Introduction
Corona viruses (CoV) are enveloped non-segmented RNA viruses belongs to the family Coronaviridae.1 In December 2019, corona virus disease (covid-19) epidemic occurred in Wuhan, China and has rapidly spread to other part of world and it became pandemic. The novel CoV 2019, is 7th known CoV that can infect humans; the remaining are HCoV-229E, HCoV-OC43, HCoV-NL63, HCoV-HKU1, SARS-CoV, and MERS-CoV.2 Past two epidemics of corona virus were due to severe acute respiratory syndrome coronavirus (SARS- CoV) and Middle East respiratory syndrome coronavirus (MERS-CoV) with mortality rate of 10% and 37% respectively. 3, 4
Novel CoV 2019 is reported to have almost similar symptoms as seen in SARS-CoV 2003. Both viruses attacks shared angiotensin-converting enzyme 2 (ACE2) receptor.5 Until 31 May 2020 there were around 59 lacs confirmed cases with 4 lacs deaths in world. Covid 19 known to mainly involves respiratory system but now there are emerging evidences regarding various neurological manifestations in the form of headache, anosmia, dysguesia, impaired consciousness, seizures, stroke and vascular events, encephalitis, myositis and acute inflammatory demyelinating polyneuropathy. So, our aim is to review and analyze the extent of COVID 19 propensity to damage different level of neuraxis.
Materials and Methods
Search strategy
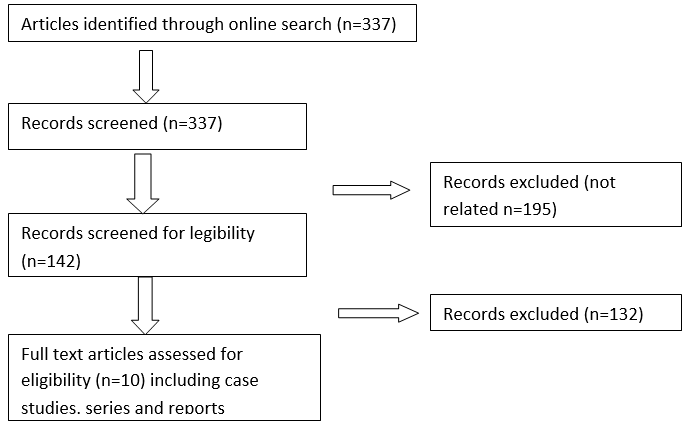
The major online database was searched upto May 2020 to collect all related published articles. Following key words were used COVID 19, novel corona virus, SARS COV -2, neurological, brain, CNS and neuroinvasion. After the initial search, references from the relevant articles were included. Search strategy showed in Flow chart. There were no language restrictions. Authors independently assessed each article that was considered for inclusion in study. Exclusion criteria were non human studies, incomplete or non extractable data. Demographic data including sample size, study types and year of study were extracted.
Flow diagram of study method
Results
Studies Focusing on neurological manifestations of COVID-19 are very few. These studies are summarized in Table 1.
Study 1 included 214 patients out of them 36.4% patients had neurological involvement 6. Study 2 done in Italy included 88 patients of them 33.9% reported at least one taste or olfactory disorder and 18.6% both. 7 Study 3 was retrospective study investigated acute cerebrovascular disease following covid 19. 8 Study by Chen et al9 on 99 patients reported non specific symptoms of headache and confusion. One case report was also included reporting necrotizing encephalitis after COVID-19. 10
Table 1
Discussion
Out of seven corona virus which can infect humans three virus SARS-CoV,MERS-CoV and SARS-CoV2) are associated with neurological complications.
SARS-CoV patients may presents as polyneuropathy, encephalitis, and aortic ischemic stroke. 12 Cerebral oedema and meningeal vasodilation leads to symptoms of encephalitis and infiltraton of mononuclear cells in vessel wall leads to ischemia of brain and peripheral nerves. 13
MERS-CoVis also neuroinvasive about 20% patients of MERS-CoV had neurological involvement 14
Evidence of primarily fatality and morbidity directly due to lung involvement, but expansion of abnormality in neurological system related was not reviewed in depth till date. Hypercoagulable state in covid 19 leads to vascular events ans associated with mortality in these patients. DIC property of the virus itself associated with endothelial dysfunction ,activation of complement cascade and antiphospholipid syndrome have been described in possible mechanism of hypercoagulable state.
Our analysis of study, case series and case reports showed nervous system may involve directly or indirectly by COVID-19.
SARS-CoV-2 has genetical similarity with SARS-CoV.15 Patients of covid 19 has symptoms ranging from mild fever, cough to multi organ involvement with mortality of 2-3%.
Some patients presented with non-specific symptoms dizziness, headache and confusion. Some patients had specific neurological involvement i.e. stroke, encephalitis, seizure and myositis
Most common finding in all analysis was olfactory nerve involvement (5-33%). Hypoguesia and hyposmia was seen commonly. Olfactory nerve in nasal epithelium is important pathway for spread of infection to CNS. 16 Olfactory route of CNS invasion favour study by Andrea Giacomelli et al 7 in Italy, in their study they found that 33.9% patients had smell and taste disturbance. one case report by Thomas laurendon et al 17 patient had complete anosmia and dysgeusia MRI of that patient showed bilateral olfactory bulb oedema
Only case reports are available regarding encephalitis in covid 19 patients. A case of acute necrotizing encephalitis has been reported 10 which was due to immune mediated response.MRI brain showed involvement of medial temporal lobe, insular region and bilateral thalamus.
Another case of encephalitis was reported from japan that was CSF positive for SARS-COV-2 and MRI finding suggestive of involvement of temporal lobe and hippocampus. 18
Activation of glial cells leads to release of interleukin-6 which cause immune mediated neuronal damage.19 Early anti- inflammatory immune modulator therapy may prevent immune mediated nervous system injury in critically ill patients.
Patients of Covid- 19 may presents with impaired consciousness that may be due to metabolic or toxic derangement like sepsis, severe inflammation, electrolytes disturbances, hypoglycaemia, liver and renal impairment. 20 Diffuse alveolar injury in corona virus infection leads to hypoxic injury in brain and shift to anerobic metabolism in brains mitochondria. That leads to interstitial edema, obstruction of cerebral blood flow manifest as various neurological signs and symptoms. 21
Yanan li et al 8 in their study of 221 patients in Italy reported Ischemic stroke 5%,cerebral hemorrhage 0.5% and CVT 0.5% patients. They noticed that cerebrovascular disease had statistically significant correlation with older age, hypertension, diabetes, past history of stroke and in addition of raised CRP and D-dimer.Corona virus can damage blood brain barrier by binding to ACE2 receptor present on capillary endothelium and can enter to CNS. Interaction with ACE2 receptor increase risk of stroke.22 There are recently discussed building of hypothesis regarding risk of vascular events in COVID 19 and how neuroinvesion by novel corona virus play role in cerebrovascular events,outline suggesations related to the management of stroke in COVID 19 pandemic. 23
Only few cases of GBS are reported in COVID 19 patients. Molecular mimicry play role in pathogenesis of GBS in COVID 19 patients. In Italy 2 patients of AIDP, 24 3 patients of AMAN24 and one patient of miller fisher variant of GBS was reported. 25 Headache is nonspecific but commonly reported symptom in COVID 19 patients. Pathogenesis of headache is less clearly none, cytokine and chemokines are thought to play important role. Mao L et al 6 and Chen et al 11 reported 13.1% and 8% cases respectively in their study. Till now only few studies focusing on neurological involvement in COVID 19 are available.
Further studies targeting on neurological symptoms and signs, detail investigation including isolation of virus from CSF required to know extant of neurological involvement and to identify optimal management strategy.
Conclusions
Corona virus infection primarily affects respiratory system but neurological involvement is also frequently observed and associated with poor outcome
Common neurological manifestations were related to olfactory and taste disturbance followed by encephalopathy, vascular events and GBS.
Each COVID19 patients should be evaluated for neurological involvement clinically followed by investigations (electrophysiology, brain imaging, CSF analysis for noval corona virus) as needed. Since this is a new emerging on going pandemic disease so more changes are expected in future and needs good evidence based studies, So that early treatment of complications can improve outcome.