- Visibility 75 Views
- Downloads 42 Downloads
- Permissions
- DOI 10.18231/j.ijn.2021.046
-
CrossMark
- Citation
Non-ketotic hyperglycemia presenting as acute hemiparkinsonism
- Author Details:
-
Nagabushan Hesarur
-
Saji K John
-
Thomas Mathew *
Abstract
Non-ketotic hyperglycaemia is commonly associated with hyperkinetic movement disorders like chorea. Here we report a case of non-ketotic hyperglycaemia, in a 70 year old man with longstanding diabetes presenting as acute onset hemi-parkinsonism. Hypokinetic movement disorders are only rarely reported in non-ketotic hyperglycaemia.
Introduction
Acute Parkinsonism occurs due to a variety of non-degenerative causes, which on most occasions are reversible. Most common aetiologies include drugs, structural lesions like strokes, toxin exposure and infections like toxoplasma.[1] Here we report a case of acute hemiparkinsonism caused by hyperglycemia in a diabetic patient.
C ase Report
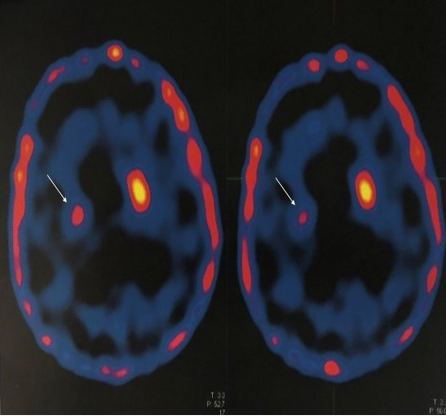
A 70-year-old man, a known diabetic for 30 years presented with acute onset of walking difficulty and slowness of movements of left upper and lower limb. He was suspected to have stroke but the MRI Brain did not reveal any features of acute stroke. He was diagnosed as Parkinson’s disease based on the PET scan finding of hypometabolism involving right putamen ([Figure 1]). He was started on Syndopa 125 mg (Leveodopa 100 mg + carbidopa 25mg) thrice a day for his parkinsonism, but there was no benefit with the medication. He had come for a second opinion after one month of his disease onset. On reviewing the history, the extrapyramidal symptoms were acute in onset. The symptoms started over hours, reached a nadir at 24 hours and improved slightly over one month. His neurological examination revealed mask facies, rigidity, bradykinesia and reduced arm swing on the left side but there was no tremor.
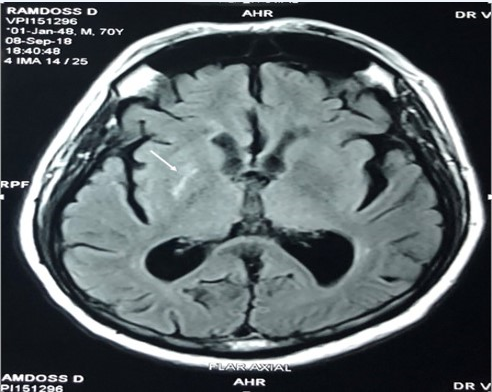
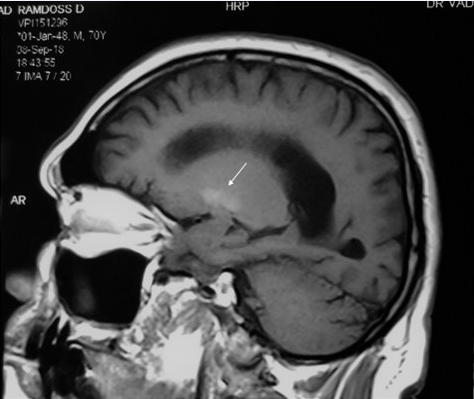
His blood sugar level at the time of onset of symptoms was 400mg/dl with an HbA1c of 11%. His urine ketones were negative. His MRI Brain revealed right putaminal hyperintensity on FLAIR ([Figure 2]) and T1W images ([Figure 3]) with no diffusion restriction. A diagnosis of hemiparkinsonsim due to non ketotic hyperglycemia was made. He was advised intensive glycaemic control and Syndopa was withdrawn. His parkinsonian symptoms improved slowly over months and at 12 months follow up his left sided bradykinesia and rigidity had improved significantly.
Discussion
Hyperglycemia causing hyperkinetic movement disorders like hemiballismus and hemichorea is a well-recognized entity.[2] However, hypokinetic movement disorders like acute hemiparkinsonism secondary to hyperglycemia is rarely seen and reported. The lack of awareness of this entity led to a mistaken diagnosis of Parkinson’s disease in our patient. The findings of PET scan showing hypometabolism in the putamen also misled the physician. Physicians should be aware that a PET scan reveals only a hypofunction of the basal ganglia and does not point to the exact etiology. The etiological diagnosis must be reached based on detailed history including the type of onset, drug exposure, investigations including blood glucose, calcium, MRI Brain and in some cases genetic studies. Hsu et al reported a case of hyperglycemia having clumsiness and unsteadiness without any involuntary movements and characteristic signal changes in basal ganglia on MRI.[3] The exact pathogenesis of hyperglycemia-induced basal ganglia injury is not known. Although glucose is the sole energy source for the brain, its utilization at the cellular level remains elusive. Increased glucose metabolism is seen in substantia nigra pars reticulata and globus pallidus externa of Parkinson's disease patients.[4] Metabolic derangement, vascular insufficiency, hyperviscosity, and vasogenic edema may play a role in basal ganglia cell injury.[3] In these patients, proper functioning of the basal ganglia cells may be compromised by chronic ischemia due to microangiopathic changes without the development of an infarct. [5] When a stage of the metabolic crisis is reached, either because there is a further compromise of circulation or glucose dysmetabolism, the clinical syndrome begins. Basal ganglia injury causes reactive astrocytosis and manganese deposition producing the typical signal changes on MRI.[6]
Acute hemiparkinsonism is a rare entity and prompt identification of the cause and early initiation of treatment may result in a good prognosis. Before initiating the long-term antiparkinsonian medications, one should look for reversible causes. Amongst them, hyperglycemia appears to be an unrecognised cause and all patients presenting with acute hemiparkinsonism should also be evaluated for hyperglycemia. The prompt treatment of hyperglycemia may help in improving the parkinsonian features.
Conflict of Interest
The authors declare that there are no conflicts of interest in this paper.
Source of Funding
None.
References
- Fernandez HH, Friedman JH. Acute Parkinsonism. Current Clinical Neurology: Movement Disorder Emergencies: Diagnosis and Treatment. . 2013. [Google Scholar] [Crossref]
- Roy AK, Raghunandan N, Sarma, Mathew T. A case series of hemichorea due to nonketotic hyperglycemia with MRI brain finding. J Neurol Neurophysiol. 2013. [Google Scholar] [Crossref]
- Hsu JL, Wang HC, Hsu WC. Hyperglycemia induced unilateral basal ganglion lesions with and without hemichorea A PET Study. J Neurol. 2004;251(12):1486-90. [Google Scholar] [Crossref]
- Yamada K. Glucose metabolism in the basal ganglia. Brain Nerve. 2009;61(4):381-8. [Google Scholar]
- Ziegler D, Langen KJ, Herzog H, Kuwert T, Muhlen H, Feinendegen LE. Cerebral glucose metabolism in type 1 diabetic patients. Diabet Med. 1994;11(2):205-9. [Google Scholar] [Crossref]
- Fujioka M, Taoka T, Matsuo Y, Mishima K, Ogoshi K, Kondo Y. Magnetic resonance imaging shows delayed ischemic striatal neurodegeneration. Ann Neurol. 2003;54(6):732-47. [Google Scholar] [Crossref]
How to Cite This Article
Vancouver
Hesarur N, John SK, Mathew T. Non-ketotic hyperglycemia presenting as acute hemiparkinsonism [Internet]. IP Indian J Neurosci. 2021 [cited 2025 Sep 21];7(3):254-256. Available from: https://doi.org/10.18231/j.ijn.2021.046
APA
Hesarur, N., John, S. K., Mathew, T. (2021). Non-ketotic hyperglycemia presenting as acute hemiparkinsonism. IP Indian J Neurosci, 7(3), 254-256. https://doi.org/10.18231/j.ijn.2021.046
MLA
Hesarur, Nagabushan, John, Saji K, Mathew, Thomas. "Non-ketotic hyperglycemia presenting as acute hemiparkinsonism." IP Indian J Neurosci, vol. 7, no. 3, 2021, pp. 254-256. https://doi.org/10.18231/j.ijn.2021.046
Chicago
Hesarur, N., John, S. K., Mathew, T.. "Non-ketotic hyperglycemia presenting as acute hemiparkinsonism." IP Indian J Neurosci 7, no. 3 (2021): 254-256. https://doi.org/10.18231/j.ijn.2021.046
