitis, metastatic disease or Histiocytosis were suspected. CT and MRI findings did not allow for a final diagnosis, a CT guided biopsy from the lesion in the right anterior 3rd rib was performed to confirm the diagnosis. It was inconclusive and the result of Acid Fast Bacilli culture was negative; however polymerase chain reaction performed by CBNAAT (cartridge based nucleic acid amplification test) was positive for TB. Based on these observations, a diagnosis of multifocal TB was established. She was treated conservatively and administered antiTB chemotherapy regimen,[2], [5] including isoniazid (300 mg /day), rifampicin (600 mg/day), pyrazinamide (750 mg/day) and ethambutol (750 mg/day). Patient was then discharged from hospital. In the follow up after 3 months, she was clinically better and radiological findings ([Figure 7]) showed improvement and her ESR was 45mm/hr.
Discussion
Multifocal TB and disseminated forms of the disease are usually more frequent in certain patients, such as those with a much older age, malnourished as well as immune-compromised and in particular HIV infected individuals.[7], [8], [9] However, our patient was a healthy 25 years old female with no signs of systemic involvement and a negative HIV status presenting to a neurosurgeon with vague symptoms of headache and neck pain. With wide range of involvement and symptoms the atypical forms of TB are difficult to diagnose.
TB that involves the posterior elements of the spine, particularly in isolation, is considered rare.[10] According to literature, two hypothesis exist explaining this atypical presentation:[5], [11] (I) increased pressure in the body cavities leading to retrograde flow of blood and mycobacterium from a primary focus through the valveless Batson venous plexus located in the epidural space to the vertebral venous plexi, (II) infection of the immunocompromised patients. Lymphatic spread and multidrug-resistent TB are less widely accepted theories for atypical spinal TB.[9]
Calvarium TB is also rare even in areas where TB is endemic and occurs secondary to a primary focus elsewhere.[2] About 50% of patients affected are younger than 10 yrs and 70-90% are younger than 20yrs,[12], [13] as in our case patient was 25yrs old. Various hypothesis have been mentioned for the pathogenesis of calvarial TB including hematogenous seeding of the bacilli to the diploe, trauma and lymphatic dissemination.[14] The common sites of involvement are frontal and parietal followed by occipital and sphenoid bones, which is probably due to greater amount of cancellous bone with diploic channels at these sites.[13] In our case there were lesions in basisphenoid and occipital condyles.
Biopsy or CT guided needle aspiration remain essential for accurate diagnosis and adequate treatment.[15], [16], [17] The advantage of needle aspiration is that it is a less invasive technique; however, only a small number of specimens can be obtained, particularly when the lesions are sclerotic, and thus the diagnosis rate is only 81.0% in children and 91.3% in adults.[18] The CBNAAT (Cartridge based Nucleic acid amplification test) also known as Xpert® MTB/RIF assay (Cepheid Inc.,CA, USA) marks an important development in the field of rapid molecular TB diagnostics. This diagnostic platform is an performs PCR and can be used by operators with minimal technical training, enabling diagnosis of TB and also assessment of rifampicin resistance to be completed as early as 2h.[7] CBNAAT is a robust test for accurate diagnosis of tuberculosis both pulmonary and extra-pulmonary, smear negative as well, especially in resource-limited settings.[19] In our case she was smear negative but CBNAAT positive, and in view of strong clinical suspicion, multidrug anti-TB therapy was advised.
Multidrug anti-TB therapy including Isoniazid, Rifampin, Ethambutol and Pyrazinamide advocated for an approximate duration of 12 to18 months usually leads to complete resolution of TB.[2], [6], [17] The mainstay of treatment of Spinal TB is conservative management with bracing and anti tubercular drugs. Surgery is indicated in cases with neurological deficit or spinal instability.Medical treatment is highly effective when administered appropriately, as performed in the present study.
Conclusion
Extrapulmonary tuberculosis can involve any part of the body. Rare manifestations like Base of Skull involvement illustrates the importance of a detailed physical examination in this cases with vague clinical symptoms and keeping TB in differential diagnosis. Extra-pulmonary tuberculosis should always be ruled out in any patient with multiple round hypodense lytic lesions in any part of the skeletal system including skull base in countries endemic for TB.
Source of Funding
No financial support was received for the work within this manuscript.
Conflicts of Interest
There are no conflicts of interest.
References
- . . . [Google Scholar]
- M Thawani, E Hale, E Habte-Gabr. Multifocal tubercular osteomyelitis: a case with atypical manifestations. Tuberc Res Treat 2011. [Google Scholar] [Crossref]
- MH Yilmaz, F Kantarci, I Mihmanli, K Kanberoglu. Multifocal Skeletal Tuberculosis. South Med J 2004. [Google Scholar] [Crossref]
- A Agarwal, SA Khan, NA Qureshi. Multifocal osteoarticular tuberculosis in children. J Orthop Surg (Hong Kong) 2011. [Google Scholar] [Crossref]
- N Al-Khudairi, A Meir. Isolated tuberculosis of the posterior spinal elements: case report and discussion of management. JRSM Open 2014. [Google Scholar] [Crossref]
- SS Nadavapalli, UR Thota, VR Jampana. Multifocal calvarial tuberculosis: a rare presentation. J Evol Med Dent Sci 2016. [Google Scholar] [Crossref]
- SD Lawn, AI Zumla. Diagnosis of extrapulmonary tuberculosis using the Xpert®MTB/RIF assay. Expert Rev Anti-infective Ther 2012. [Google Scholar] [Crossref]
- A Marudanayagam, J J Gnanadoss. Multifocal skeletal tuberculosis: A report of three cases. Iowa Orthop J 2006. [Google Scholar]
- RK Garg, DS Somvanshi. Spinal tuberculosis: A review. J Spinal Cord Med 2011. [Google Scholar] [Crossref]
- Y Zhang, Y Zhang, J Ma. The prospect of incidental detection of unsuspected skeletal tuberculosis by bone scintigraphy should not be overlooked. Clin Nucl Med 2007. [Google Scholar]
- M Gardam, S Lim. Mycobacterial Osteomyelitis and Arthritis. Infect Dis Clin North Am 2005. [Google Scholar] [Crossref]
- D C Strauss. Tuberculosis of the flat bones of the vault of the skull. Surg Gynaecol Obstet 1933. [Google Scholar]
- CM Meng, YK Wu. Tuberculosis of the flat bones of the vault of the skull: A study of forty cases. JBJS 1942. [Google Scholar]
- HL Rieder, DE Snider, GM Cauthen. Extrapulmonary Tuberculosis in the United States. Am Rev Respir Dis 1990. [Google Scholar] [Crossref]
- F G St Clair Strange. Current concepts review. Tuberculosis of bones and joints (78-A:288-298, Feb. 1996) by Watts and Lifeso. J Bone Joint Surg Am 1996. [Google Scholar]
- SL Moore, M Rafii. Imaging of Musculoskeletal and Spinal Tuberculosis. Radiol Clin North Am 2001. [Google Scholar] [Crossref]
- FC Ringshausen, A Tannapfel, V Nicolas, A Weber, HW Duchna, G Schultze-Werninghaus. A fatal case of spinal tuberculosis mistaken for metastatic lung cancer: recalling ancient Pott's disease. Ann Clin Microbiol Antimicrob 2009. [Google Scholar] [Crossref]
- D Ballah, E Nijs, MS Keller, X Zhu, G Krishnamurthy, AM Cahill. Percutaneous CT-guided vertebral bone biopsy in children. Pediatr Radiol 2013. [Google Scholar] [Crossref]
- A K Prakash, B Datta, J P Tripathy, N Kumar, P Chatterjee, A Jaiswal. The clinical utility of cycle of threshold value of GeneXpert MTB/RIF (CBNAAT) and its diagnostic accuracy in pulmonary and extra-pulmonary samples at a tertiary care center in India. Indian J Tuberc 2007. [Google Scholar]
