- Visibility 127 Views
- Downloads 35 Downloads
- DOI 10.18231/j.ijn.2020.045
-
CrossMark
- Citation
Idiopathic intracranial hypertension in a case of mycoplasma pneumonia
- Author Details:
-
Mukheem Mudabbir M A
-
Kiran Kumar Ramineni *
-
Viswesvaran Balasubramanian
Introduction
Idiopathic intracranial hypertension (IIH) is one of the treatable causes of headache and vision loss, especially in young females. Risk factors for IIH are female sex, obesity, recent weight gain, hormonal pills usage, steroid withdrawal, thyroid hormone supplementation and vitamin-A intoxication etc.[1] Limited data is available on association of IIH with infections and few reports especially in paediatric age group described mycoplasma infection as one of the triggering factors for the development of IIH.[2], [3]
Case Report
A 28-year-old lady was admitted for the evaluation of the one-month history of fever, cough, myalgias and fatigue. She reported two weeks history of refractory headache localised to the occipital region associated with neck pain. One week before admission she developed double vision predominantly for distant objects, especially on right-sided gaze. Headache, exacerbated with prolonged lying down position, more severe in early hours of mornings with associated nausea and occasional vomitings. No history of head trauma, recent weight gain or similar complaints in the past. She had last childbirth three years back, the peripartum period was uneventful and not on any oral contraceptives. No significant drug intake history except for symptomatic analgesics. Vitals includes a temperature of 100oF, pulse rate of 88 beats per min regular and blood pressure of 110/70mmHg. She was well built with a Body mass index of 24.5 kg/m2 and other general physical examination was unremarkable and chest auscultation revealed left more than right inspiratory crepitations. She was conscious, alert without any neck stiffness or focal deficits. Fundus examination revealed grade-4 papilloedema, Visual acuity: 6/9 bilaterally, right eye abduction restricted with binocular diplopia, had symmetric, normal and reactive pupils. Rest of the neurological examination was normal.
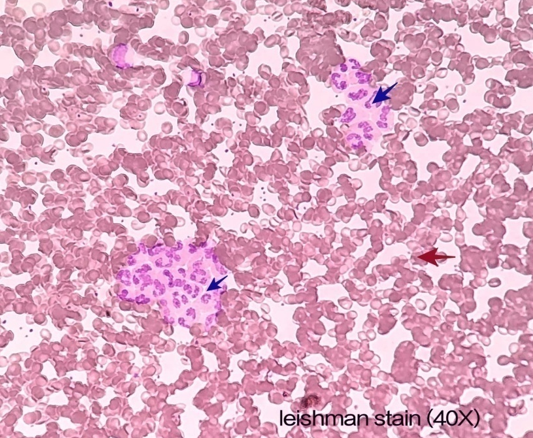
Laboratory investigations revealed haemoglobin of 12gr/dl, total WBC count 5600/microL, platelet count 2.8 lakhs/microL and blood peripheral smear showed leukoagglutination ([Figure 1]). Random blood sugar, serum creatinine, electrolytes, liver function tests, thyroid function tests, serum cortisol and calcium were within normal limits. Serum HIV 1 & 2 non-reactive, Rheumatoid factor and Anti nuclear antibody were negative. Serum mycoplasma IgM antibody was positive. Cardiac evaluation and Ultrasound abdomen did not reveal any significant abnormality.
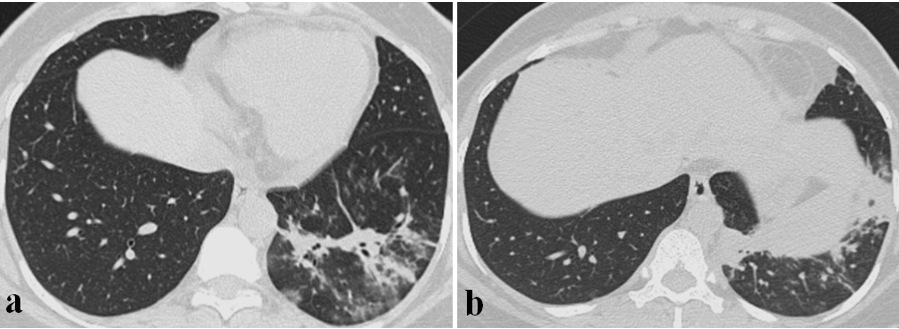
High Resolution Computed Tomography Chest showed left lower lobe patchy consolidation ([Figure 2]a) and basal fibrotic changes ([Figure 2]b). Broncho Alveolar Lavage (BAL) done and was positive for mycoplasma antigen by Polymerase Chain Reaction (PCR).
Magnetic Resonance Imaging of brain plain and contrast with MR-Venogram revealed features of raised intracranial pressure like tortuosity of optic nerves, enlarged subarachnoid space around optic nerves, flattened posterior globe, intra-ocular protrusion of optic nerve heads ([Figure 3]a), and partially empty sella ([Figure 3]b). There was no evidence for venous thrombosis or significant stenosis ([Figure 3]c), no evidence of contrast enhancement or cerebral oedema ([Figure 3]d). Lumbar puncture confirmed grossly elevated opening pressure of 310 mm of H2O and routine CSF biochemical analysis and cell count were within normal limits. CSF was negative for gram stain, bacterial culture as well as fungal culture and Mycobacterium tuberculosis PCR.
She was managed with two weeks course of intravenous antibiotics including Ceftriaxone & Clarithromycin and with gradually titrated dosage of intravenous mannitol followed by oral acetazolamide. She showed steady improvement in her headache and double vision, fever subsided and was discharged on day fifteen in a stable condition with specific advice to follow the course of titrating dose of oral acetazolamide and advised for lifestyle modification to prevent weight gain in future. At six weeks follow up she was asymptomatic with normal extraocular movements and visual acuity as well as resolving papilledema. No adverse drug reactions were noted. However she did not turn up for further follow-ups.

Discussion
Idiopathic intracranial hypertension (IIH), also known as Pseudo tumour cerebri syndrome (PTCS) indicates an unexplained increase in intracranial pressure and is a diagnosis of exclusion. Young and obese females are usually affected. Initial presentation includes headache more so in early hours of the morning along with transient visual obscuration, diplopia and/or pulsatile tinnitus. It may result in permanent vision loss, if not detected and managed in time.
Neurological examination is routinely unremarkable except for the presence of papilledema and restriction of extraocular movements with abducens palsy.[1], [4] Although precise pathogenesis of IIH remains unknown various proposed mechanisms include cerebral venous outflow abnormalities with venous hypertension, increased cerebrospinal fluid outflow resistance, obesity-related increased intra-abdominal and intracranial venous pressure, distorted sodium and water retention and abnormal vitamin-A metabolism etc. [5] Association with infectious agents are extremely rare and often symptoms overlap with features of meningitis. Mycoplasma pneumoniae is implicated in some of the atypical pneumonias and neurological complications are known to occur in approximately 10% of these patients including encephalitis, acute disseminated encephalomyelitis, Guillain-Barre Syndrome sometimes resulting in permanent residual deficits. [6], [7] However association with IIH is extremely rare with only a few reports describing mycoplasma infection as one of the triggers for IIH, especially in paediatric age group.[3] Our report highlights one such association in a young lady without any significant past medical, drug intake history and co-morbidities. Combination of classical clinical features, supportive magnetic resonance imaging of brain findings and normal CSF findings except for grossly elevated opening pressure made the diagnosis of IIH very obvious. Given the preceding symptoms of respiratory tract infection, thorough etiological workup for the possible coexisting infective etiology including BAL was done which helped in the final diagnosis of underlying mycoplasma pneumonia. The additional supportive diagnostic feature was the presence of leuko-agglutination which is well described in mycoplasma infections. [8] As the neurological symptoms started before the initiation of treatment for pneumonia and avoidance of specific medications like quinolones and tetracyclines in this patient makes the possibility of previously described drug-induced IIH extremely unlikely. [9] Her respiratory, neurological symptoms and signs improved after starting appropriate antibiotics and antiedema measures to reduce intracranial pressure as per recommendations. [10] This temporal relationship of mycoplasma pneumoniae pneumonia followed by the development of raised intracranial pressure features and exclusion of the possible alternative etiologies hence support to the hypothesis that mycoplasma infection might have triggered IIH. However further larger studies are needed to prove such definite etiological relationship.
Conclusion
Idiopathic Intracranial Hypertension should be suspected in all young patients presenting with new-onset headache with visual symptoms. Possible differentials can be excluded with judicious utilization of brain imaging and laboratory services. Thorough evaluation for the co-occurring illness based on clinical symptoms like mycoplasma pneumonia in this report helps in the appropriate management and a better outcome.
Source of Funding
None.
Conflict of Interest
None.
References
- M Wall. Idiopathic Intracranial Hypertension. Neurol Clin 2010. [Google Scholar]
- A M Gorostidi, M Iridoy Zulet, G Azcona Ganuza, E Gembero Esarte, M E Yoldi Petri, S Aguilera Albesa. Seudotumor cerebri enniños: etiología, característicasclínicas y evolución. Neurología 2019. [Google Scholar]
- S Masutani, R Takayama, T Tsugawa, K Nikaido, T Doi, H Tsutsumi. Intracranial Hypertension in a Boy with Mycoplasma pneumoniae Infection: The First Report. Scand J Infect Dis 2004. [Google Scholar]
- J Hoffmann, S P Mollan, K Paemeleire, C Lampl, R H Jensen, A J Sinclair. European Headache Federation guideline on idiopathic intracranial hypertension. J Headache Pain 2018. [Google Scholar]
- V Biousse, B B Bruce, N J Newman. Update on the pathophysiology and management of idiopathic intracranial hypertension. J Neurol, Neurosurg Psychiatry 2012. [Google Scholar]
- M Narita. Pathogenesis of neurologic manifestations of Mycoplasma pneumoniae infection. Pediatr Neurol 2009. [Google Scholar]
- J Kammer, S Ziesing, L Davila, E Bültmann, S Illsinger, A Das. Neurological Manifestations of Mycoplasma pneumoniae Infection in Hospitalized Children and Their Long-Term Follow-Up. Neuropediatrics 2016. [Google Scholar]
- Y Kubota, Y Hirakawa, K Wakayama, S Kimura. Peculiar cold-induced leukoagglutination in Mycoplasma pneumoniae pneumonia. Turkish J Hematol 2017. [Google Scholar]
- L Maffeis, R Dilena, S Guez, F Menni, C Bana, S Osnaghi. Pseudotumour cerebri associated with mycoplasma pneumoniae infection and treatment with levofloxacin: a case report. BMC Pediatr 2019. [Google Scholar]
- S P Mollan, K A Markey, J D Benzimra, A Jacks, T D Matthews, M A Burdon. A practical approach to, diagnosis, assessment and management of idiopathic intracranial hypertension. Pract Neurol 2014. [Google Scholar]
How to Cite This Article
Vancouver
A MMM, Ramineni KK, Balasubramanian V. Idiopathic intracranial hypertension in a case of mycoplasma pneumonia [Internet]. IP Indian J Neurosci. 2020 [cited 2025 Sep 11];6(3):236-238. Available from: https://doi.org/10.18231/j.ijn.2020.045
APA
A, M. M. M., Ramineni, K. K., Balasubramanian, V. (2020). Idiopathic intracranial hypertension in a case of mycoplasma pneumonia. IP Indian J Neurosci, 6(3), 236-238. https://doi.org/10.18231/j.ijn.2020.045
MLA
A, Mukheem Mudabbir M, Ramineni, Kiran Kumar, Balasubramanian, Viswesvaran. "Idiopathic intracranial hypertension in a case of mycoplasma pneumonia." IP Indian J Neurosci, vol. 6, no. 3, 2020, pp. 236-238. https://doi.org/10.18231/j.ijn.2020.045
Chicago
A, M. M. M., Ramineni, K. K., Balasubramanian, V.. "Idiopathic intracranial hypertension in a case of mycoplasma pneumonia." IP Indian J Neurosci 6, no. 3 (2020): 236-238. https://doi.org/10.18231/j.ijn.2020.045
