Introduction
Spondylolisthesis is a common cause of low back pain, radiculopathy, and neurogenic claudication among the adult population. Translated from Greek, spondylolisthesis literally means “slipping of the spine”. Degenerative spondylolisthesis was first described by Newman in 1955 and other types were described later.1, 2 The most commonly affected level of the spine in degenerative spondylolisthesis is L4-L5 with women affected five to six times more than men,and black women are affected three times more than white women.3
Non-operative treatments include non-steroidal anti-inflammatory drugs with or without narcotics,lumbosacral epidural injections, physical therapy and flexion-based exercise protocols. Surgery is usually considered if there is no improvement of function or pain relief after a minimum conservative trial of three months, or if there is a progression of neurologic deficit or development of cauda equina syndrome. Dynamic instability on radiologic assessment is also considered for surgery.
The surgical management of degenerative lumbarspondylolisthesis associated with spinal canal stenosis has evolved throughout the past several decades.Early surgery of laminectomy (decompression) paid little importance to the instability related to the vertebral slippage. In patients who had decompressive laminectomy with preservation of a majority of facet joints, the outcome was dramatically better. The best outcome occurred in those patients who had undergone a decompressive laminectomy combined with a posterolateral intertransverse process arthrodesis.4
In this study, we have attempted to compare the pre-operative intensity of pain and functional limitations with corresponding values at six months postoperative follow up using self-administered questionnaire.5
Materials and Methods
This prospective non-randomized study was conducted in patients with degenerative spondylolisthesis attending Neurosurgery outpatient Department of a tertiary care centre at Bangalore. The patientswere enrolled for surgery to be followed up postoperatively using self-administered questionnaire, over a period of three years. Approval from an institutional ethics committee was taken before the study. Data from 56 (fifty-six) patients were collected and analyzed over this period tocompare the degree of pre-operative pain and functional disability with corresponding values at 6(six) months postoperatively.
Patients with degenerative spondylolisthesis and symptomatic spinal canal stenosis who had undergone non-operative treatment for at least 3(three) months before the surgery were included in the study. Patients who had a prior history of lumbar spinesurgery, osteoporotic changes in the lumbosacral CTscan and back pain due to other pathologies were excluded from the study.
The pre-operative and post-operative parameter was assessed by using a self-administeredquestionnaire ( Table 1, Table 2, Table 3 ) developed by Stucki et al.5 Some modifications were made by rating the pain in the backand lower limbs/ buttock using visual analogue scale(VAS) ranging from 0(no pain) to 10(severe pain).6
Table 1
Component items of symptoms severity scale.
Table 2
Component items of the physical function scale.
Table 3
Component items of the satisfaction scale (after 6 months of follow-up)
Table 4
Demographic profile and Co-morbidity status
(continuous data are expressed as mean±standard deviation (S.D) and categorical data(s) are expressed as ratios; n=56).
Table 5
Shows the percentage of spondylolisthesis, VAS and degree of disability pre-operative and post-operative;
Table 6
Post-operative complications
| Parameters | Nos. | Percentage (%) |
| Infection | 1 | 1.9% |
| Deep vein thrombosis (DVT) | 1 | 1.9% |
| Cauda equina syndrome | 1 | 1.9% |
The percentage of spondylolisthesis was assessed preoperatively by radiological method.7
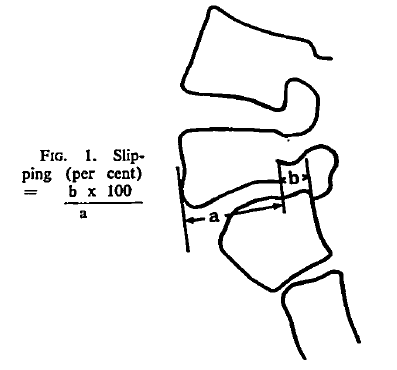
Slippage of spondylolisthesis (Percent) = b 100/a
The degree of spondylolisthesis is classified depending on the displacement of the vertebral bodywidth8 : Grade = 0to 25%; Grade 2=25 to 50%; Grade 3= 50-75% and Grade 4 = 75 to 100%.
After obtaining written informed consent, the operation was performed using midline linear incision in the lower lumbar region to expose the posterior elements of the spine from one level above to one level below the proposed level of fusion. The surgical procedure included lumbar decompression (laminectomy) and transpedicular instrumentation by pedicle screws,rods and autologous iliac crest bone graft.
The pre-operative and postoperative (at 6 months) data(s) were followed up clinically and radiologically and analyzed using SPSS version 15.0(SPSS Inc, Chicago IL). Student’s t-test (two-tailed, dependent) wasused and a ‘p’value less than 0.05 was considered significant.
Results
This study was conducted in 56 patients of degenerative spondylolisthesis requiring surgery to compare the preoperative and postoperative pain and disability. The demographic profile of the patients is shown in Table 4 . All the patients turned up for postoperative assessment at 6 months.
(continuous data are expressed as mean±standard deviation (S.D) and categorical data(s) are expressed as ratios; n=56).
Out of the fifty-six patients, three patients (5.4%) had pseudoarthrosis and the rest (94.6%) had bony fusion. Patients in the bony fusion group had complications like infection (one patient), deep vein thrombosis (one patient) and cauda equina syndrome in another patient (Table 6 ).
Discussion
The results of our study have shown that the degree of spondylolisthesis, pain and disability are markedly reduced postoperatively with minimal complications. There was no incidence of implant failure through 3(three) patients (5.4%) developed pseudoarthrosis without bony fusion. Some early studies9, 10 have indicated that fusion status does not affect early clinical outcome.
A fibrous union appears to provide sufficient stabilization and pain relief of the back and lower extremities. In a prospectiverandomized study comparing decompressive laminectomy and arthrodesis with and without spinal instrumentation, Fischgrund et al11 noted that pseudoarthrosis developed in 55% of the non-instrumental group,but the clinical outcome was still good or excellent in 83% of the patients. However, instrumentation has been recommended to increase the fusion rate, decrease the rehabilitation time and improve patient outcome.12, 13, 14, 15 In the current study, the fusion mass was evaluated using plain radiograph. The overall results of bony fusion and pseudoarthrosis (94.6% and 5.4%) in our study seem better than that of Mardjetko et al16 (86% and 14%) and Booth et al (85% and 15%).17 However, our sample size is too small to claim any superiority, and one16 of them involves a meta-analysis.
In this study, all patients had significant post-operative pain relief compared to the preoperative period. The classic presentation of lumbar spondylolisthesis with canal stenosis is that of bilateral neurogenic claudication as well as intermittent pain radiating to the thigh or leg, or bothwhich is worse with prolonged standing, activity or lumbar extension, and this pain is relieved by sitting, lying down, or lumbar flexion.18 In patients with spondylolisthesis and canal stenosis of the L4-L5 segment, the L5 nerve root is usually affected. In case of severe stenosis, the L4 root may also be affected. L4 radiculopathy usually causes pain that radiates in the lateral thigh across the tibial tubercle area and extends down the medial portion of the leg. An L5 radiculopathy usually causes pain and numbness that radiates from the posterolateral thigh to the lateral portion of the leg and onto the dorsum of the foot. The maximum number of patients in this study involved L4-5 and L5-S1 levels.
The degree of disabilitieswas also significantly reduced postoperatively. Though statistically significant improvement can be shown, our results fall short of others,13 who had followed up the patients for 3(three) years and could demonstrate the ability to walk in 83% patients who had an instrumental fusion.
Limitation of the study
Lateral flexion-extension of the lumbosacral spine should be obtained to demonstrate the sagittal motion at the location of the spondylolisthesis. However, due to resource constraints, only neutral erect x-ray of the lumbosacral spine was included in the study.
The outcome of the pseudoarthrosis cases deteriorate over time. But as the mean duration of follow up was only 6(six) months, these aspects could not be ascertained in the study.