Introduction
Trigeminal neuralgia (TN) is defined as sudden, severe, brief, stabbing and recurrent pain within the distribution of one or more branches of the trigeminal nerve.1 Microvascular decompression (MVD) is a well-accepted and highly effective surgical technique in trigeminal neuralgia (TN). But some times microscope may fail to detect the compressing vessel at the root entry zone or distally especially when the suprameatal tubercle is prominent and when culprit vessel is lying anterior to nerve.2 To avoid these disadvantages, MVD technique has been enhanced over the years by the integration with the endoscope in the so‑called endoscopic microvascular decompression.2, 3, 4
Frequently drilling of the prominent suprameatal tubercle, dissection of the cerebellar fissure and the supracerebellar route could be required to permit identification and dissection of neurovascular conflict (NVC) in such patients.5 Such additional procedures of drilling of bone and fissure dissection could be avoided when endoscope is used i.e. EMVD (endoscopic microvascular decompression). Endoscope ascertains some advantages in TN, such as improved visualization of entire course of trigeminal nerve and vascular culprits, which could be missed in significant percentage of patients by microscope use only. Improved visualization without brain retraction is a major advantage of endoscopic surgery.6 The endoscope also helps in better delineation of completeness of decompression. The endoscope can be used solely for the whole procedure or as an additional help to the microscope in TN.7, 8, 9, 10
Though literature is available on the above mentioned procedures regarding their efficacy in TN, but scarce literature is available on the comparison between the two techniques. Hence the present study was conducted to compare as well as evaluate microscopic vascular decompression and endoscopic vascular decompression for trigeminal neuralgia.
Materials and Methods
The present study was conducted in Department of Neurosurgery at SMS Medical College during November 2018-December 2019 among the patients with the diagnosis of medically refractory trigeminal neuralgia. Patients were seen in the neurosurgery OPD for preoperative evaluation. The ethics committee of our institute approved this study. Written consent was taken from all the patients. Thirty three patients were recruited for the study, out of which 22, and 11 underwent MVD and EMVD respectively. The decision to perform a microscopic procedure and purely endoscopic procedure was based on the comfort of the surgeon as well as the availability of equipment. Pre operative parameters like age, gender, chief complaints, duration of symptom, side and number of involved branches were recorded. The work described has been carried out in accordance with The Code of Ethics of the World Medical Association.
Surgical Technique
Patients with trigeminal neuralgia were managed by surgical exploration using a standard retrosigmoid approach. Patients were placed in the lateral decubitus or supine position with their head tilted as far away as the mobility of their neck permitted. Under general endotracheal anesthesia, a 1- to 2-cm retrosigmoid craniectomy was made just inferior to the junction of the transverse and sigmoid sinuses. The dura was opened and reflected against the sinus. With standard microneurosurgical techniques, the trigeminal nerve was identified by gently retracting the cerebellum, releasing cerebrospinal fluid from the basal cisterns, and lysing the arachnoidal bands. After the nerve was explored as thoroughly as possible with the microscope, a handheld 30-degree rigid endoscope was placed into the cerebellopontine angle to enhance the surgeon’s view.
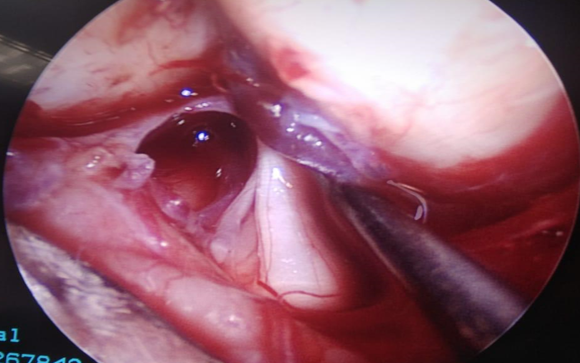
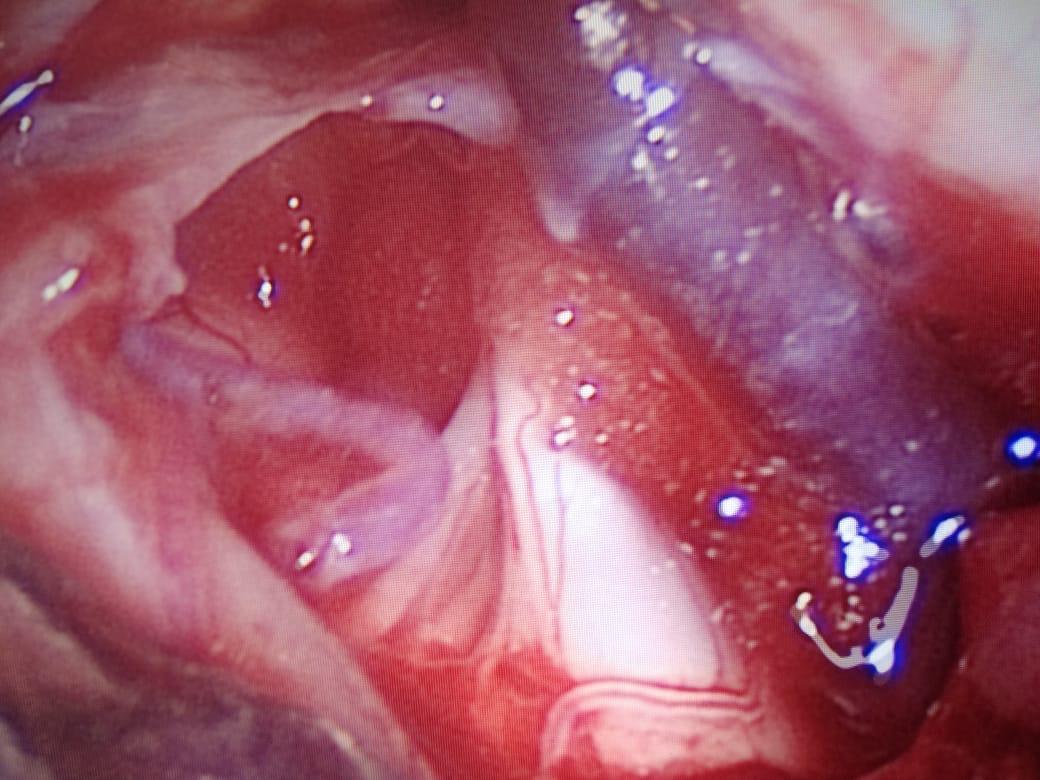
The endoscope was advanced in a straight line toward the trigeminal nerve, keeping the shaft of the endoscope stabilized against the edge of the craniotomy or the venous sinus. The endoscope was rotated to the degree that the surgeon’s wrist allowed to inspect the root entry zone. By aiming the 30-degree endoscope laterally, medially, superiorly, or inferiorly, a comprehensive view of the entire trigeminal nerve was obtained (Figure 1). To obtain each view, the endoscope was adjusted by rotating the rod lens and camera to keep the image upright and the vector of the view ideal. If the compressing vessel was seen better or only with the endoscope, it was noted and MVD was performed under endoscopic control. (Figure 2).
MVD was achieved by placing a small Gelfoam patch securely between the root entry zone of the nerve and the offending vessel. When possible, the patch was folded in half under tension so that it pushed the vessel away from the nerve. During endoscopic MVD, the endoscope was carefully introduced into the posterior fossa alongside a small blunt suction or a small dissector which was maintained ahead of the endoscope so that it remains in view at all times, avoiding possible unseen collisions with delicate neurovascular structures. Drainage of cerebrospinal fluid normally made it possible to operate for brief periods without the aid of suction in the non-dominant hand. With endoscope in non dominant hand, one-handed dissection and manipulation were performed as well as the patch placement with the operating instrument in the dominant hand. Adequacy of decompression was confirmed by endoscope and noted. Closure was completed by standard techniques, including watertight dural closure, whenever possible.
Outcomes Recorded
Patients were followed up at one and three months post-surgery. Outcomes were categorized into four groups: excellent (patients had no pain, were on no medication, and had no persistent side effects), good (patients had no pain, but experienced minor [nondisabling] surgical complications), fair (pain was well controlled with medication), and poor (patients had persistent neuralgia or no pain, but persistent debilitating side effects). Various complications and degree of reduction of symptoms were also recorded.
Statistical analysis
Data so collected was tabulated in an excel sheet, under the guidance of statistician. The means and standard deviations of the measurements per group were used for statistical analysis (SPSS 22.00 for windows; SPSS inc, Chicago, USA). Difference between two groups was determined using chi square test and the level of significance was set at p < 0.05.
Results
In the present study, 45.45% and 72.73% of the subjects were male in MVD and EMVD group respectively. The mean age of the subjects was 52.55 years in MVD group while in EMVD group, the mean age was 56.55 years (Table 1).
Pain on right side was reported more in both MVD and EMVD group. The mean duration of symptoms was 38.11 and 39.62 months in MVD and EMVD group respectively (Table 2).
Excellent outcome was reported among 81.82% of the subjects in EMVD while it was found only in 59.09% of the subjects in MVD group. Poor outcome was revealed only in 4.55% of the subjects in MVD group. When outcomes were compared statistically among MVD and EMVD group, it was found to be statistically insignificant as p>0.05 (Table 3).
Table 1
Demographic characteristics among the study groups
|
Groups |
Male |
Female |
Age (in years) |
|||
|
N |
% |
N |
% |
Mean |
SD |
|
|
MVD (N=22) |
10 |
45.45 |
12 |
54.55 |
52.55 |
14.35 |
|
EMVD (N=11) |
8 |
72.73 |
3 |
27.27 |
56.55 |
8.78 |
Discussion
Endoscopy is commonly used in skull base, spine, and cranial surgery. It is also useful for various types of pathologies such as congenital lesions, hematomas evacuation, tumor excisions, and infective pathologies.11, 12, 13
Endoscopic techniques for TN were found to be safe in our study; other authors made similar observations. The endoscopic procedure was very effective with good outcome rate in our study, as other authors have also observed.14, 15 In the present study, excellent outcome was reported among 81.82% of the subjects in EMVD while it was found only in 59.09% of the subjects in MVD group. Poor outcome was revealed only in 4.55% of the subjects in MVD group.
Casey H. Halpern et al 16 in their study revealed that fully endoscopic MVD supports the safety, feasibility, and potential benefits of this approach for a wide variety of neurovascular syndromes. Although they neither demonstrate superiority of the fully endoscopic approach nor find any statistically significant difference when compared to the microscopic procedure. It is important to note that no difference was found despite the relatively short period of time following introduction of the endoscope into routine practice. Hence, they believe that the use of the endoscope is safe for microvascular decompression, and at least as effective as a microscopic procedure.
There was no mortality in our series; similar observations were made in other reported series as well.17 The use of the endoscope in the posterior fossa, however, offers additional benefits to skull base surgeons. Once the surgeon becomes accustomed to the technique of operating with the endoscope using the view from the monitor, it opens up the possibility of operating with angled scopes, which may allow safe access to structures not previously seen using the standard operative microscope. We believe that extended retrosigmoid approaches to more difficult areas of the brain will become more likely.16
The present study sample is small and also short follow-up period. It is too early to determine the effect that the addition of endoscopy will have on long-term clinical outcomes in larger series. In our preliminary experience, however, endoscopy was a valuable adjunct both when adequate decompression was thought to have been performed and when no compression was visible with the microscope alone as was seen in 2 of the cases in our series. Therefore, it should be considered a useful adjunct in all cases, regardless of whether a compressive vessel is identified during microscopic exploration.
Conclusion
It can be concluded from the results of present study that endoscopic microvascular decompression is a safe, feasible and effective procedure for cure of TGN. Our experience summarizes the transition from conventional microscopic surgery to a fully endoscopic procedure, demonstrating the ease and safety of incorporating this tool into practice as a solo instrument. Expanding this experience from neurovascular syndromes to cerebellopontine angle tumors represents the next step in the expanding era of minimally invasive endoscopic neurosurgery.