- Visibility 46 Views
- Downloads 11 Downloads
- DOI 10.18231/j.ijn.2021.020
-
CrossMark
- Citation
To assess and analyze the clinical outcome of conservative and operative management of head injury in acute subdural haematoma
- Author Details:
-
Deepak Rathor
-
I.D Chaurasia *
Introduction
An Acute Subdural haematoma is a collection of fresh blood under the dura, which may compress the brain. Acute subdural haematoma represents common neurosurgical problem associated with significant morbidity, mortality and high recurrence rates.[1] Subdural haematoma may be acute or chronic, Acute subdural haematoma usually occurs after severe high-impact injuries and is often associated with contusions of the adjacent areas of the brain.[2] Acute subdural haematoma presents within 48-72 hours of injury. If the acute SDH is small (<5 mm in thickness) and the patient is clinically stable, a period of observation may be effective. If conservative management is preferred, careful clinical observation and follow-up radiological imaging are mandatory, because there is potential for the acute SDH to enlarge.[3] Craniotomy to remove the haematoma is preferred if there is significant mass effect with raised Intracranial pressure. During surgery, the haematoma is felt to have a solid, jelly-like consistency.
In some studies, more craniotomies than decompressive craniectomies were performed as a surgical treatment of choice for AcSDH. Primary/ early decompressive craniectomy can provide more effective control of intracranial pressure (ICP) and aggressive brain edema. DAI are commonly associated with Acute SDH, which explains the high mortality in patients with Acute SDH despite appropriate management of Acute SDH. Surgical indications for AcSDH:
Lesion causing raised ICP
Midline shift <75mm
Brain stem compression
Thickness of AcSDH<5mm with midline shift.
Surgery not needed
Patients with good GCS with small AcSDH
Patients with absent brainstem reflexes after resuscitation.
Subdural hematomas are caused more frequently by venous rather than arterial damage and are often self-limiting because of the slow bleeding process. Commonly involved veins are bridging cortical vein near sagittal sinus,[4] veins from sylvian fissure to sphenoparital sinus, the inferior cerebral and deep veins into the transverse and superior petrosal sinus. Notwithstanding if the haematoma is enormous, mass weight impact may occur, moving cerebral structures and causing edema in the parenchyma of the mind bringing about a poor clinical outcome.[5] Moreover, the chance of herniation exists with huge subdural haematomas or with haematomas that keep on amplifying after injury. Intense subdural haematoma emerge profound to the dura yet outer to the arachnoid layer and the untreated haematoma may get subacute or chronic.[6] Intense subdural haematoma is more normal in more seasoned age bunch in light of the fact that the veins are not so much tough but rather more effectively harmed. Patients taking anticoagulants and patients with liquor abuse are likewise inclined to create intense subdural haematoma.
Materials and Methods
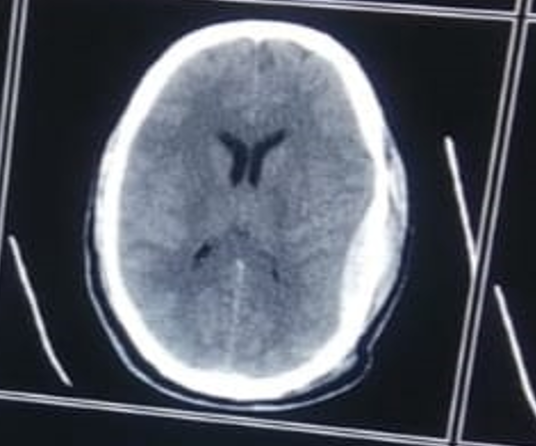
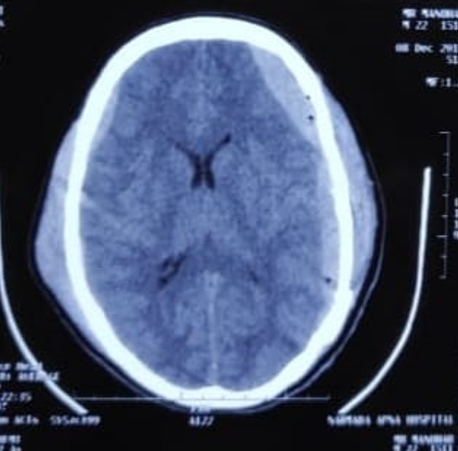
This is a study based in department of surgery in the Neurosurgery unit of Gandhi Medical College, Bhopal. After taking complete history and detailed examination and investigation (CT Scan) was be done. Decision of surgery was be taken by the consultant neurosurgeon of the acute Subdural Haematoma, involvement of aloquent areas and associated other injury of brain.
200 patients with head injury who reported at casualty of Gandhi Medical College, and Hamidia Hospital, Bhopal between period of Nov 2018 to July 2020, was further investigated for CT scan head, which revealed acute SDH were included in the study.
Data about the demographical characteristics such as age & gender, the history & clinical findings such as mechanism of injury, the time duration from the traumatic event until surgical decompression were recorded.
The hemispherical location of the haematoma, the presence of extracranial injury, presence of midline shift at the level of septum pellucidum in CT. systolic and diastolic blood pressure, the pupillary reactivity and the signs of herniation (unilateral or bilateral pupil dilatation) were recorded.
Following the establishment of airway patency and appropriate fluid resuscitation, patients having significant acute SDH in CT were immediately operated for decompression.
Inclusion criteria
Age - Adult > 18 years age and above
Acute Subdural Haematoma any size
Only head injury patient
Traumatic patient involve.
Pupillary asymmetry (any pupillary size)
With or without midline shift
Acute Subdural Haematoma at any site e.g. frontal, parietal, hemispheric.
Exclusion criteria
Age <18 years of age
Chronic Subdural Haematoma
Polytrauma (Severe life threatening musculoskeletal/spine/thoraco- abdominal injury)
Systemic illness, metabolic disorder, endocrine abnormalities & coagulopathy
Evidence of severe brain stem dysfunction
Presence of bradycardia
Patients who are unwilling for inclusion in the study
Results
|
|
|
Conservative |
|
Operative Management |
|
P Value |
|
S. No. |
Age Group |
No. |
Percentage |
No. |
Percentage |
.325111 |
|
1 |
20-35 |
34 |
34 |
26 |
26 |
|
|
2 |
36-50 |
30 |
30 |
42 |
42 |
|
|
3 |
51-65 |
22 |
22 |
18 |
18 |
|
|
4 |
66-85 |
14 |
14 |
14 |
14 |
Maximum cases of patients were in age range 36-50 i.e. 30% & 42% in Conservative & Operative Management respectively.[Table 1]
The chi-square statistic is 3.4667. The p-value is .325111. The result is not statistically significant as p < .05. This indicated that there is no statistically significant correlation between age group of the patient and management protocol in patients of acute SDH.
|
|
|
Conservative |
|
Operative Management |
|
P Value |
|
S. No. |
Mode of Injury |
No. |
Percentage |
No. |
Percentage |
.09177 |
|
1 |
Assault |
20 |
20 |
06 |
06 |
|
|
2 |
Fall |
27 |
27 |
14 |
14 |
|
|
3 |
RTA |
53 |
53 |
80 |
80 |
In our study, Mode of Injury found to be Assault were 20%, Fall were 27% & RTA 53% in Conservative whereas Assault were 06%, Fall were 14% & RTA 80%.[Table 2]
The chi-square statistic is 17.1416. The p-value is .09177. The result is not significant at p < .05. These findings confirmed that the mode of injury doesnot affect the management of the patient of acute SDH.
|
|
MLS |
Conservative |
|
|
Operative Management |
|
P Value |
|
S. No. |
Yes/No |
No. |
Percentage |
Yes/No |
No. |
Percentage |
< .00001 |
|
1 |
N |
87 |
87 |
N |
08 |
08 |
|
|
2 |
Y <5 mm |
13 |
13 |
Y >5 mm |
92 |
92 |
The chi-square statistic is 125.1328. The p-value is < .00001. The result is significant at p < .05.[Table 3]
|
|
|
Conservative |
|
|
Operative Management |
|
|
P Value |
|
S. No. |
Acute SDH Thickness |
No. |
Alive |
Dead |
No. |
Alive |
Dead |
< 0.00001 |
|
1 |
< 5 mm |
62 |
51 |
11 |
07 |
07 |
00 |
|
|
2 |
05-09 mm |
38 |
23 |
15 |
93 |
51 |
42 |
The chi-square statistic is 96.3397. The p-value is < 0.00001. The result is significant at p < 0.05. These findings indicate that the thickness/size of acute SDH significantly correlates with the type of management to be done for the patient.[Table 4]
Discussion
This study was conducted on 200 patients of age group 18 year and above with clinically apparent head injury who reported at casualty of Gandhi Medical College and Hamidia Hospital, Bhopal (M.P.) during the time period extending from November 2018 to July 2020, who were further investigated for CT scan head which revealed acute subdural hematoma were included in the study. The patients who were less than 18 year of age and who were not giving consent were excluded from our study group.
Management of Acute subdural hematoma mostly depends upon detailed examination and CT scan (head) findings of patient. Decision of conservative and operative management in Acute subdural hematoma (Acute SDH) depend upon GCS, midline shift, volume of the SDH, involvement of aloquent area and associated injuries of brain.
The initial management of acute subdural hematoma includes maintenance of airway, maintenance of blood pressure and measures to lower the intracranial pressure [ICP]. The aim of decreasing the intracranial pressure and maintaining the blood pressure is to maintain cerebral perfusion pressure [CPP].[7]
The major indications for the surgical treatment of acute subdural haemotoma are increased intracranial pressure, significant midline shift more than 5 mm and signs of brain stem compression. In general all subdural haematomas that are more than 5 mm thick with midline shift were considered for surgical evacuation. [8] Those patients with absent brain stem reflexes after resuscitation will almost have a poor prognosis and are rarely operative patients.
Also, it is important to repeat the scan within 72 hours of injury as haematomas may enlarge, have more mass effect because of surrounding oedema, new lesions may appear, patients with acute SDH with GCS 3-5 had higher mortality rate and poor prognosis.
Poor prognostic factors:
Patients older than 50 years.
GCS<8
Pupillary abnormalities
Post operatively raised ICP
Delay in diagnosis & operation.
Our study showed good outcome with decompressive craniectomy in patients whose GCS was <8 and were not associated with other intracranial lesions. Our results carry similar selection basis that neurosurgeons tend to perform decompressive craniectomy. When patient’s preoperative clinical status is poor. To clarify this point, we counted on number of unfavorable features for each patient that may influence on poor outcome.
Patients with good Glasgow coma scale [GCS] with small subdural haemotoma did not required surgery and treated conservatively. Age is not among the prognostic factors converting the outcome in acute head injury patients. In our study, maximum cases of acute subdural hematoma patients were in age range 36-50 year i.e. 30% & 42% in conservative and operative management, which is statistically not significant in my study ( P Value = 0.325111). Present study shows similar results in study done by Soubhagya R. Tripathy et al in 2016 [9], that’s shows 46.87% of SASDH patients belonged to the 35 – 54 year age group. In Sachidanand Gautam [10] et al 2018 study, the maximum patients suffering from subdural hematoma were in the age group of 11 – 60 years. Present study shows similar results in conservative patient age group of 20-35 year (34%) and 36-50 year (30%), in operative patient age range 20-35 year (26%) and 36-50 year (42%). However this study is with small patient population. Limitations of selection basis hinder any conclusion on role of decompressive craniectomy for AcSDH. We think furthur investigation with larger patient population and carefully selected criteria is needed to clarify the optimal surgical modality for patient with AcSDH.
Conclusion
Acute subdural haematoma is the major cause of significant morbidity and mortality due to traumatic head injury. Acute subdual haematoma is commonly associated with countercoup injuries and diffuse axonal injury (DAI). The clinical presentation in patients with acute SDH is related to raised ICP and the severity of DAI. C.T. Scan is the investigation of choice in patients with head injury. Early decompression in AcSDH may be of particular benefit. The age of the patients, pupillary size and reaction at the time of admission was statistically significant predictor of outcome. The concept of performing decompressive craniectomy in traumatic AcSDH patients seems to be attractive and beneficeal.
Source of Funding
No financial support was received for the work within this manuscript.
Conflicts of Interest
There are no conflicts of interest.
References
- S Hatashita, N Koga, Y Hosaka, S Takagi. Acute Subdural Hematoma: Severity of Injury, Surgical Intervention, and Mortality. Neurol Med Chir (Tokyo) 1993. [Google Scholar] [Crossref]
- M Zumkeller, R Behrmann, HE Heissler, H Dietz. Computed Tomographic Criteria and Survival Rate for Patients with Acute Subdural Hematoma. Neurosurgery 1996. [Google Scholar] [Crossref]
- R K Koç, H Akdemir, I S Oktem. Acute subdural hematoma: outcome and outcome prediction. Neurosurg Rev 1997. [Google Scholar] [Crossref]
- F Servadei, MT Nasi, AM Cremonini, G Giuliani, P Cenni, A Nanni. Importance of a Reliable Admission Glasgow Coma Scale Score for Determining the Need for Evacuation of Posttraumatic Subdural Hematomas. J Trauma 1998. [Google Scholar] [Crossref]
- TA Gennarelli, GM Spielman, TW Langfitt, PL Gildenberg, T Harrington, JA Jane. Influence of the type of intracranial lesion on outcome from severe head injury. J Neurosurg 1982. [Google Scholar] [Crossref]
- Z Kotwica, J Brzeziński. Acute subdural haematoma in adults: an analysis of outcome in comatose patients. Acta Neurochir (Wien) 1993. [Google Scholar] [Crossref]
- WG Obana, LH Pitts. Extracerebral Lesions. Neurosurg Clin N Am 1991. [Google Scholar] [Crossref]
- SH Meyer, RM Chesnut, GT Tindall, PR Cooper, DL Barrow. Post traumatic Extra-axial mass lesion: subdural and extradural haematoma. The practice of neurosurgery 1996. [Google Scholar]
- SR Tripathy, PK Swarnakar. A review of sub acute subdural hematoma (SASDH) with our institutional experience and its management by double barrel technique (DbT): A novel technique. 2016. [Google Scholar]
- S Gautam, A Sharma, SC Dulara. A clinicoradiological scoring for management of acute subdural hematoma: a prospective study. Rom Neurosurg 2018. [Google Scholar] [Crossref]
